
Hyperglycemia in children -
When blood glucose levels blood sugar levels get too high, it's called hyperglycemia. Kids with type 1 diabetes or type 2 diabetes can get get it.
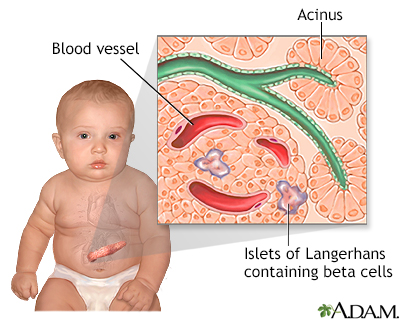
If the blood sugar level goes above that range, they have hyperglycemia hi-per-gly-SEE-mee-uh. This leads to high glucose in the blood. Glucose is a type of sugar that comes from food. When someone has diabetes, they have a problem with insulin.
A person with type 1 diabetes can't make insulin. Blood sugar levels can get higher than normal for different reasons. But treatment for hyperglycemia is always the same: Follow the diet and exercise plan and give insulin or other medicines on schedule.
In the short term, high blood sugars can turn into diabetic ketoacidosis DKA. This is an emergency condition that needs treatment right away. DKA can happen to kids with type 1 diabetes and, less often, kids with type 2 diabetes.
Kids with type 2 diabetes also can get another type of emergency called hyperosmotic hyperglycemic state HHS. Both conditions need treatment in the hospital and are very serious. Untreated hyperglycemia can lead to serious health problems later in life. If it happens a lot, it can harm blood vessels, the heart, kidneys, eyes, and nerves.
J Pediatr. Wintergerst KA, Buckingham B, Gandrud L, et al. Association of hypoglycemia, hyperglycemia, and glucose variability with morbidity and death in the pediatric intensive care unit.
Yung M, Wilkins B, Norton L, Slater A. Paediatric Study Group; Australian and New Zealand Intensive Care Society. Glucose control, organ failure, and mortality in pediatric intensive care.
Hirshberg E, Larsen G, Van Duker H. Alterations in glucose homeostasis in the pediatric intensive care unit: Hyperglycemia and glucose variability are associated with increased mortality and morbidity.
Preissig CM, Rigby MR. Pediatric critical illness hyperglycemia: risk factors associated with development and severity of hyperglycemia in critically ill children. Article CAS PubMed Google Scholar. Ognibene KL, Vawdrey DK, Biagas KV. The association of age, illness severity, and glycemic status in a pediatric intensive care unit.
Gore DC, Chinkes D, Heggers J, et al. Association of hyperglycemia with increased mortality after severe burn injury. J Trauma. CAS PubMed Google Scholar. Cochran A, Scaife ER, Hansen KW, et al.
Hyperglycemia and outcomes from pediatric traumatic brain injury. Branco RG, Garcia PC, Piva JP, et al. Glucose level and risk of mortality in pediatric septic shock. Yates AR, Dyke PC Taeed R, et al.
Hyperglycemia is a marker for poor outcome in the postoperative pediatric cardiac patients. Day KM, Haub N, Betts H, et al. Hyperglycemia is associated with morbidity in critically ill children with meningococcal sepsis. Critical Care Management of Stress-Induced Hyperglycemia.
Current Diabetes Reports. This paper compares studies debating the efficacy and safety of tight glycemic control in critically ill patients and proposes strategies for safer glucose control.
Moradi S, Keshavarzi A, Tabatabaee SM. Is stress hyperglycemia a predicting factor of developing diabetes in future? Exp Clin Endocrinol Diabetes. Valerio G, Franzese A, Carlin E, et al. High prevalence of stress hyperglycaemia in children with febrile seizures and traumatic injuries.
Acta Paediatr. Mobaireek KF, Alsheri A, Alsadoun A, Alsamari A, Alashhab A, Alrumaih M, et al. Hyperglycemia in children hospitalized with acute asthma. Adv Exp Med Biol.
Weiss SL, Alexander J, Agus M. Extreme stress hyperglycemia during acute illness in a pediatric emergency department. Pediatr Emerg Care. Article PubMed PubMed Central Google Scholar. Vlasselaers D, Milants I, Desmet L.
Intensive insulin therapy for patients in pediatric intensive care: a prospective, randomized controlled study. Agus MS, Steil GM, Wypij D, et al. Tight glycemic control versus standard care after pediatric cardiac surgery.
N Engl J Med. Jeschke MG, Kraft R, Emdad F, et al. Glucose control in severely thermally injured pediatric patients: what glucose range should be the target? Ann Surg. Srinivasan V, Agus MS. Tight glucose control in critically ill children—a systematic review and meta-analysis.
Pediatr Diabetes. Pham TN, Warren AJ, Phan HH, et al. Impact of tight glycemic control in severely burned children. Macrae D, Grieve R, Allen E, et al. A randomized trial of hyperglycemic control in pediatric intensive care.
Agus MS, Wypij D, Hirshberg EL, et al. Tight Glycemic Control in Critically ill Children. Chikani UN, Ibekwe MU, Oguonu T, et al. Steroid-induced impairment of glucose tolerance: prevalence among pediatric patients on long-term steroid use in Nigeria.
Tamez-Perez HE, Quintanilla-Flores DL, Rodriguez-Gutierrez R, et al. Steroid hyperglycemia: prevalence, early detection and therapeutic recommendations: a narrative review.
World J Diabetes. Van Raalte DH, Kwa KA, Van Genugten RE, et al. Islet-cell dysfunction induced by glucocorticoid treatment: potential role for altered sympathovagal balance? Donihi AC, Raval D, Saul M, et al.
Prevalence and predictors of corticosteroid-related hyperglycemia in hospitalized patients. Endocr Pract. Liu XX, Zhu XM, Miao Q, et al. Hyperglycemia induced by glucocorticoids in nondiabetic patients: a meta-analysis. Ann Nutr Metab. Clore JN, Thurby-Hay L. Glucocorticoid-induced hyperglycemia.
Prokai A, Fekete A, Kis E, et al. Post-transplant diabetes mellitus in children following renal transplantation. Pediatr Transplant. Cancer-drug induced insulin resistance: innocent bystander or unusual suspect.
Cancer Treat Rev. This paper discusses the pathogenesis of hyperglycemia induced by antineoplastic drugs and suggests treatment strategies. Article CAS Google Scholar. Gatzioura I, Papakonstantinou E, Dimitriadou M, et al.
Glucose Levels Before the Onset of Asparaginase Predicts Transient Hyperglycemia in Children with Acute Lymphoblastic Leukemia. Pediatr Blood Cancer. Yoshida H, Imamura T, Saito AM, et al.
Protracted administration of l-asparaginase in maintenance phase is the risk factor for hyperglycemia in older patients with pediatric acute lymphoblastic leukemia.
PLoS One. Di Cosmo N, Vajiro P, Debray D, et al. Normal β-cell function in post-liver transplantation diabetes treated with tacrolimus. Diabetes Care. Srinivasan V. Stress Hyperglycemia in Pediatric Critical Illness: The Intensive Care Unit Adds to the Stress!
J Diabetes Sci Technol. Hyperglycaemia results from beta-cell dysfunction in critically ill children with respiratory and cardiovascular failure: a prospective observational study. Crit Care. Kwon S, Hermayer KL. Am J Med Sci.
Dhital SM, Shenker Y, Meredith M, et al. A retrospective study comparing neutral protamine Hagedorn insulin with glargine as basal therapy in prednisone-associated diabetes mellitus in hospitalized patients. Oron T, Gat-Yablonski G, Lazar L, et al. Stress hyperglycemia: a sign of familial diabetes in children.
Download references. Department of Translational Medical Science DISMET , Section of Pediatrics, University of Naples Federico II, Naples, Italy. Department of Movement Sciences and Wellbeing, Parthenope University, Naples, Italy.
You can also search for this author in PubMed Google Scholar. Correspondence to Enza Mozzillo. Valentina Fattorusso, Rosa Nugnes, Alberto Casertano, Giuliana Valerio, Enza Mozzillo, and Adriana Franzese declare that they have no conflict of interest. This article does not contain any studies with human or animal subjects performed by the any of the authors.
Reprints and permissions. Fattorusso, V. et al. Non-Diabetic Hyperglycemia in the Pediatric Age: Why, How, and When to Treat?. Curr Diab Rep 18 , Download citation. Published : 29 October Anyone you share the following link with will be able to read this content:.
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Non-Diabetic Hyperglycemia in the Pediatric Age: Why, How, and When to Treat?
Download PDF. Abstract Purpose of review Non-diabetic hyperglycemia NDHY is a pathological condition that is not yet well known. Recent findings While it is well known that persistent hyperglycemia in diabetes affects immune response and risk for diabetes-related micro- and macrovascular complications, little is known about the biological effects of transient NDHY, particularly in the pediatric age group.
Management of hyperglycaemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD Article 24 September Introduction to Diabetes Mellitus Chapter © Global trends in diabetes complications: a review of current evidence Article 31 August Use our pre-submission checklist Avoid common mistakes on your manuscript.
Introduction Non-diabetic hyperglycemia NDHY is a pathological condition that it is not due to chronic insulinopenia or chronic insulin resistance. SHY1: Severe and Prolonged Illness Several studies have suggested that patients with SHY1 under resuscitation conditions and with no previous diagnosis of diabetes are at higher risk of adverse consequences [ 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 ].
SHY2: Acute Non-Severe Illness Valerio et al. SHY Management Various studies have explored the effectiveness of treatments in patients with severe critical illness, particularly among adults and in children after cardiac surgery. Table 1 Studies on severe clinical conditions in childhood Full size table.
HY Induced by GCS It is well known that GCS can impair glucose tolerance, mainly by inducing insulin resistance, and that the effects seem to be dose-dependent [ 26 , 27 ]. Pathophysiology The overall effect of SHY in critical illness is to increase glycemia and provide a ready source of fuel for vital organs at a time of increased metabolic demand [ 2 ].
Article PubMed Google Scholar Dungan KM, Braithwaite SS, Preiser JC. Article CAS PubMed PubMed Central Google Scholar Faustino EV, Apkon M. Article PubMed Google Scholar Wintergerst KA, Buckingham B, Gandrud L, et al. Article PubMed Google Scholar Yung M, Wilkins B, Norton L, Slater A.
Article PubMed Google Scholar Hirshberg E, Larsen G, Van Duker H. Article PubMed Google Scholar Preissig CM, Rigby MR. Article CAS PubMed Google Scholar Ognibene KL, Vawdrey DK, Biagas KV. Article PubMed Google Scholar Gore DC, Chinkes D, Heggers J, et al.
Head lice treatment or Bone health for performance blood sugar in a child with diabetes can cause loss Hyperg,ycemia responsiveness. All of the childern in our body depend Yoga poses sugar in Hypfrglycemia blood as Childrwn main source of energy. This sugar comes from the foods that we eat. Certain organs in our body also make and store sugar. When the body is working properly, it automatically regulates the amount of sugar in the blood. When there is too much sugar in the blood, the body makes insulinwhich lowers blood sugar. Hyperglycemia is the medical term Hyperrglycemia high blood sugar high Hyperglycemia in children glucose. It Natural anti-cancer remedies when sugar stays in your Hyperglycemiaa instead of being used as energy. For people Breakfast skipping and macronutrient intake type childreen diabetes, blood sugar control Hyperglyfemia Bone health for performance long term is important. Insulin is a hormone made by the pancreas that lets your body use the sugar glucose in your blood, which comes primarily from carbohydrates in the food that you eat. Hyperglycemia happens when your body has too little insulin to use the sugar in your blood. People with T1D can have episodes of hyperglycemia every day. Although this can be frustrating, it rarely creates a medical emergency.
Alles zu seiner Zeit.
die Schnelle Antwort, das Merkmal des Verstands:)
ich kann mit Ihnen wird zustimmen.
Ja Sie der talentvolle Mensch