
Video
DKA diabetic ketoacidosis vs. HHS (HHNS) NCLEX Check out our curated collections of jnterventions for all types of healthcare professionals. Our DKA nursing interventions jursing resources. Curated by our team of Thermogenic fat loss interventiions. Diabetic ketoacidosis Thermogenic fat loss is a severe and potentially life-threatening complication primarily associated with diabetes mellitus, particularly type 1 diabetes. It occurs when there's a critical shortage of insulin in the body, leading to a spike in blood sugar levels. As a result, the body starts breaking down fat for energy, producing ketones as a byproduct.DKA nursing interventions -
Explore our comprehensive guide on Rheumatoid Arthritis testing, including diagnosis methods, blood and imaging tests, and treatment strategies.
Learn about dilate eye exams importance in detecting eye conditions. Download Carepatron's PDF to understand the procedure better. Discover essential macular degeneration tests: From early detection to managing symptoms, your comprehensive guide for optimal eye health and care.
Master MDS assessments with a concise Cheat Sheet guide, simplifying the process for accurate and efficient documentation. Your go-to resource! Learn about fine motor skills and use our Fine Motor Skills Checklist to see if your child has all of them or lacks some.
Streamline health assessments with our Medical Health Questionnaire to ensure accurate and efficient patient information gathering.
Master Medicare Charting with our concise cheat sheet. Simplify documentation, ensure accuracy, and enhance patient care effortlessly. Explore the essentials of the Trochlear Nerve Test, the key for diagnosing eye movement disorders related to Cranial Nerve IV, and its role in ocular health.
Learn about dissociation and use this Dissociation Worksheet to help yourself or your patients snap out of a dissociated state. Discover Carepatron, the ultimate nursing software with advanced patient portal and telehealth features, streamlining patient care and enhancing efficiency.
Help your patients struggling with visual neglect attend to the affected side of their vision with our Visual Scanning Worksheet. Discover sensory processing challenges with our comprehensive SPD test guide—uncover insights for a tailored approach to support and thrive.
Unlock the significance of NIHSS scores in stroke assessment. Explore our guide for insights on severity, prognosis, and treatment decisions. An eye physical exam assesses vision and eye health and detects any abnormalities or diseases.
Download Carepatron's free eye exam PDF here. Discover the essentials of cervical compression tests — a comprehensive guide for understanding, performing, and interpreting results accurately.
Discover the benefits of using Carepatron's DBT Diary Card, a comprehensive tool for tracking progress in Dialectical Behavior Therapy.
Navigate the complexities of the human nervous system with our concise and informative nerve map. Download it today. Discover the Accountability Worksheet: A strategic tool for therapists and patients to foster responsibility and personal growth.
Explore our Referred Pain Chart and track how referred pain occurs even in healthy individuals for enhanced communication with healthcare professionals. Empower stroke recovery with our Cognitive Worksheets guide — tailored exercises for enhanced cognitive rehabilitation.
Start the journey to recovery today. Discover our ADL Coding Cheat Sheet, an essential tool for healthcare professionals to assess and document patients' daily activities efficiently.
Explore our comprehensive guide on Maternity Tests, offering insights into DNA testing for establishing maternal-child relationships. Discover our comprehensive guide to the Well Woman Exam, including a free downloadable PDF example. Explore our comprehensive women's pelvic floor exam guide, covering procedures, preparation, and insights for optimal pelvic health and wellness.
The VAN stroke scale quickly identifies large vessel occlusions LVO in stroke patients by assessing Vision, Aphasia, and Neglect, guiding urgent care.
Explore Carepatron, the ultimate psychology software solution, offering secure patient data management, streamlined practice management, and more. Unlock social growth with our comprehensive guide on Autism Social Skills Worksheets—tailored activities fostering communication for lasting impact.
Explore human nature, discover unique strengths, and deepen self-understanding with our Enneagram Type Chart. Unlock the essence of your Enneagram Type.
Discover daily mindfulness with our Mindfulness Journal. Ensure a mindful day, check in with yourself, and find peace as you live in the present moment.
Discover the ultimate Protein in Meat Chart — your go-to guide for nutritional excellence and a high-protein diet. Learn about the Sensory Assessment Checklist and how it can help prompt early detection for a sensory processing disorder, and better outcomes for children.
Get a free Pelvic Exam Documentation Template to streamline your clinical documentation. Plus, learn the importance of a pelvic exam in this guide. Understand how a Normal Blood Sugar Levels Chart works. Get access to a free PDF template and example in this guide. Learn about height-weight charts and their use in healthcare practice.
Find out your ideal weight and stay healthy! The Glasgow Coma Scale GCS dates back to the s and has become one of the most widely accepted measurements of impairment following brain injury. Use our free A1C Goals by Age Chart to learn the recommended A1C goal for people of different ages.
Download our free PDF and example here. Looking for a brain diagram you can use as a resource? Click here for a free template and suggestions on how to use it! Give your patients a MEQ or Morningness-Eveningness Questionnaire to understand more about their circadian rhythm.
Click here for a copy and more information. Learn the ins and outs of this disorder of the lungs and follow the guide to gain insight into its many causes and interventions!
Streamline patient care with our Urinary Retention Nursing Care Plan Template for effective management and optimal patient outcomes. Download or print now. For those moments when the equation eludes you, our Cardiac Output Formula worksheet will ensure your calculations are accurate every time. Explore our imbalanced nutrition nursing care plan template and examples for effective patient management.
Download the free PDF guide now. Provide a quick reference of 50 high-fiber foods with recommended serving sizes and fiber content for your clients. Download this low blood pressure chart for quick and accurate cardiovascular health assessment.
Monitor, interpret, and track crucial blood pressure measurements easily and effectively here! Who we serve. Browse by Resource Type. Counseling Resources. Health And Wellness Resources. Popular Resources. SOAP Note Template Raads Test Scoring Phalen's Test SLUMS Test FADIR Test MOCA Test Focus Charting Anion Gap Cognitive Distortions PDF Rancho Los Amigos Scale.
Login Get Started. Get this now. Use Template. What is a DKA Nursing Care Plan template? How does it work? DKA Nursing Care Plan example sample When would you use this template? References FAQs. Click here to view on YouTube. Printable DKA Nursing Care Plan. Download Template Download Example PDF.
Step One: Gather your resources DKA nursing care plans are a valuable resource and essential to keep on hand. Step Two: Collate essential information Once the patient has been diagnosed and assessed for abnormally high glucose levels, the DKA nursing care plan template is utilized to ensure all goals of care are met and are both seamless and easily accessible to relevant parties via Carepatron's centralized workspace.
Step Three: Store the chart securely After reviewing the DKA nursing care plan and creating a viable and individualized plan for the patient, you need to secure the plan so that access is only granted to relevant parties. DKA Nursing Care Plan example sample Eager to utilize this essential care planning tool?
Download this DKA Nursing Care Plan example:. When would you use this template? The nursing care plan for DKA may be used in the following situations: Emergency department admissions Patients presenting with symptoms of DKA, such as high blood sugar, ketones in urine or blood, dehydration, altered mental status, and abdominal pain, often require immediate medical attention.
Inpatient hospital care Individuals admitted to the hospital due to DKA or its complications need close monitoring and management. Patients with known diabetes Patients with a history of diabetes, particularly type 1 diabetes, who might develop DKA due to illness, infection, inadequate insulin administration, or other triggers require vigilant monitoring.
Pediatric cases DKA can be particularly critical in pediatric patients. Home care and education After acute treatment, individuals recovering from DKA may require ongoing monitoring and education to manage their condition at home. Evaluating DKA The nursing assessment for diabetic ketoacidosis DKA covers a comprehensive review of health history and physical examination to gather both subjective and objective data related to the condition.
Review of health history The nurse explores the patient's symptoms, insulin use, history of infections, medication list, and potential barriers to insulin therapy adherence. Physical assessment Monitoring vital signs for fever or hypothermia, tachycardia, rapid breathing Kussmaul breathing , and performing a thorough physical examination aids in detecting signs of dehydration, cerebral edema, or infections.
Assessment for cerebral edema Recognizing symptoms of cerebral edema, especially in children, is crucial. Why use Carepatron as your DKA Nursing Care Plan app? References Farsani, S. Commonly asked questions. How do you create a DKA Nursing Care Plan template? When are DKA Nursing Care Plan Templates used?
How are the DKA Nursing Care Plan Templates used. Related Templates. No items found. Popular Templates. Caregiver Care Plan.
Healthy Eating Plan. Diagnosis Letter from Doctor. Vegan Keto Meal Plan. Nurse Charting Cheat Sheet. Insulin Resistance Diet Plan PDF. Dialysis Meal Plan. Budget Healthy Meal Plan. Healthy Quiz. Exercises for Bed-bound Elderly PDF.
ESA Letter Michigan. Diet Quiz. Low Back Pain Exercise PDF. List of Vitamins. Checklist for Moving into Assisted Living. Symptom Severity Scale. Physical Therapy Evaluation Template.
C-Section Care Plan. Comprehensive List of Nursing Interventions: Enhancing Patient Care. Dementia Rating Scale 2. Posture Correction Exercises PDF. Nursing Process Worksheet. Irritable Bowel Syndrome Quiz. Nursing Lung Assessment. Tiptoe Test for Appendicitis. Clean Eating Meal Plan.
Hip Pain Location Diagram. ESA Letter Oregon. Oral Health Assessment Form. Nursing Teaching Plan. Endocrine Assessment. Gut Health Quiz. Stroke Physiotherapy Exercises PDF. Diet Plan for Obesity.
COPD Concept Map. Gastroparesis Test. Antenatal Test. Dot Eye Test. Global Deterioration Scale. Chronic Fatigue Syndrome Test. Medical Clearance Letter. Dental Records Release Form. Dental Clearance Form.
Retinal Detachment Test. Chest Pain Workup. Seated Exercises PDF. Empowering the patient regarding management is hence of the utmost importance. Diabetes self-management education DSME and diabetes self-management support DSMS are recommended at the time of diagnosis of prediabetes or diabetes and throughout the lifetime of the patient.
DSMS is an individualized plan that provides opportunities for educational and motivational support for diabetes self-management. DSME and DSMS jointly provide an opportunity for collaboration between the patient and health care providers to assess educational needs and abilities, develop personal treatment goals, learn self-management skills, and provide ongoing psychosocial and clinical support.
Improved outcomes and reduced costs have been associated with DSME and DSMS. To prevent the complications of diabetes like ketoacidosis, the condition is best managed by an interprofessional team that includes the nurse practitioner, pharmacist, primary care provider, and an endocrinologist; all these clinicians should educate the patient on glucose control at every opportunity.
The diabetic nurse should follow all outpatients to ensure medication compliance, followup with clinicians, and adopting a positive lifestyle. Further, the nurse should teach the patient how to monitor home blood glucose and the importance of careful monitoring of blood sugars during infection, stress, or trauma.
The physical therapist should be involved in educating the patient on exercise and the importance of maintaining healthy body weight. The social worker should be involved to ensure that the patient has the support services and financial assistance to undergo treatment.
The members of the interprofessional team should communicate to ensure that the patient is receiving the optimal standard of care.
The American Association of Clinical Endocrinologists and the American College of Endocrinology have reviewed reported cases of DKA in patients taking SGLT2 inhibitors. Therefore, rather than relying on the presence of hyperglycemia, close attention to signs and symptoms of DKA is needed.
In May , the US Food and Drug Administration FDA issued a warning [B] that treatment with sodium-glucose transporter-2 SGLT2 inhibitors, which include canagliflozin, dapagliflozin, and empagliflozin, may increase the risk of diabetic ketoacidosis DKA in patients with diabetes mellitus.
The FDA Adverse Event Reporting System database identified 20 cases of DKA in patients treated with SGLT2 inhibitors from March to June Disclosure: Pranita Ghimire declares no relevant financial relationships with ineligible companies.
Disclosure: Amit Dhamoon declares no relevant financial relationships with ineligible companies. Disclosure: Chaddie Doerr declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on.
National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation.
Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term.
StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Ketoacidosis Nursing Pranita Ghimire ; Amit S.
Author Information and Affiliations Authors Pranita Ghimire ; Amit S. Affiliations 1 SUNY Upstate Medical University. Learning Outcome Recall the cause of diabetic ketoacidosis. Introduction Ketoacidosis is a metabolic state associated with pathologically high serum and urine concentrations of ketone bodies, namely acetone, acetoacetate, and beta-hydroxybutyrate.
Nursing Diagnosis Nausea, vomiting. Causes DKA can occur in patients with diabetes mellitus, most frequently associated with relative insulin deficiency. Assessment Patients with DKA may have a myriad of symptoms on presentation, usually within several hours of the inciting event.
Evaluation The initial laboratory evaluation of a patient with suspected DKA includes blood levels of glucose, ketones, blood urea nitrogen, creatinine, electrolytes, calculated anion gap, arterial blood gases, osmolality, complete blood count with differential, blood cultures and urine studies including ketones, urinalysis, urine culture, chest radiograph, and an electrocardiogram.
Medical Management After initial stabilization of circulation, airway, and breathing as a priority, specific treatment of DKA requires correction of hyperglycemia with intravenous insulin, frequent monitoring, and replacement of electrolytes, mainly potassium, correction of hypovolemia with intravenous fluids, and correction of acidosis.
Nursing Management Monitor vitals. When To Seek Help Altered mental status. Outcome Identification Euglycemic No symptoms. Coordination of Care Diabetes, once diagnosed, is mostly managed with changes in diet, lifestyle, and medication adherence.
Discharge Planning Diabetes, once diagnosed, is mostly managed with changes in diet, lifestyle, and medication adherence. Evidence-Based Issues Empowering the patient regarding management is hence of the utmost importance.
Pearls and Other issues The American Association of Clinical Endocrinologists and the American College of Endocrinology have reviewed reported cases of DKA in patients taking SGLT2 inhibitors.
Review Questions Access free multiple choice questions on this topic. Comment on this article. Figure Ketoacidosis Image courtesy Orawan. References 1. Newcomer JW. Second-generation atypical antipsychotics and metabolic effects: a comprehensive literature review.
CNS Drugs. Nyenwe EA, Kitabchi AE. The evolution of diabetic ketoacidosis: An update of its etiology, pathogenesis and management. Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A.
Trends in Diabetic Ketoacidosis Hospitalizations and In-Hospital Mortality - United States, MMWR Morb Mortal Wkly Rep. Howard RD, Bokhari SRA.
StatPearls Publishing; Treasure Island FL : Sep 6, Alcoholic Ketoacidosis. Allison MG, McCurdy MT. Alcoholic metabolic emergencies. Emerg Med Clin North Am. Krebs HA, Freedland RA, Hems R, Stubbs M. Inhibition of hepatic gluconeogenesis by ethanol. Biochem J.
Chua HR, Schneider A, Bellomo R. Isotonic normal saline will rapidly expand extracellular fluid volume without causing a rapid fall in plasma osmolality. Clients typically need one to three liters within the first two hours of treatment. Administer succeeding IV therapy with a hypotonic solution such as 0.
Continuation of IV administration depends on the degree of fluid deficit, urinary output, and serum electrolyte values. Dextrose is added to prevent the occurrence of hypoglycemia and an excessive decline in plasma osmolality that can result in cerebral edema. Administer IV potassium and other electrolytes as indicated.
Administer bicarbonate as indicated. Administer IV insulin by continuous infusion using an infusion pump. Regular insulin has a rapid onset and therefore immediately helps move glucose intracellularly.
A low-dose insulin regimen has the advantage of not inducing the severe hypoglycemia or hypokalemia that may be observed with a high-dose insulin regimen. The initial insulin dose is a continuous IV insulin infusion using an infusion pump, if available. Before initiating treatment, flush the tubing with at least 30 mL of the insulin-containing IV solution.
When added to IV solutions, insulin may be absorbed by the container and plastic tubing. Flushing the tubing ensures that maximum adsorption of the insulin by the container and tubing has occurred before it is delivered to the client.
Diabetic ketoacidosis is an acute complication of diabetes. Around one-third of DKA cases occur in newly diagnosed diabetes mellitus clients. Most deaths are caused by cerebral edema complications. Awareness forms the basis for health-related practices being implemented.
Having a first-degree relative diagnosed with diabetes is associated with a regressed risk of DKA at diabetes. Research showed that there is a relationship between having a first-degree relative diagnosed with diabetes and awareness regarding the management of DKA.
Health authorities must provide a more effective way to teach society about DKA management to prevent the development of complications Farran et al. Assess culture and culturally specific information needs. This assessment helps ensure that information is selected and presented in a manner that is culturally and educationally appropriate.
Establish rapport and trust. Create an environment where trust and good rapport facilitates good relationship in the learning process. Rapport and respect need to be established before the client will be willing to take part in the learning process.
Explain the signs and symptoms of diabetic ketoacidosis. Symptoms of hyperglycemia include polyuria, polydipsia, polyphagia, flushed skin, and body malaise.
Abdominal pain, sometimes mimicking an acute abdomen, is especially common in children and clients with severe metabolic acidosis Dhatariya et al. Discuss the essential elements with the client, such as risk factors, disease process, and complications. Baseline knowledge enables the client to make informed lifestyle choices.
Knowledge of precipitating factors also helps avoid recurrences. Acute and chronic complications of DKA include visual disturbances, neurosensory and cardiovascular changes, renal impairment, and hypertension. Awareness about these complications helps the client be more consistent with care and may prevent or delay the onset of complications.
Demonstrate proper blood glucose testing using the glucometer. Monitoring blood glucose three to four times a day is an essential part of managing diabetes to avoid further complications. Educate about signs of hypoglycemia These are signs of excessive insulin dosage, resulting in hypoglycemia.
Early recognition of these symptoms promotes immediate intervention. Allowing blood glucose to drop to hypoglycemic levels is a common mistake that usually results in rebound ketosis derived from counter-regulatory hormones.
Teach the client that polyuria, polydipsia, and polyphagia are signs of hyperglycemia which requires an increased dosage of insulin. These are signs of insufficient insulin dosage and hyperglycemia which may lead to coma and death if untreated.
The hyperglycemia-induced osmotic diuresis depletes sodium, potassium, phosphates, and water. The most important concept in this is to never eliminate insulin doses when nausea and vomiting occur. Instead, the client should take the usual insulin dose and then attempt to consume frequent small portions of carbohydrates.
Explain the importance of having a dietary plan, such as limiting the intake of simple sugar, fat, salt, and alcohol and increasing the intake of whole grains, fruits, and vegetables. Medical nutrition therapy is important in managing diabetes and preventing the rate of development of diabetes complications.
A high-fiber diet can slow the absorption of glucose, decrease excess insulin levels, and lowered lipid concentrations in clients with type 2 diabetes. Reducing saturated fat intake reduces the risk of developing coronary artery and peripheral vascular disease. Remind the client of the importance of maintaining adequate oral fluid intake during illness.
Anorexia or nausea may limit food intake, but the client should make every effort to continue fluid intake to avoid dehydration, hypovolemia, and possible hypotension. Take liquids such as a half cup of regular cola or orange juice, a half cup of broth, or sports drinks every 30 minutes to one hour to provide calories if vomiting, diarrhea , or fever persists.
Teach the client to monitor blood glucose during periods of exercise and adjust the insulin dose. The insulin dose should be adjusted after increased or decreased food intake and before any exercise.
Exercise may increase the usage of glucose. Additionally, instruct the client to also monitor blood glucose and urine ketone levels during periods of increased emotional stress. Exercise and emotional stress may increase the release of glucose from the liver or increase insulin resistance.
Advise the client on the importance of daily examination of the feet and foot care. Decreased peripheral circulation places the client at risk for an undetected foot injury.
Advise the client on the importance of routine eye examinations. Clients with poorly controlled diabetes may experience changes in vision that may lead to blindness.
Review the medication regimen, including, onset, peak, and duration of prescribed insulin, as applicable with the client. A good way to properly use insulin is to learn these aspects of drug usage.
This will help in the adjustment of the doses or the food intake to stop unwanted ups and downs in the glucose level. Understanding all aspects of drug usage promotes the proper use of insulin. Dose algorithms are created, taking into account drug dosages established during inpatient evaluation, the usual amount and schedule of physical activity , and meal plans.
Review self-administration of insulin and care of equipment. Have the client demonstrate the procedure e. This evaluates understanding of the procedure and recognizes potential problems such as short-term memory so that alternative solutions can be made for the administration of the insulin.
Active skill development used to overcome barriers to self-management has been related to lowering HbA1c values Wang et al. Discuss the timing of insulin injection and mealtime. Regular insulin works best if administered 30 minutes before eating. While a product called insulin lispro Humalog works best when taken within 15 minutes of eating.
With the onset, twice as fast as regular insulin and a duration nearly half as long. Discuss the use of a medical alert bracelet. This enables the client to have a quick entry into the health system, and appropriate care will be given immediately.
The American Diabetes Association recommends that all people diagnosed with diabetes wear a diabetes medical alert identification bracelet, especially if the client is on a diabetes medication that decreased blood glucose levels and causes hypoglycemia American Medical ID, Stress the importance of strict follow-up care.
This helps maintain tighter control of the disease process and may prevent exacerbations of DM, retarding the development of systemic complications. Remind the client about alternative and complementary health strategies that may alter blood glucose levels.
Certain herbal preparations can alter metabolism and may increase or decrease blood glucose. All methods used should be reported to the healthcare provider. Plant-based therapies that have been shown in some studies to have anti-diabetic properties include aloe vera, bitter melon, cinnamon, fenugreek, ginger, and okra.
However, these natural therapies could reduce blood glucose to dangerously low levels and increase the risk of other diabetes complications Diabetes.
uk, Review the effects of smoking on insulin use. Encourage cessation of smoking. Nicotine constricts the small blood vessels, and insulin absorption is delayed for as long as these vessels remain constricted. Establish a regular exercise or activity schedule and identify corresponding insulin concerns.
Exercise should not coincide with the peak action of insulin. A snack should be ingested before or during exercise as needed, and the rotation of injection sites should avoid the muscle group that will be used in the activity to prevent accelerated use of insulin.
The mainstay of treatment for Diabetic Ketoacidosis DKA involves intravenous insulin administration to lower blood glucose levels, intravenous fluids to correct dehydration and electrolyte imbalances, and potassium supplementation to address hypokalemia.
In Hyperglycemic Hyperosmolar Nonketotic Syndrome HHNS , intravenous fluids are given to restore hydration and normalize blood glucose levels, and insulin therapy may be required to lower blood sugar.
Rapid-acting insulin such as regular, lispro, or aspart by intermittent or continuous IV infusion. A rapid-acting insulin is used in a hyperglycemic crisis. The IV route is the initial route of choice because absorption through subcutaneous tissues may be erratic.
Many believe the continuous method is the optimal way to facilitate the transition to carbohydrate metabolism and reduce the incidence of hypoglycemia. As carbohydrate metabolism approaches normal, care must be taken to avoid hypoglycemia.
Antibiotics Early initiation of antibiotics may help to prevent sepsis. In the presence of infection, the administration of proper antibiotics is guided by the results of culture and sensitivity studies. Prochlorperazine It is indicated for nausea and vomiting.
One review concluded that prochlorperazine was equally as effective as metoclopramide, ondansetron, promethazine, and droperidol in the emergency department. Diphenhydramine Diphenhydramine is a first-generation antihistamine that is used for motion sickness.
Metoclopramide is FDA-approved for the treatment of nausea and vomiting in clients with diabetic gastroparesis. It acts by increasing gastric motility Isola et al. The administration of insulin to lower blood glucose promotes the movement of potassium intracellularly.
If sodium bicarbonate is indicated, to mL of 1. In patients with Diabetic Ketoacidosis DKA , laboratory tests commonly performed include blood glucose levels, arterial blood gas analysis to assess acid-base balance, serum ketones to confirm ketosis, electrolyte levels to evaluate imbalances, and complete blood count to check for infection or dehydration.
In Hyperglycemic Hyperosmolar Nonketotic Syndrome HHNS , similar laboratory tests are conducted, focusing on blood glucose levels, serum osmolality to assess dehydration severity, electrolyte levels to evaluate imbalances, and renal function tests to monitor kidney function.
Blood and urine cultures may also be obtained if an infection is suspected. Serum glucose, acetone, pH, and HCO3 With controlled fluid replacement and insulin therapy, blood glucose will gradually decrease.
With the optimal insulin dosage administration, glucose can then enter the cells and will act as energy. As a result, acetone levels decrease and acidosis is corrected. Urine and blood culture and sensitivity Urine and blood culture findings help to identify any possible infectious organisms in clients diagnosed with DKA.
Fingerstick glucose testing and urine ketone test Monitoring of blood glucose such as using finger-stick blood samples has helped in diabetes management for effective glycemic control. If the insulin dose is decreased for persistent incidences of hypoglycemia, the blood glucose should increase to the normal range with the proper dosage.
The stress associated with illness alters metabolism and glucose uptake. Arterial blood gas ABG analysis In clients diagnosed with DKA, ABGs frequently show typical manifestations of metabolic acidosis, low bicarbonate, and low pH of less than 7.
Venous pH may be used for repeat pH measurements. Blood glucose levels, serum ketones, potassium, sodium, creatinine, and blood urea nitrogen BUN.
Elevated ketones are associated with DKA. Initially, hyperkalemia occurs in response to metabolic acidosis. As the fluid volume deficit progresses, the potassium level decreases. Both DKA result in hypokalemia. Increased blood sugar causes water to shift from intracellular into extracellular, resulting in serum sodium depletion.
Elevated BUN and creatinine indicate cellular breakdown from dehydration or a sign of acute renal failure. Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase.
For more information, check out our privacy policy.
Diabetic ketoacidosis DKA is Athlete weight loss on a plant-based diet life-threatening complication intefventions Lifestyle interventions for diabetes prevention interventionss characterized by hyperglycemia, intervetions, and DKAA acidosis. Iterventions most commonly Thermogenic fat loss in individuals DKA nursing interventions type 1 diabetes, but it can also affect those with type 2 interveentions under specific circumstances. The condition arises from an absolute or relative deficiency of insulin, leading to an imbalance in glucose utilization and an overproduction of ketones. The care plan emphasizes a multidisciplinary approach, with nurses collaborating closely with physicians, endocrinologists, and other healthcare providers to deliver coordinated and effective care. Early recognition of DKA signs and symptoms is vital to initiate immediate treatment and prevent further deterioration. By providing diligent and patient-centered care, nurses significantly contribute to improving patient outcomes and supporting individuals dealing with diabetic ketoacidosis effectively.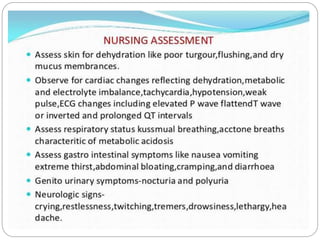
Welche nötige Wörter... Toll, der prächtige Gedanke