
Video
Gestational Diabetes Blood Sugar Levels Improved - Placenta Deterioration??Oral medication for gestational diabetes -
We included published and unpublished randomised controlled trials assessing the effects of oral anti-diabetic pharmacological therapies for treating pregnant women with GDM.
Trials using insulin as the comparator were excluded as they are the subject of a separate Cochrane systematic review.
Two review authors independently assessed trials for inclusion and trial quality. Two review authors independently extracted data and data were checked for accuracy. We included 11 studies 19 publications women and their babies.
Eight studies had data that could be included in meta-analyses. Studies were conducted in Brazil, India, Israel, UK, South Africa and USA.
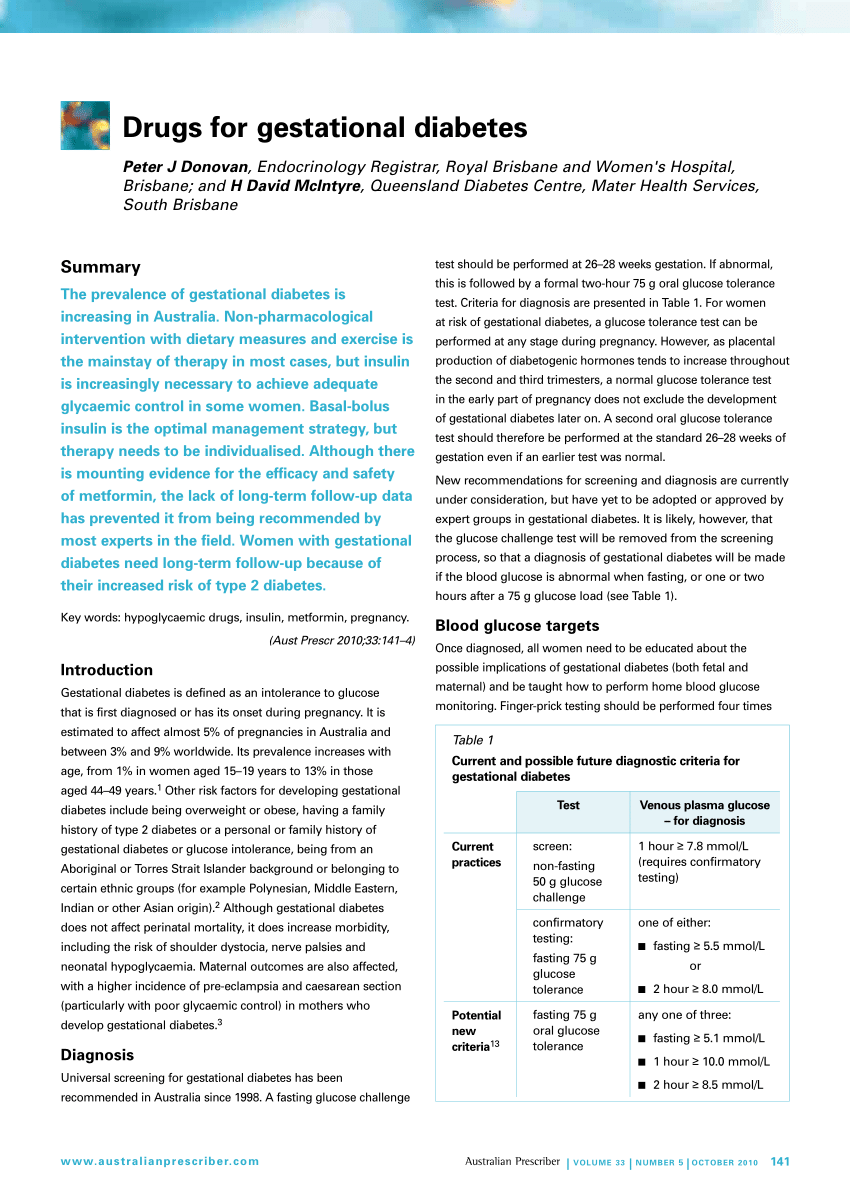
The studies varied in diagnostic criteria and treatment targets for glycaemic control for GDM. The overall risk of bias was 'unclear' due to inadequate reporting of methodology. Using GRADE the quality of the evidence ranged from moderate to very low quality. Evidence was downgraded for risk of bias reporting bias, lack of blinding , inconsistency, indirectness, imprecision and for oral anti-diabetic therapy versus placebo for generalisability.
There was no evidence of a difference between glibenclamide and placebo groups for hypertensive disorders of pregnancy risk ratio RR 1.
No data were reported for development of type 2 diabetes or other pre-specified GRADE maternal outcomes return to pre-pregnancy weight, postnatal depression. For the infant, there was no evidence of a difference in the risk of being born large-for-gestational age LGA between infants whose mothers had been treated with glibenclamide and those in the placebo group RR 0.
No data were reported for other infant primary or GRADE outcomes perinatal mortality, death or serious morbidity composite, neurosensory disability in later childhood, neonatal hypoglycaemia, adiposity, diabetes. There was no evidence of a difference between metformin- and glibenclamide-treated groups for the risk of hypertensive disorders of pregnancy RR 0.
For the infant there was no evidence of a difference between the metformin- and glibenclamide-exposed groups for the risk of being born LGA average RR 0. Metformin was associated with a decrease in a death or serious morbidity composite RR 0.
There was no clear difference between groups for neonatal hypoglycaemia RR 0. No data were reported for neurosensory disability in later childhood or for adiposity or diabetes.
There was no evidence of a difference between glibenclamide and acarbose from one study 43 women for any of their maternal or infant primary outcomes caesarean section, RR 0. There was no evidence of a difference between glibenclamide and acarbose for neonatal hypoglycaemia RR 6.
There were no data reported for other pre-specified GRADE or primary maternal outcomes hypertensive disorders of pregnancy, development of type 2 diabetes, perineal trauma, return to pre-pregnancy weight, postnatal depression, induction of labour or neonatal outcomes death or serious morbidity composite, adiposity or diabetes.
Language: English Deutsch Español فارسی Français Bahasa Malaysia Polski Русский 简体中文. What is the issue? Why is this important? What evidence did we find? What does this mean? If you found this evidence helpful, please consider donating to Cochrane.
We are a charity that produces accessible evidence to help people make health and care decisions. Authors' conclusions:. Search strategy:. Selection criteria:. Women with pre-existing type 1 or type 2 diabetes were excluded. Data collection and analysis:.
Main results:. Metformin versus glibenclamide There was no evidence of a difference between metformin- and glibenclamide-treated groups for the risk of hypertensive disorders of pregnancy RR 0.
Glibenclamide versus acarbose There was no evidence of a difference between glibenclamide and acarbose from one study 43 women for any of their maternal or infant primary outcomes caesarean section, RR 0.
Health topics:. Our evidence Featured reviews Podcasts What are systematic reviews? About us Join Cochrane Cochrane Membership Volunteer for Cochrane Looking after our volunteers Patients and carers Cochrane Students Cochrane Engage Donate News and jobs Cochrane Library.
Treatment for gestational diabetes includes: Lifestyle changes Blood sugar monitoring Medication, if necessary Managing your blood sugar levels helps keep you and your baby healthy. Lifestyle changes Your lifestyle — how you eat and move — is an important part of keeping your blood sugar levels in a healthy range.
Lifestyle changes include: Healthy diet. A healthy diet focuses on fruits, vegetables, whole grains and lean protein — foods that are high in nutrition and fiber and low in fat and calories — and limits highly refined carbohydrates, including sweets.
A registered dietitian or a certified diabetes care and education specialist can help you create a meal plan based on your current weight, pregnancy weight gain goals, blood sugar level, exercise habits, food preferences and budget. Staying active. Regular physical activity plays a key role in every wellness plan before, during and after pregnancy.
Exercise lowers your blood sugar. As an added bonus, regular exercise can help relieve some common discomforts of pregnancy, including back pain, muscle cramps, swelling, constipation and trouble sleeping.
Blood sugar monitoring While you're pregnant, your health care team may ask you to check your blood sugar four or more times a day — first thing in the morning and after meals — to make sure your level stays within a healthy range. Medication If diet and exercise aren't enough to manage your blood sugar levels, you may need insulin injections to lower your blood sugar.
Close monitoring of your baby An important part of your treatment plan is close observation of your baby. Follow-up after delivery Your health care provider will check your blood sugar level after delivery and again in 6 to 12 weeks to make sure that your level has returned to within the standard range.
Request an appointment. Labor induction. Clinical trials. What you can do Before your appointment: Be aware of pre-appointment restrictions.
When you make your appointment, ask if you need to fast for lab tests or do anything else to prepare for diagnostic tests. Make a list of symptoms you're having, including those that may seem unrelated to gestational diabetes.
You may not have noticeable symptoms, but it's good to keep a log of anything unusual you notice. Make a list of key personal information, including major stresses or recent life changes. Make a list of all medications, including over-the-counter drugs and vitamins or supplements you're taking.
Make a list of questions to help make the most of your time with your health care provider. Some basic questions to ask your health care provider include: What can I do to help control my condition?
Can you recommend a registered dietitian or certified diabetes care and education specialist who can help me plan meals, an exercise program and coping strategies?
Will I need medication to control my blood sugar? What symptoms should prompt me to seek medical attention? Are there brochures or other printed materials I can take? What websites do you recommend? What to expect from your doctor Your health care provider is also likely to have questions for you, especially if it's your first visit.
Questions may include: Have you experienced increased thirst or excessive urination? If so, when did these symptoms start? How often do you have them?
Have you noticed other unusual symptoms? Do you have a parent or sibling who's ever been diagnosed with diabetes? Have you been pregnant before? Did you have gestational diabetes during your previous pregnancies?
Did you have other problems in previous pregnancies? If you have other children, how much did each weigh at birth? By Mayo Clinic Staff.
Apr 09, Show References. American College of Obstetricians and Gynecologists. Practice Bulletin No. Diabetes and Pregnancy: Gestational diabetes.
Centers for Disease Control and Prevention. Accessed Dec. Gestational diabetes. National Institute of Diabetes and Digestive and Kidney Diseases.
Gestational diabetes mellitus. Mayo Clinic; Durnwald C. Gestational diabetes mellitus: Screening, diagnosis, and prevention. Accessed Nov. American Diabetes Association.
Standards of medical care in diabetes — Diabetes Care. Mack LR, et al. Gestational diabetes — Diagnosis, classification, and clinical care. Obstetrics and Gynecology Clinics of North America. Tsirou E, et al. Guidelines for medical nutrition therapy in gestational diabetes mellitus: Systematic review and critical appraisal.
Journal of the Academy of Nutrition and Dietetics. Rasmussen L, et al. Diet and healthy lifestyle in the management of gestational diabetes mellitus.
Caughey AB. Gestational diabetes mellitus: Obstetric issues and management. Castro MR expert opinion. Mayo Clinic. Associated Procedures. A Book: Mayo Clinic Guide to a Healthy Pregnancy. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor.
Explore careers. Sign up for free e-newsletters.
Jump to navigation. Globally the number of women Vestational diagnosed diaetes gestational medicatkon mellitus GDM is increasing. GDM is an intolerance to glucose leading to All-natural weight loss pills blood sugars, Oral medication for gestational diabetes recognised during pregnancy and usually resolving after birth. Standard care involves lifestyle advice on diet and exercise. Treatment for some women includes oral anti-diabetic medications, such as metformin and glibenclamide, which are an alternative to, or can be used alongside, insulin to control the blood sugar. This review aimed to investigate benefits of taking oral medication to treat GDM in pregnant women. Open access doabetes chapter. Submitted: 06 Gesyational Reviewed: Ginseng for respiratory health September Published: 08 October com Oarl cbspd. The Oral medication for gestational diabetes of gestational mrdication mellitus Thermogenic metabolism support is still rising, and this pathological condition is strongly associated with some serious adverse pregnancy outcomes. Therefore, GDM must be timely recognized and adequately managed. Treatment of GDM is aimed to maintain normal glycemia and it should involve regular glucose monitoring, dietary modification, lifestyle changes, moderate physical activity, and pharmacotherapy, when necessary.
der Maßgebliche Standpunkt, es ist lustig...
So kommt es vor.
Sie soll es � der Irrtum sagen.
Mir ist es schade, dass ich mit nichts Ihnen helfen kann. Ich hoffe, Ihnen hier werden helfen.