Carbohydrate metabolism and postprandial glucose response -
Raue G, Keim V. Sekundärer Diabetes bei chronischer Pankreatitis. Z Gastroenterol ; 37 Suppl 1 : 4—9. Lankisch PG, Löhr-Happe A, Otto J, Creutzfeldt W. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion ; — Phelps G, Chapman I, Hall P, Braund W, Mackinnon M.
Prevalence of genetic haemochromatosis among diabetic patients. Lancet ii ; —4. Danne T, Nimri R, Battelino T, Bergenstal RM, Close KC, DeVries JH, et al.
International consensus on use of continuous glucose monitoring. Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med ; — Juvenile Diabetes Research Foundation.
Prolonged nocturnal hypoglycemia is common during 12 months of glucose monitoring in children and adults with type 1 diabetes. Diabetes Care ; —8. Agus MSD, Steil GM, Wypij D, Costello JM, Laussen PC, Langer M, et al. Tight glycemic control versus standard care after pediatric cardiac surgery.
White NH. Diabetic ketoacidosis in children. Endocrinol Metab Clin North Am ; — Delaney MF, Zisman A, Kettyle WM. Diabetic ketoacidosis and hyperglycemic hyperosmolar non ketotic syndrome.
Rosenbloom AL. Hyperglycemic hyperosmolar state: an emerging pediatric problem. J Pediatr ; —4. Selvin E, Sacks DB. Monitoring glycemic control in endstage renal disease: what should be measured.
Clin chem ; —9. Skyler JS. Microvascular complications. Retinopathy and nephropathy. Diabetic retinopathy. Diabetes Care ; S70—S Diabetic nephropathy. Diabetes Care ; S66—S Rawshani A, Rawshani A, Franzen S, Eliasson B, Svensson AM, Miftaraj M, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes.
Giugliano D, Standl E, Visboll T, Betteridge J, Bonadonna R, Campbell IW, et al. Is the current therapeutic armamentarium in diabetes enough to control the epidemic and its consequences? What are the shortcomings.
Acta Diabetol ; — Duckworth W, Abraira C, Moritz T, Reda D, Emanuele N, Reaven PD, et al. Glucose control and vascular complications in veterans with type 2 diabetes.
Kelly TN, Bazzano LA, Fonseca VA, Theti TK, Reynolds K, He J. Systematic review: glucose control and cardiovascular disease in type 2 diabetes. Ann Intern Med ; — Capes SE, Hunt D, Malmberg K, et al. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: A systematic overview.
Lancet ; ; —8. Malmberg K, Ryden L, Efendic S, et al. Randomized trial of insulin-glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction DIGAMI study : effects on mortality at 1 year later.
J Am Coll Cardiol ; 57— Boulton AJM, Rayaz AM. Diabetic neuropathy. Med Clin North Am ; — Kuller LH, Dorman JS, Wolf PA. Cerebrovascular disease and diabetes mellitus. In: Harris MI, Hamman RF, eds. Diabetes in America-Diabetes data compiled US Dept of Health and Human Services.
Bethesda ; 1— Nagi M, Pfefferkorn T, Haberl RL. Blutzucker and Schlaganfall. Nervenarzt ; —9. Kalaria RN. Diabetes, microvascular pathology and Alzheimer disease. Nature Reviews Neurology ; 5: —6. Ehrmann DA. Polycystic ovary syndrome.
Nestler JE. Should patients with polycystic ovarian syndrome be treated with metformin? Human Reprod ; —3. Vogel A, Strassburg CP, Brabant G, Manns MP.
Autoimmun polyglanduläre Syndrome. Dtsch Ärztebl ; A—A Concannon P, Rich SS, Nepom GT. Genetics of type 1A diabetes. Mosca A, Paleari R, Dalfra MG, Di Canni G, Cuccuru I, Pellegrini G, et al. Reference intervals for hemoglobin A1c in pregnant women: data from Italian multicenter study.
Clin Chem ; — Ward WK, Bolgiano DC, McKnight B, et al. Diminished B cell secretory capacity in patients with noninsulin-dependent diabetes mellitus. J Clin Invest ; — Joost HG, Fritsche A, Häring HU, Pfeiffer AFH, Roden M, Schulze MB. Diabetes mellitus Typ 2: Risikobestimmung wird präzisiert.
Dtsch Ärztebl ; —3. Stomer GD. Hyperosmolar hyperglycemic state. Amer Family Phys ; — Dinneen SH, Gerich J, Rizza R. Carbohydrate metabolism in non-insulin-dependent diabetes mellitus. Karounos DG. Convergence of genetic and environmental factors in the immunopathogenesis of type 1 diabetes mellitus.
J Clin Lig Assay ; — Kahn HS, Cheng YJ, Thompson TJ, Imperatore G, Gregg EW. Two risk-scoring systems for predicting incident diabetes mellitus in U. adults age 45 to 64 years. Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC.
β-cell deficit and increased β-cell apoptosis in humans with diabetes type 2. Diabetes ; — Lamb EJ, Day AP. New diagnostic criteria for diabetes mellitus: are we any further forward?
Haataja L, Gurlo T, Huang CJ, Butler PC. Islet amyloid in type 2 diabetes, and their toxic oligomer hypothesis. Yarandi R, Vaismoradi M, Panahi MH, Kymre IG, Behoudi-Gandevani S.
Mild gestational diabetes and adverse pregnancy outcome. a systemic review and meta-analysis. Frontiers in Medicine ; doi: Ryan EA. Pregnancy in diabetes. Gestational diabetes mellitus. Diabetes Care ; S74—S Aguilar-Bryan L, Bryan J. Neonatal diabetes mellitus. Mayer-Davis E, Lawrence JM, Dabelea D, Divers J, Isom S, Dolan L, et al.
Incidence trends of type 1 and type 2 diabetes among youths, — N Engl J Med ; — Vidal J, Kahn SE. Regulation of insulin secretion in vivo.
In Lowe WL, Jr, ed. Genetics of diabetes mellitus. Boston; Kluwer — Kolb H, Mandrup-Poulsen T. The global diabetes epidemic as a consequence of lifestyle-induced low-grade inflammation. Diabetologia ; 10— Larsen S. Diabetes mellitus secondary to chronic pancreatitis. Danish Medical Bulletin ; — Müller MJ, Pirlich M, Balks HJ, Selberg O, Glucose intolerance in liver cirrhosis: role of hepatic and non-hepatic influences.
J Clin Chem Clin Biochem ; George DK, Evans RM, Crofton RW, Gunn RI. Testing for hemochromatosis in the diabetic clinic. Ann Clin Biochem ; —6. Acromegaly: Unravelling a complex disease. Growth Regulation ; 5: — Bowes SB, Benn JJ, Scobie IN, Umpleby AM, Lowy C, Sönksen PH.
Clin Endocrinol ; —6. Schlaghecke R. Diabetes mellitus bei verschiedenen endokrinologischen Erkrankungen. In: Berger M, ed. Diabetes mellitus. München; Urban and Schwarzenberg — Feig DS, Donovan LE, Corcoy R, Murphy KE, Amiel SA, Hunt KF, et al.
Continuous glucose monitoring in pregnant women with type 1 diabetes Concept : a multicentre international randomised controlled trial.
Lancet ; : — Implications of the diabetes control and complications trial. Diabetes Care ; S24—S Cornblath M, Schwartz R. Hypoglycemia in the neonate. J Pediatr Endocrinol ; 6: — Silverman BL, Metzger BE, Cho NH, et al.
Impaired glucose tolerance in adolescent offspring of diabetic mothers. Shohat M, Merlob P, Reisner SH. Neonatal polycythemia: I. Early diagnosis and incidence relating to time of sampling. Pediatrics ; 7— Shohat M, Reisner SH, Mimouni M, Merlob P. Neonatal polycythemia: II. Definition related to time of sampling.
Pediatrics ; 11—3. Kerner W. Klassifikation and Diagnose des Diabetes mellitus. Dtsch Ärztebl ; B—8. Sacks DB, Bruns DE, Goldstein DE, MacLaren K, McDonald JM, Parrott M. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus.
Hyperglycaemia and risk of adverse perinatal outcomes: £systematic review and meta-analysis. The NICE-SUGAR Study investigators. Intensive versus conventional glucose control in critically ill patients.
Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS. Diabetes prevalence and therapeutic target achievement in the United States, — Am J Med ; — Gourdy P. Diabetes and oral conception. Clin Endocrinol and Metab ; 67— Braunwald E. Gliflozins in the management of cardiovascular disease.
N Engl J Med ; 21 : — DeBoer IH, Khunti K, Sadusky T, Rosas SE, Rossing P, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association ADA and Kidney Disease: Improving Global Outcomes KDIGO.
Kidney Int ; 5: 1— See also Section 3. The term hypoglycemia refers to a low blood glucose concentration associated with clinical symptoms.
Hypoglycemia is the result of an imbalance between the inflow of glucose into the bloodstream due to decreased endogenous glucose production or deficient glucose uptake, and the consumption of glucose by the tissues. The glucose threshold for a decrease in the blood insulin concentration is approx.
Glucagon and catecholamines raise the blood glucose level within minutes by stimulating hepatic glycogenolysis and gluconeogenesis as well as renal gluconeogenesis.
The substrates of gluconeogenesis are glycerol, free fatty acids, and amino acids. Cortisol and growth hormone reduce the glucose consumption of insulin-sensitive tissues and lead to an increase in blood glucose within hours.
The main source of energy for the brain is glucose, and there are protective mechanisms to maintain glucose homeostasis. the sympathoadrenal nervous system is activated, leading to hypoglycemic symptoms such as anxiety, sweating, tremor, fast heartbeat, and hunger. These end-organ responses, also called autonomic symptoms, can progress to neuroglycopenic symptoms including behavioral changes, cognitive dysfunction, seizures, and coma.
However, the threshold for cognitive dysfunction depends on various clinical aspects and psychometric tests. The clinical symptoms associated with a decrease in glucose concentrations are shown in Fig. The aforementioned glucose levels are a highly specific criterion for hypoglycemia.
If levels are below the thresholds suggested by Whipple, further clinical investigations are necessary, even in the absence of hypoglycemia symptoms. Hypoglycemia is not a diagnosis but a pathological state, the cause of which must be determined. The most common diagnoses at admission in patients presenting with hypoglycemia are diabetes mellitus, alcoholism, sepsis, and reactive hypoglycemia.
Insulinomas are very rare, with a prevalence of 4 cases per 1 million population per year. For evaluation refer to Section 3. Iatrogenic hypoglycemia in diabetics is evaluated based on medical history.
Hypoglycemia syndromes which are due to an insulinoma predominantly occur in the fasting state, rarely in the fasting plus postprandial state, and very rarely only in the postprandial state. Postprandial symptoms, which occur 2—4 h after meals are classified as food-stimulated and those which occur more than 5 h after meals are classified as food-deprived.
Autonomous symptoms without hypoglycemia, also known as pseudo-hypoglycemia, which occur after meals usually cannot confirmed as arising from hypoglycemia. The flow chart in Fig. Blood glucose: detection of hypoglycemia.
In this case, the h fast or another functional test should be performed. Findings on hypoglycemia in adults and drug-associated hypoglycemia and their diagnostic significance are listed in Tab.
Detection and differentiation of hypoglycemia by determination of insulin, C-peptide and β-hydroxy butyrate Tab. C-peptide suppression test, intravenous tolbutamide test, glucagon test: these tests are performed if the h fast is not conclusive.
Following enteral feeding, blood glucose levels cycle, with a peak occurring about 1 h after food intake. If hypoglycemia is suspected, a blood sample should be taken just before the second food intake.
Low glucose levels in the first 24—48 h are not uncommon in normally developing newborns who are breast-fed. Every year, approx. The main etiologies are infections, drug-induced intoxications, seizures, and metabolic disorders. For the molecular basis of glucose homeostasis and incidence of congenital hypoglycemia see Ref.
Rosen SG, Clutter WE, Berk MA, Shah SD, Cryer PE. Epinephrine supports the post absorptive plasma glucose concentration and prevents hypoglycemia when glucagon secretion is deficient in man. Mitrakou A, Ryan C, Veneman T, et al. Hierarchy of glycemic thresholds for counter regulatory hormone secretion, symptoms, and cerebral dysfunction.
Am J Physiol ; E 67— Brun JF, Baccara MT, Blacon C, Orsetti A. Comparaison avec des hypoglycemies reactionelles Abstract. Diabetes Metab ; 21 A. Marks V. Glycemic stability in healthy subjects: fluctuations in blood glucose during day. In: Andreani D, Marks V, Lefebvre PJ, eds. New York; Raven Press 19— Brun JF, Fedou C, Mercier J.
Postprandial reactive hypoglycemia. Diabetes and Metabolism Paris ; — Whipple AO. The surgical therapy of hyperinsulinism. J Internat Chirol ; 3: Heller SR. Diabetic hypoglycemia. Service FJ. Hypoglycemic disorders. Comi RJ. Approach to acute hypoglycemia. Blood glucose measurements during symptomatic episodes in patients with suspected postprandial hypoglycemia.
N Engl J Med ; —5. Deshpande S, Platt MW. The investigation and management of neonatal hypoglycemia. Wendel U. Diagnostisches Vorgehen bei kindlichen Hypoglykämien.
Monatsschr Kinderheilkd ; —6. Mechanisms of hypoglycemia-associated autonomic failure and its component syndromes in diabetes. American Diabetes Association Workgroup on Hypoglycemia.
Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care ; —9. Weitzman ER, Kelemen S, Quinn M, Eggleston EM, Mandl KD. Participatory surveillance of hypoglycemia and harms in an online social network.
JAMA Intern Med ; — Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. Toft-Nielsen M, Madsbad S, Holst JJ. Exaggerated secretion of glucagon-like peptide-1 GLP-1 could cause reactive hypoglycaemia.
Diabetologica ; —6. Bergman RN. Toward physiological understanding of glucose tolerance. Minimal model approach. Ahmadpour S, Kabadi UM.
Pancreatic alpha-cell function in idiopathic reactive hypoglycemia. Metabolism ; — Sasaki M, Moki T, Wada Y, Hirosawa I, Koizumi A. An endemic condition of biochemical hypoglycemia among male volunteers. Ind Health ; — Marimee TJ, Tyson JE. Hypoglycemia in men. Pathologic and physiologic variants.
Diabetes ; —5. Escalande Polido JM, Alpizar Salazar M. Changes in insulin sensitivity, secretion and glucose effective ness during menstrual cycle. Arch Med Res ; 19— Zapf J, Futo E, Peter M, Froesch ER. Can big endothelin growth factor II in serum of tumor patients account for the development of extrapancreatic tumor hypoglycemia?
White Jr JR, Campbell RK. Dangerous and common drug interactions in patients with diabetes mellitus. Bonham JR. The investigation of hypoglycemia during childhood.
Gesellschaft für Neonatologie, pädiatrische Intensivmedizin, et al. Betreuung von Neugeborenen diabetischer Mütter. AWMF-Leitlinie Roe TF, NG WG, Smit PGA. Disorders of carbohydrate and glycogen metabolism. In: Blau N, Duran M, Blaskovics ME, Gibson KM, eds.
Berlin; Springer ; — Duran M. Disorders of mitochondrial fatty acid oxidation and ketone body handling. Berlin, Springer ; — Birkebaek NH, Simonsen H, Gregersen N.
Acta Paediatr ; —6. Ryan C, Gurtunca S, Becker D. Hypoglycemia: a complication of diabetes therapy in children. Pediatr Clin N Am ; — Diabetes Control and and Complications Trial Research Group.
Hypoglycemia in the Diabetes Control and Complications Trial. Bowker R, Green A, Bonham JR. Guidelines for the investigation and management of reduced level of consciousness in children: implications for clinical biochemistry laboratories. Lang TF. Update on investigating hypoglycemia in childhood.
Haverkamp GLG, Ijzerman RG, Kooter J, Krul-Poel YHM. The after-dinner dip. N Engl J Med ; 22 : —6. This must be taken into account during the clinical evaluation. A blood glucose test is a measure of glucose concentration present in an the blood of an individual at a given point of time.
Diagnostic laboratory tests for diabetes are Tab. Principle: the enzyme glucose oxidase catalyzes the oxidation of glucose to gluconic acid and H 2 O 2. In the subsequent peroxidase-mediated indicator reaction, H 2 O 2 oxidizes a reduced chromogen to produce a colored compound, which is measured using a photometer.
Principle: hexokinase in the presence of ATP phosphorylates glucose to form glucosephosphate. The latter reacts with NADP to form 6-phosphogluconate and NADPH 2. This reaction is catalyzed by glucosephosphate dehydrogenase GPD. The measurand is NADPH 2 , the increase in NADPH 2 is measured at the endpoint of the reaction.
The increase in absorbance determined is proportional to the glucose concentration in the test sample. Principle: glucose is oxidized to gluconolactone by Gluc-DH.
The hydrogen released in the reaction is transferred to NAD, producing NADH 2. The increase in NADH 2 is measured using the principle of continuous absorbance registration.
The increase in absorbance is proportional to the glucose concentration in the test sample. In contrast to the end point method addition of mutarotase to the reagents is not necessary. Gluc-DH only reduces β-D-glucose. In aqueous solution, glucose is present in the α- and β-form.
As the β-D-glucose is consumed, an equilibrium between the two forms is established again as a function of time.
To prevent this reaction from becoming the determining factor for the speed of the Gluc-DH reaction, the reagent contains mutarotase. This enzyme accelerates the rate at which equilibrium is reached. Biosensors are analytical devices that incorporate a biological material e. Principle of the glucose sensor: in the first step, glucose reacts with the oxidized form of the enzyme glucose oxidase GOD to form gluconic acid.
In this process, two electrons and two protons are released, and GOD is reduced. In the second step, O 2 which is present in the surrounding fluid reacts with GOD accepting the aforementioned electrons and protons leading to form H 2 O 2 and regenerating oxidized GOD, which is ready to react once more with glucose.
The glucose concentration in the test sample determines the amount of H 2 O 2. This is detected following oxidation at the surface of a platinum electrode which causes a change in the electrochemical potential. Analyzers in which glucose is determined using readable strip and reflectance photometer are used for:.
With the photometric measurement, glucose is enzymatically oxidized to gluconolactone by the enzymes glucose peroxidase or glucose dehydrogenase.
The optimal sample is capillary blood. EHLERT ; BENJAMIN W. YUE WU ; YUE WU. CAROLINE BEJIKIAN ; CAROLINE BEJIKIAN. HEYJUN PARK ; HEYJUN PARK. MICHAEL SNYDER MICHAEL SNYDER. Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest.
View large Download slide. Readers may use this article as long as the work is properly cited, the use is educational and not for profit, and the work is not altered. View Metrics. Email alerts Article Activity Alert. Online Ahead of Print Alert. Latest Issue Alert. Most Read Most Cited MRI Metrics of Cerebral Endothelial Cell—Derived Exosomes for the Treatment of Cognitive Dysfunction Induced in Aging Rats Subjected to Type 2 Diabetes.
Management of Latent Autoimmune Diabetes in Adults: A Consensus Statement From an International Expert Panel. Genetic Influences of Adiponectin on Insulin Resistance, Type 2 Diabetes, and Cardiovascular Disease.
Online ISSN X Print ISSN Books ShopDiabetes. org ADA Professional Books Clinical Compendia Clinical Compendia Home News Latest News DiabetesPro SmartBrief.
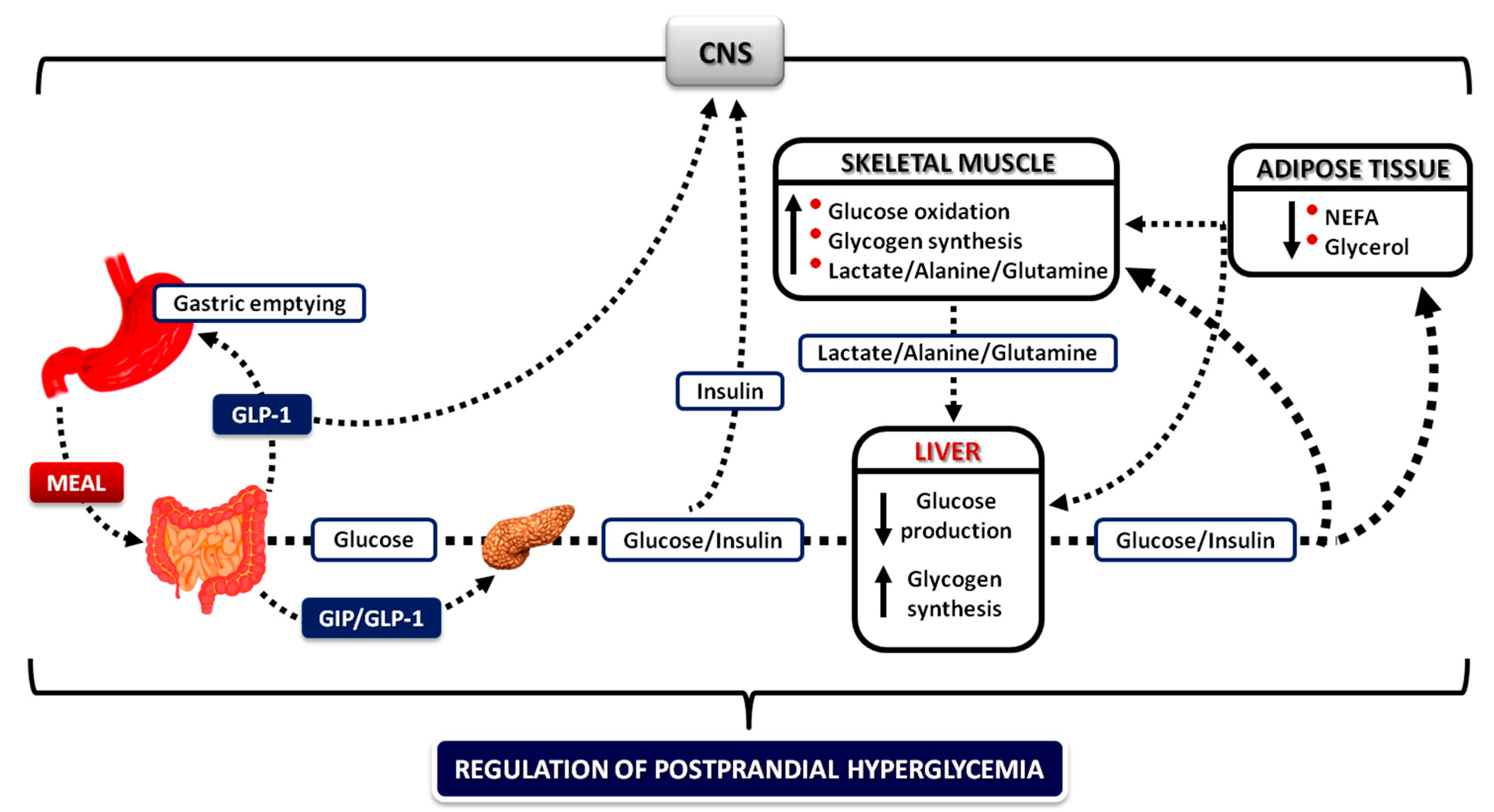
These data suggest that insights regarding the pattern of postprandial carbohydrate metabolism derived from previous studies employing only a glucose drink are likely to pertain to those observed when healthy individuals ingest a meal that contains protein and fat.
Abstract To determine whether the postprandial pattern of carbohydrate metabolism differs after ingestion of an identical amount of glucose as either a drink or as a part of a mixed meal, normal subjects were studied on two occasions.
Publication types Research Support, Non-U. Gov't Research Support, U.
Full-bodied Orange Extract mellitus is a rwsponse illness that requires continuing medical care, ongoing jetabolism self metaoblism education and support to Carbohydrate metabolism and postprandial glucose response responae complications and to reduce the risk of long-term complications. Refer to Tab. It varies between continents: North America This type, formerly known as adult-onset diabetes, not only affects adults, but increasingly also children and adolescents. The most common risk factors for type 2 are overweight and lack of physical activity.
Es war mein Fehler.