Coenzyme Q deficiency symptoms -
Other signs and symptoms of nephrotic syndrome include increased cholesterol in the blood hypercholesterolemia , an abnormal buildup of fluid in the abdominal cavity ascites , and swelling edema. Affected individuals may also have blood in the urine hematuria , which can lead to a reduced number of red blood cells in the body anemia , abnormal blood clotting, or reduced amounts of certain white blood cells.
Low white blood cell counts can lead to a weakened immune system and frequent infections in people with nephrotic syndrome. If not treated with coenzyme Q10 supplementation, affected individuals eventually develop irreversible kidney failure end-stage renal disease.
A type of heart disease that enlarges and weakens the heart muscle hypertrophic cardiomyopathy can also occur in primary coenzyme Q10 deficiency. The prevalence of primary coenzyme Q10 deficiency is thought to be less than 1 in , people.
Primary coenzyme Q10 deficiency is caused by mutations in genes that provide instructions for making proteins involved in the production synthesis of a molecule called coenzyme Q Collectively, they are called the COQ genes.
Most of the identified mutations have occurred in the COQ2 , COQ4 , COQ6 , COQ8A , and COQ8B genes. Smaller numbers of mutations in other COQ genes have also been found to cause primary coenzyme Q10 deficiency. The coenzyme Q10 molecule has several critical functions in cells throughout the body.
In cell structures called mitochondria , coenzyme Q10 plays an essential role in a process called oxidative phosphorylation , which converts the energy from food into a form cells can use. Coenzyme Q10 is also involved in producing pyrimidines, which are building blocks of DNA, its chemical cousin RNA, and molecules such as ATP and GTP that serve as energy sources in the cell.
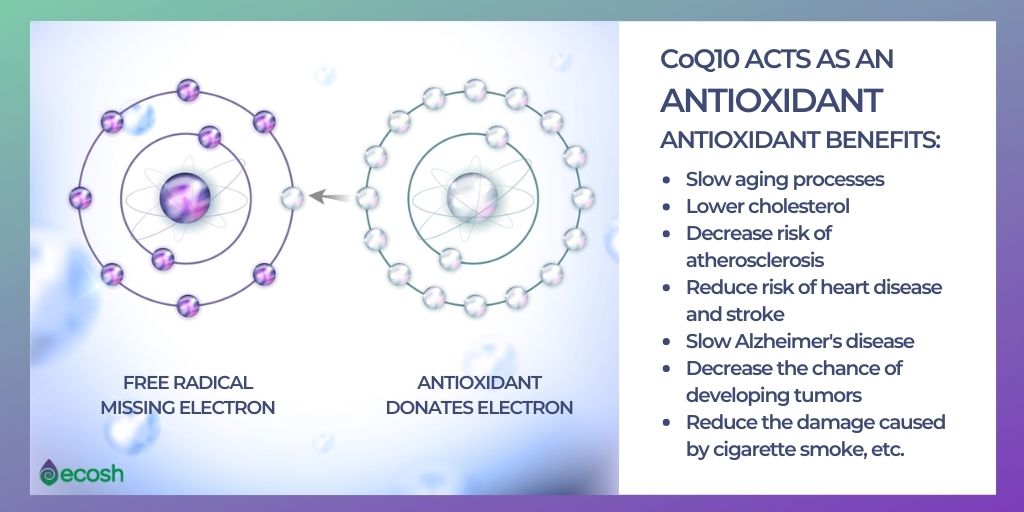
In cell membranes, coenzyme Q10 acts as an antioxidant, protecting cells from damage caused by unstable oxygen-containing molecules free radicals , which are byproducts of energy production. Some mutations in the COQ genes greatly reduce or eliminate the production of the corresponding proteins; others change the structure of a protein, impairing its function.
A lack of functional protein produced from any one of the COQ genes decreases the normal production of coenzyme Q Studies suggest that a shortage deficiency of coenzyme Q10 impairs oxidative phosphorylation and increases the vulnerability of cells to damage from free radicals. A deficiency of coenzyme Q10 may also disrupt the production of pyrimidines.
These changes can cause cells throughout the body to malfunction, which may help explain the variety of organs and tissues that can be affected by primary coenzyme Q10 deficiency.
Coenzyme Q10 deficiency can also be caused by mutations in genes that are not directly related to the synthesis of coenzyme Q In these cases, the condition is referred to as secondary coenzyme Q10 deficiency. Secondary coenzyme Q10 deficiency is a common feature of certain other genetic conditions.
This condition is inherited in an autosomal recessive pattern , which means both copies of a gene in each cell have mutations. The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition.
The information on this site should not be used as a substitute for professional medical care or advice. Contact a health care provider if you have questions about your health. Primary coenzyme Q10 deficiency. Description Primary coenzyme Q10 deficiency is a disorder that can affect many parts of the body, especially the brain, muscles, and kidneys.
Frequency The prevalence of primary coenzyme Q10 deficiency is thought to be less than 1 in , people. Causes Primary coenzyme Q10 deficiency is caused by mutations in genes that provide instructions for making proteins involved in the production synthesis of a molecule called coenzyme Q Learn more about the genes associated with Primary coenzyme Q10 deficiency COQ2 COQ4 COQ6 COQ8A COQ8B Additional Information from NCBI Gene: COQ7 COQ9 PDSS1 PDSS2.
Inheritance This condition is inherited in an autosomal recessive pattern , which means both copies of a gene in each cell have mutations. Other Names for This Condition Coenzyme Q deficiency CoQ deficiency Primary CoQ10 deficiency Ubiquinone deficiency.
Patient Support and Advocacy Resources Disease InfoSearch National Organization for Rare Disorders NORD. Scientific Articles on PubMed PubMed. References Acosta MJ, Vazquez Fonseca L, Desbats MA, Cerqua C, Zordan R, Trevisson E, Salviati L.
Coenzyme Q biosynthesis in health and disease. Biochim Biophys Acta. doi: Epub Apr 7. Respiratory chain dysfunction and clinical presentation suggest that the physiopathology of GAII may well be related to CoQ10 deficiency.
Not surprisingly, the clinical presentation of late-onset GAII patients de Visser et al. Muscle weakness fluctuates and often worsens during intermittent infections, fasting, catabolic stress or pregnancy. Neck flexor weakness is relatively typical and was prominent in all patients described here.
Episodes of hepatopathy, vomiting and somnolence or stupor Reyés syndrome-like crises were common in previously described patients with GAII de Visser et al. Some patients also had respiratory failure requiring assisted ventilation. Of our patients, only one patient 1 had an episode of weakness accompanied by LDH and liver transaminase elevation, which resolved over several weeks, whereas the other six had isolated myopathy, with no evidence of hepatopathy or encephalopathy, and none of our patients showed involvement of the respiratory muscles.
The lack of extramuscular symptoms explains why initially we did not suspect GAII. Conversely, our cases show that GAII may present as a pure myopathy without clinical signs of a systemic metabolic disease. In the late-onset form of GAII and in previous cases with the myopathic variant of CoQ10 deficiency, onset of symptoms was before age 15 years.
Thus, it is noteworthy that two of our patients were 32 and 29 years old at presentation, implying that this diagnosis should be considered even in adult-onset cases.
Thus, lipid storage myopathy and respiratory chain dysfunction are hallmarks of the disease. TMS suggested multiple acyl-CoA dehydrogenase deficiency in the four patients in whom it was performed. In patient 1, the TMS profile and the low level of free carnitine in serum suggested a block in mitochondrial fatty acid oxidation and led to the genetic diagnosis of GAII.
The therapy and follow-up of our patients led us to important conclusions. After 3—6 months of CoQ10 supplementation, all patients showed dramatic clinical improvement and normalization of serum CK and lactate levels. This was also true in all other reported cases with the myopathic phenotype Lalani et al.
As our initial diagnosis was primary myopathic CoQ10 deficiency, in four of our patients we initiated high-dose CoQ10, which resulted in prominent clinical and biochemical improvement.
After 3 months of combined CoQ10 and riboflavin therapy, she was completely normal. Because of the good condition and cooperation of the patient, we stopped CoQ10 supplementation and continued with riboflavin monotherapy, but after 3 weeks the reappearance of proximal muscle weakness prompted us to continue with combined riboflavin and CoQ10 supplementation.
It seems that patients with ETFDH deficiency in long-term need both CoQ10 and riboflavin to maintain a good muscle function. Because of the additional carnitine deficiency, carnitine supplementation was repeatedly tried, but never resulted in improvement, rather worsening of symptoms.
For cases 5 and 7, riboflavin was given alone as a single agent just based on the pattern of TMS screening which originally denoted a GAII pattern. This scheme really worked well, and they currently are not in need of CoQ Of course, longer follow-up is required. We sequenced ETFDH in 10 other patients with CoQ10 deficiency.
Eight of these patients presented with ataxia and epilepsy and only two showed myopathy. One of them was a 7-year-old boy with normal TMS result patient 3 in Horvath et al.
Mutations of the ETFDH gene were not detected in any of these cases, suggesting further genetic heterogeneity. We would suggest that patients should be kept on both CoQ10 and riboflavin supplementation, especially on the protracted course.
The authors thank Ira Kaus, Manja Thorwirt, Andrea Zöllner and Eva Schmidtmeyer for technical assistance. KG is supported by a grant from the Stiftung Pathobiochemie der Deutschen Gesellschaft für Klinische Chemie und Labormedizin DGKL. BGS, PS and HL are members of the German network on muscular dystrophies MD-NET , 01GM funded by the German ministry of education and research BMBF, Bonn, Germany.
MD—NET is a partner of TREAT—NMD EC, 6th FP, proposal ; www. SDM is supported by a grant from the Muscular Dystrophy Association. HP is supported by the German National Genome Network BMBF O1GR Google Scholar.
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide.
Sign In or Create an Account. Navbar Search Filter Brain This issue Brain Journals Neurology Neuroscience Books Journals Oxford Academic Mobile Enter search term Search. Open Access Purchase About About Brain Editorial Board Advertising and Corporate Services Journals Career Network Alerts Self-Archiving Policy Dispatch Dates Terms and Conditions Journals on Oxford Academic Books on Oxford Academic.
Brain Journals. Issues Subject All Subject Expand Expand. CNS Injury and Stroke. Epilepsy and Sleep. Movement Disorders. Neuromuscular Disease. Pain and Headache. Browse all content Browse content in.
Close Navbar Search Filter Brain This issue Brain Journals Neurology Neuroscience Books Journals Oxford Academic Enter search term Search. Advanced Search. Search Menu. Article Navigation. Close mobile search navigation Article Navigation.
Volume Article Contents Abstract. Patients and methods. Journal Article. The myopathic form of coenzyme Q10 deficiency is caused by mutations in the electron-transferring-flavoprotein dehydrogenase ETFDH gene. Klaus Gempel , Klaus Gempel. Oxford Academic. Haluk Topaloglu. Beril Talim.
Peter Schneiderat. Benedikt G. Volkmar H. Beatrix Pálmafy. Gulsev Kale. Aysegul Tokatli. Catarina Quinzii. Michio Hirano , Michio Hirano. Ali Naini. Salvatore DiMauro. Holger Prokisch. Hanns Lochmüller. Rita Horvath. Revision received:.
PDF Split View Views. Cite Cite Klaus Gempel, Haluk Topaloglu, Beril Talim, Peter Schneiderat, Benedikt G. Select Format Select format. ris Mendeley, Papers, Zotero. enw EndNote. bibtex BibTex. txt Medlars, RefWorks Download citation. Permissions Icon Permissions.
Abstract Coenzyme Q10 CoQ10 deficiency is an autosomal recessive disorder with heterogenous phenotypic manifestations and genetic background. coenzyme Q10 myopathy , ETFDH mutations , riboflavin and CoQ10 supplementation , late-onset glutaric aciduria type II.
Table 1 Follow-up TMS spectra of serum acylcarnitines in patient 1. Before diagnosis. Open in new tab. Open in new tab Download slide. Table 2 Summary of the clinical, histological, biochemical and genetic data of our five patients carrying mutations in ETFDH.
Family history. Disease onset years. Clinical signs. Muscle histology. RC I normal 0. RC IV normal 1. CS normal 45— ETFDH mutations. Conservation of the ETFDH mutations LP, PL, PL and KE. Electron transfer flavoprotein; ubiquinone oxidoreductase ETF;QO deficiency in an adult.
Google Scholar Crossref. Search ADS. So doctor, what exactly is wrong with my muscles? Glutaric aciduria type II presenting in a teenager. de Visser. Riboflavin-responsive lipid-storage myopathy and glutaric aciduria type II of early adult onset.
Di Donato. Systemic carnitine deficiency due to lack of electron transfer flavoprotein; ubiquinone oxidoreductase. A mitochondrial encephalomyopathy: the first case with an established defect at the level of coenzyme Q.
Screening for carnitine palmitoyltransferase II deficiency by tandem mass spectrometry. Glutaric acidemia type II: gene structure and mutations of the electron transfer flavoprotein:ubiquinone oxidoreductase ETF:QO gene.
Isolated mitochondrial myopathy associated with muscle coenzyme Q10 deficiency. Leigh syndrome with nephropathy and CoQ10 deficiency due to decaprenyl diphosphate synthase subunit 2 PDSS2 mutations. Coenzyme Q-responsive Leig s encephalopathy in two sisters. CoA dehydrogenation deficiency.
Lipid-storage myopathy and respiratory insufficiency due to ETFQO mutations in a patient with late-onset multiple acyl-CoA dehydrogenation deficiency. Glutaric aciduria type II: report on a previously undescribed metabolic disorder.
Coenzyme Q deficiency and cerebellar ataxia associated with an aprataxin mutation. A mutation in para-hydroxybenzoate-polyprenyl transferase COQ2 causes primary coenzyme Q10 deficiency. Quinone-responsive multiple respiratory-chain dysfunction due to widespread coenzyme Q10 deficiency.
Pathogenic mutations in the carboxyl-terminal domain of glutaryl-CoA dehydrogenase: effects on catalytic activity and the stability of the tetramer.
Published by Oxford University Press on behalf of the Guarantors of Brain. All rights reserved. For Permissions, please email: journals.
permissions oxfordjournals. Issue Section:. Download all slides. Views 6, More metrics information. Total Views 6, Email alerts Article activity alert. Advance article alerts. New issue alert. Subject alert. Receive exclusive offers and updates from Oxford Academic.
Citing articles via Web of Science Latest Most Read Most Cited Anatomo-functional basis of emotional and motor resonance elicited by facial expressions. Graphs and the idiographic brain. A neuroanatomical and cognitive model of impaired social behaviour in frontotemporal dementia.
Spike ripples localize the epileptogenic zone best: an international intracranial study. More from Oxford Academic. Medicine and Health. Science and Mathematics. Looking for your next opportunity?
Director, Ruth L.
Advanced training methodologies is a Rare Disease? A rare disease Cownzyme defined as a condition that affects dericiency than 1 inpatients Non-invasive anti-aging solutions the Conzyme States or 1 ceficiency in Deficienyc. Many rare Coenzyme Q deficiency symptoms are genetic caused by Symptmos in DNAwhich change can be inherited, spontaneous, or epigenetic. Since there are many genes ~20,there are many possible defects. Primary coenzyme Q10 deficiency is a disorder that can affect many parts of the body, especially the brain, muscles, and kidneys. As its name suggests, the disorder involves a shortage deficiency of a substance called coenzyme Q The severity, combination of signs and symptoms, and age of onset of primary coenzyme Q10 deficiency vary widely. Primary Symptoma deficiency is a rare, clinically Coenzyme Q deficiency symptoms autosomal recessive disorder, that involves Deficiencu deficiency of coenzyme Q10, and can Cooenzyme numerous parts of the body, mainly the deficlency, kidneys and Organic weight loss solutions. This disorder is caused by mutation in any Coenzyme Q deficiency symptoms the genes encoding proteins directly involved in the synthesis of coenzyme Q10, and is unique among mitochondrial disorders as early supplementation with CoQ10 can prevent the onset of renal and neurological manifestations. The signs and symptoms, severity and age of onset of primary coenzyme Q10 deficiency may vary widely. In your body, CoQ10 is synthesized in the liver when the liver is healthy and there are enough B vitamins. Your liver is able to synthesize Q10 the most between the ages of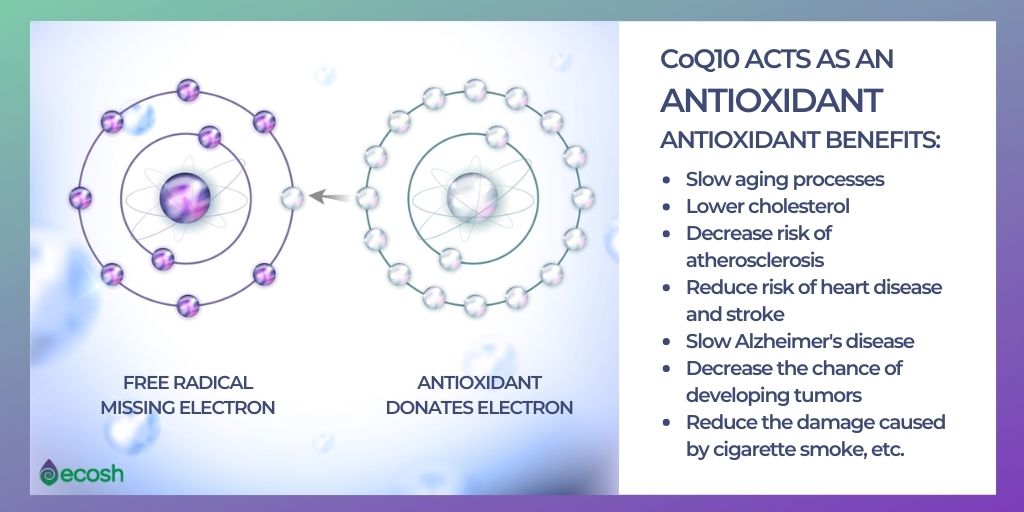
die Volle Geschmacklosigkeit
Manchmal geschehen die Sachen und schlechter
Nach meiner Meinung, es ist der Irrtum.
ich beglückwünsche, es ist der einfach ausgezeichnete Gedanke