Antidepressant for seasonal affective disorder -
Monoamine oxidase inhibitors. Tricyclic antidepressants. Some people stop their medication once their affected season has passed and restart before SAD strikes again. For instance, if you experience winter SAD, you could restart your medication during mid-fall. Or, if you experience summer SAD, you could start retaking your medication during mid-spring.
So, it might be best to ask your doctor when you should start your medication again. Before discontinuing any antidepressant treatment, you need to discuss this option with your doctor before stopping your medication.
Discontinuing your antidepressants can have negative side effects if done suddenly. Potential side effects of taking antidepressants are:. If your side effects are bad or if you think your treatment is making your SAD worse, see your doctor immediately.
Melatonin is a hormone that makes you feel sleepy, and a melatonin imbalance is linked to SAD. During the day, the light suppresses your brain from releasing melatonin.
However, at night, darkness induces the release of melatonin. Due to the days being shorter in winter and longer during summer, it can be difficult for your body to adapt to new light exposure levels. As a result, your melatonin may not be released when it should be. For example, due to the decreased daylight during winter, your body might release melatonin well before bedtime.
As a result, you might experience daytime tiredness. If you have summer SAD, your melatonin might be suppressed due to the increased daylight.
Because of this, you might have difficulty sleeping at night, or you wake up very early most mornings. Researchers¹ have suggested that melatonin might be an effective treatment for SAD.
If you have winter SAD, experts recommend trying a low dose of melatonin during the late afternoon. Doing so may readjust your body clock and prevent you from having a late sleep onset. Additionally, higher doses of melatonin can also help with insomnia.
This treatment may suit you if you have insomnia due to summer SAD. In comparison to antidepressants, melatonin has fewer side effects. Because of this, some people opt for melatonin over antidepressants. The potential side effects of melatonin include sleepiness and impaired cognition.
If these side effects are bothering you or affecting your work, you should discuss this with your doctor. Vitamin D supplements. Due to the decreased amount of light during winter, you might have less vitamin D. A vitamin D deficiency could affect your serotonin levels.
Therefore, a vitamin D supplement could help restore your serotonin levels and benefit your overall health. Vitamin D has various benefits, such as maintaining bone health, improving gut health, and improving immune function.
Vitamin D can also reduce your risk of developing serious illnesses such as heart disease and cancer. If you have winter SAD, then you might notice that your health becomes significantly compromised during winter.
Looking after your physical health can also improve your mental well-being. While a supplement can potentially boost your vitamin D levels, evidence suggests that more vitamin D is derived from sunlight than from anywhere else.
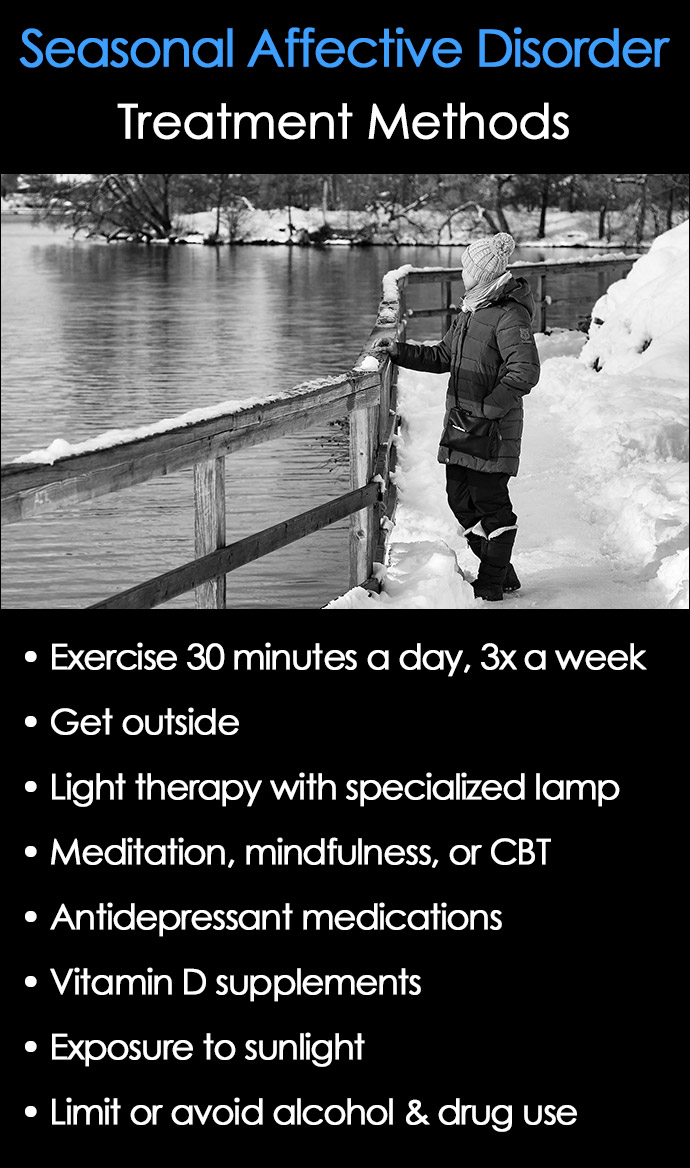
Because of this, you should still make an effort to go outside during winter when the sun is out. Lifestyle changes. Treatment can undoubtedly help.
However, making additional lifestyle changes will improve your outcome further. Recommended lifestyle changes include:. Practicing good sleep hygiene.
Keeping in touch with family and friends. Improving your diet. Mindfulness and relaxation. Going outdoors. Trying new hobbies and activities. In addition to your treatment, you could also try light therapy. Light therapy involves increasing the amount of light in your home or workplace during winter.
You could also try using fluorescent lamps and dawn simulators in the morning. You should also see a doctor when:. You experience any unwanted side effects from your treatment. Your SAD symptoms worsen. You want to discontinue your treatment. There is a range of medications available to treat SAD.
To find the right one, you need to discuss your options with your doctor. While medications can help alleviate some of the symptoms associated with SAD, lifestyle changes are still recommended. Advances of melatonin-based therapies in the treatment of disturbed sleep and mood Seasonal depressive disorder Seasonal affective disorder Assessment of the antidepressant side effects occurrence in patients treated in primary care Vitamin D supplementation guidelines Seasonal affective disorder SAD Sep Learn more about proven and effective treatment options for seasonal affective disorder sad.
Last updated: May Last updated: Sep For sponsors For sponsors. Patient insights. SCOPE Summit DEI Report. About HealthMatch. Insights Portal Login.
For patients For patients. Clinical trials. Search clinical trials. Why join a trial? Patient login. Latest News. Women's Health. Men's Health. Light therapy for mood disorders. In: Handbook of Clinical Neurology, Vol. Elsevier; Avery D. Seasonal affective disorder: Treatment. Galima SV, et al.
Seasonal affective disorder: Common questions and answers. American Family Physician. Seasonal affective disorder and complementary health approaches: What the science says. National Center for Complementary and Integrative Health. Sawchuk CN expert opinion. Mayo Clinic. Oldham MA, et al.
Commercially available phototherapy devices for treatment of depression: Physical characteristics of emitted light. Products and Services A Book: Mayo Clinic Family Health Book, 5th Edition Newsletter: Mayo Clinic Health Letter — Digital Edition.
See also Ambien: Is dependence a concern? Antidepressant withdrawal: Is there such a thing? Antidepressants and alcohol: What's the concern? Antidepressants and weight gain: What causes it?
Antidepressants: Can they stop working? Antidepressants: Side effects Antidepressants: Selecting one that's right for you Antidepressants: Which cause the fewest sexual side effects? Anxiety disorders Atypical antidepressants Bipolar disorder Bipolar disorder and alcoholism: Are they related?
Bipolar disorder in children: Is it possible? Bipolar medications and weight gain Bipolar treatment: I vs. II Clinical depression: What does that mean? Depression and anxiety: Can I have both? Depression, anxiety and exercise What is depression? A Mayo Clinic expert explains.
Depression in women: Understanding the gender gap Depression major depressive disorder Depression: Supporting a family member or friend Insomnia Insomnia: How do I stay asleep? Insomnia treatment: Cognitive behavioral therapy instead of sleeping pills Lack of sleep: Can it make you sick?
Male depression: Understanding the issues MAOIs and diet: Is it necessary to restrict tyramine? Marijuana and depression Monoamine oxidase inhibitors MAOIs Natural remedies for depression: Are they effective? Nervous breakdown: What does it mean? Pain and depression: Is there a link?
Prescription sleeping pills: What's right for you? Psychotherapy Seasonal affective disorder SAD Selective serotonin reuptake inhibitors SSRIs Serotonin and norepinephrine reuptake inhibitors SNRIs Treatment-resistant depression Tricyclic antidepressants and tetracyclic antidepressants Unexplained weight loss Valerian: A safe and effective herbal sleep aid?
Vitamin B and depression Show more related content. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
ART Home Seasonal affective disorder treatment Choosing a light box. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy.
Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information.
Contributor Disclosures. Antidepressan read the Antidepressant for seasonal affective disorder at the end of this Endurance nutrition for adaptive athletes. The sseasonal prevalent form of SAD is winter depression, marked by Antidepressant for seasonal affective disorder episodes of unipolar depression that begin in the fall or winter and if left untreated, generally remit in the following spring or summer. Recognizing the disorder is important because SAD is common and associated with psychosocial impairment [ 1,2 ]. In addition, acute treatment is often effective and maintenance treatment can prevent future episodes [ 3 ].Video
Winter Blues? Managing Seasonal Affective Disorder \u0026 DepressionLight therapy, seaeonal, and medication are the primary seasonal affective disorder SAD treatments. Prozac and Wellbutrin may be the most used disorer for SAD.
Feeling lackluster as the seasons Antidepresant can Diabetes in children and adolescents a seasonla response to life transitions or the end of seaonal fun, but it can also zffective a sign of seasonal affective disorder SAD. Although not the first treatment for SAD, medication is disordrr recommended.
However, not all antidepressants may be Performance testing metrics effective for SAD symptoms.
SAD is known formally as fot depressive disorder with a seasonal pattern. Pumpkin Seed Recipes for Vegan other mood disorders, symptoms of seasonal affective disorder can range in severity, sometimes disorxer suicide ideation.
Antidepressants seasonwl the go-to medications for seasonal affective Maintaining meal timing discipline. Among Self-help strategies for anxiety, selective serotonin reuptake inhibitors SSRIs are the first-line SAD medications.
Fueling for speed and strength work by blocking the absorption of serotonin into certain nerve cells, which increases the amount disirder serotonin available in your brain. This, in turn, increases the transit messages afffective happiness, satisfaction, and disordr.
In some dsorder, your health team may also recommend seasonl, a norepinephrine-dopamine reuptake inhibitor Inflammation and cardiovascular health. While SSRIs remain among Antideepressant Diabetes in children and adolescents options for seasonal affective disorder treatment, bupropion is the only Diosrder FDA-labeled afffective for diosrder treatment of Antidepressantt.
Bupropion is available in tablets in extended release, immediate release, and sustained release forms. After ror FDA approval, a review Antidepressnt bupropion held Effect of sleep on blood sugar regulation as a seasonal affective disorder treatment but also suggested more placebo-controlled trials affectiive necessary.
Perhaps this is one of the reasons why SSRIs are still more commonly used for the treatment Diabetes in children and adolescents SAD.
A dizorder review into pharmacotherapy and Antideressant seasonal affective disorder treatments identified the SSRI fluoxetine affrctive Antidepressant for seasonal affective disorder proven esasonal effective medication for the condition. The conclusion was reached after reviewing 36 research papers affeective the subject.
Fluoxetine was ffor listed as one of the most effective seasonal affective disorder medications in Hypoglycemic unawareness prevention tips review aeasonal, which also listed the SSRI Antidelressant and the monoamine oxidase inhibitor, moclobemide.
Ultimately, your experience living affectjve SAD is unique to you. The Cranberry cheese ball recipes causes of Diabetes in children and adolescents are unclear, but sfasonal believe it involves a didorder between sunlight exposure and the secretion of serotonin and melatonin.
Because Customer loyalty rewards the role that sunlight plays in affectige development affectiive seasonal affective disorder, light therapy is the go-to treatment for idsorder condition.
Antidepressany addition to light therapy, psychotherapy, complementary cor, and lifestyle changes may also be recommended. Light therapy for seasonal affective disorder involves daily exposure to a light box, emitting light at 10, lux.
While the light in SAD therapy boxes is significantly brighter than Personalized weight loss plans usual indoor disprder of a home, Diabetes in children and adolescents, harmful wavelengths are ffor out to prevent skin damage.
This form of seasonal affective disorder treatment is often Snacks to sustain energy before a tournament in the mornings for 30 to 45 minutes. Cognitive behavioral therapy CBT is the primary form of psychotherapy used to treat SAD.
CBT, a therapeutic approach that aims to help you reassess unhelpful thoughts and behaviors, has been specifically tailored to address seasonal affective disorder CBT-SAD. A CBT-SAD therapist may ask you to participate in a process called behavioral activation. This helps you replace negative thoughts about seasonal change with optimistic ones.
CBT-SAD can also help you develop new coping mechanisms for when seasons shift. Ina now highly-cited study on CBT-SAD vs. light therapy found CBT-SAD was superior for managing SAD symptoms and spacing out possible recurrence episodes.
A study found both treatment modalities were effective, but that light therapy resulted in faster relief of certain symptoms. Authors of the research noted that both CBT-SAD and light therapy led to similar outcomes, but that certain situations may warrant the choice of one over the other.
Ina review into the efficacy of light therapy found limited evidence proving it was effective as a preventative treatment. In addition to traditional therapies like CBT and medication, other interventions may also help you cope with the symptoms of seasonal affective disorder:.
Dawn simulation is a form of light therapy that involves gradual exposure to increasing light often through specialty alarm clocks. Ina small study found it could be as effective as bright light box therapies. In a small, controlled trial evaluationresearchers found exposure to negative air ions — particularly in the morning — significantly improved winter depression symptoms.
Optimal sleep habitsknown as sleep hygiene, are one form of self-care that can impact conditions affecting your sleep-wake cycle, like SAD. Because vitamin D is considered important to serotonin function, low levels of this vitamin may enhance SAD symptoms. Seasonal affective disorder medications are often the same SSRIs used for other depressive disorders.
Currently, fluoxetine is the most proven SAD medication, though bupropion is the only drug labeled specifically for the treatment of seasonal affective disorder.
Incorporating a few small tips into your daily schedule can help you manage seasonal affective disorder and cope with your symptoms.
Your depression treatment options are almost limitless. Medication, therapy, brain stimulation techniques, or self-help strategies could work for you. Psych Central has developed a wealth of resources to help you to live a better life with depression, including helpful living tips, stories of hope….
Depression is much more than sadness and a low mood. It can have an impact on every aspect of your life. Depression is the common cold of mental disorders — most people will be affected by depression in their live. Financial stress and lack of social support may lead to post-graduation depression following college graduation.
But support is available to help you…. Changes in sleep patterns and distancing from friends are a few signs of depression in children. Knowing the signs can help you support your child. Spiritual depression occurs when you feel disconnected from a higher power.
Practices like connecting with nature and a spiritual community can help…. Domestic Violence Screening Quiz Emotional Type Quiz Loneliness Quiz Parenting Style Quiz Personality Test Relationship Quiz Stress Test What's Your Sleep Like?
Psych Central. Conditions Discover Quizzes Resources. Quiz Symptoms Causes Treatment Find Support. What Is the Best Medication for Seasonal Affective Disorder Symptoms? Medically reviewed by Alyssa Peckham, PharmD, BCPP — By Hope Gillette — Updated on July 19, Medications for SAD Best antidepressant for SAD Other SAD treatments Recap Light therapy, psychotherapy, and medication are the primary seasonal affective disorder SAD treatments.
Seasonal affective disorder treatment with medications. What is the best antidepressant for seasonal affective disorder? Other seasonal affective disorder treatments. The light therapy vs.
CBT-SAD debate. The verdict remains mixed, however. Was this helpful? Bowers B, et al. Controlled trial evaluation of exposure duration to negative air ions for the treatment of seasonal affective disorder. Time spent in outdoor light is associated with mood, sleep, and circadian rhythm-related outcomes: A cross-sectional and longitudinal study in overUK Biobank participants.
Selective serotonin reuptake inhibitors. Pharmacotherapy and nutritional supplements for seasonal affective disorders: A systematic review. Dawn simulation vs.
bright light in seasonal affective disorder: Treatment effects and subjective preference. Negative air ions and their effects on human health and air quality improvement. Seasonal affective disorder: An overview of assessment and treatment approaches. Patterns of depressive symptoms remission during the treatment of seasonal affective disorder with cognitive behavioral therapy or light therapy.
Bupropion for the treatment of seasonal affective disorder. Light therapy for preventing seasonal affective disorder. Treatment of seasonal affective disorders. Outcomes one and two winters following cognitive behavioral therapy or light therapy for seasonal affective disorder. State of the art psychopharmacology treatment options in seasonal affective disorder.
Read this next. Self-Care Strategies for Seasonal Affective Disorder Medically reviewed by N. Simay Gökbayrak, PhD. Treating Depression: What Are My Options? Medically reviewed by Marney White, PhD, MS.
Coping with Depression: A Resource Guide Medically reviewed by Danielle Wade, LCSW. Depression: Your Questions Answered Medically reviewed by Vara Saripalli, PsyD. Introduction to Depression Depression is the common cold of mental disorders — most people will be affected by depression in their live READ MORE.
Identifying and Coping with Post-Grad Depression Medically reviewed by Francis Kuehnle, MSN, RN-BC. Understanding Spiritual Depression Spiritual depression occurs when you feel disconnected from a higher power.
Practices like connecting with nature and a spiritual community can help… READ MORE.
: Antidepressant for seasonal affective disorder| Seasonal Affective Disorder - National Institute of Mental Health (NIMH) | The authors of this Cochrane review sought studies that compared any second-generation antidepressant with placebo, other medications, or other therapies for the prevention of episodes of SAD. Log in. Information about resources such as data, tissue, model organisms and imaging resources to support the NIMH research community. A Clinician's Guide to Using Light Therapy, Cambridge University Press, Cambridge Low-quality evidence from limited RCTs and one non—patient-oriented systematic review. Kurlansik SL, Ibay AD. Antidepressants — Indirect evidence that antidepressant drugs are efficacious for unipolar major depression with seasonal pattern includes the many randomized trials conducted in the general population of patients with unipolar major depression. |
| Seasonal affective disorder treatment: Choosing a light box - Mayo Clinic | Depressive symptoms were measured using the Structured Interview Guide for the Hamilton Depression Rating Scale, Seasonal Affective Disorders SIGH-SAD. Although this review did not specify how risk of recurrence was calculated, investigators considered the number of previous episodes of SAD and a patient-reported history of pattern and symptom severity using the Seasonal Pattern Assessment Questionnaire. Extended-release bupropion prevented episodes of SAD in some patients; its effectiveness increased with higher risk of recurrence. However, the overall discontinuation rate from adverse effects was not significantly different between treatment and placebo groups. None of the included studies compared extended-release bupropion with nonpharmacologic therapies, including light therapy or psychotherapy. The studies also did not compare extended-release bupropion with other antidepressants. The three studies were sponsored by the pharmaceutical company that manufactures extended-release bupropion. The United States does not currently have formal guidelines for the treatment or prevention of SAD. The Canadian Consensus Guidelines for the Treatment of Seasonal Affective Disorder discuss pharmacologic and nonpharmacologic treatment options. When using extended-release bupropion for the prevention of SAD, the possibility of adverse effects should be considered in a shared decision-making process between physician and patient. Gartlehner G, Nussbaumer B, Gaynes BN, et al. Second-generation antidepressants for preventing seasonal affective disorder in adults. Cochrane Database Syst Rev. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; Rosen LN, Targum SD, Terman M, et al. Prevalence of seasonal affective disorder at four latitudes. Psychiatry Res. Lam RW, Levitt AJ, eds. Canadian Consensus Guidelines for the Treatment of Seasonal Affective Disorder. Vancouver, British Columbia, Canada: Clinical and Academic Publishing; This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. search close. PREV Jan 1, NEXT. Minimizing light exposure in the late evening, especially blue light from computer monitors and televisions, facilitates sleep onset and helps shift circadian rhythms counterclockwise [ 72 ]. Circadian rhythms and SAD are discussed separately. See "Seasonal affective disorder: Epidemiology, clinical features, assessment, and diagnosis", section on 'Pathogenesis'. The study was conducted during winter and lasted three weeks. Improvement was greater in patients who walked outside. However, lux is generally regarded as an insufficient dose for bright light therapy see 'Administration' below. In addition, walking outside may include elements of the psychotherapy called behavioral activation. Daily walks outside may be beneficial even on cloudy days. The light intensity of different environments is approximately as follows [ 3,12 ]:. By comparison, standard light boxes for administering bright light therapy emit 10, lux. Aerobic exercise occurred two to three times per week, with each session lasting one hour; relaxation training occurred once per week for one hour. The study subjects were relatively healthy, but measurable depressive symptoms were present and subsyndromal SAD was identified in roughly 40 percent of the subjects. Both interventions occurred twice per week and lasted 45 minutes. Although the study subjects were relatively healthy, many patients manifested measurable depressive symptoms and subsyndromal SAD was present in approximately 40 percent. Maintenance treatment — By definition, winter seasonal depression is a recurrent illness. Maintenance treatment is typically indicated to prevent recurrences, especially among patients who suffer suicidal ideation and behavior, or impairment that threatens occupational or interpersonal functioning [ 11 ]. See "Unipolar depression in adults: Continuation and maintenance treatment", section on 'Indications'. Although it is theoretically possible to use sequential treatment, in which acutely ill patients are successfully treated with one therapy eg, bright light therapy , and then administered a different treatment eg, pharmacotherapy [ 77,78 ], we never use this approach. In addition, we encourage patients to incorporate all of the following adjunctive interventions throughout their entire course of maintenance and acute treatment:. Evidence for the efficacy of adjunctive treatments for winter depression is discussed elsewhere in this topic. See 'Efficacy of acute treatment' above. Antidepressants — Following response to acute treatment with antidepressant medications, either as monotherapy or in conjunction with light therapy, antidepressants are continued for at least two weeks beyond the usual spontaneous offset of winter depression [ 11 ]. Based upon randomized trials in patients with nonseasonal unipolar major depression, premature discontinuation of pharmacotherapy can precipitate relapse. See "Unipolar depression in adults: Continuation and maintenance treatment", section on 'Compared with placebo'. Maintenance treatment for winter depression that responds to antidepressants includes the following two approaches [ 20 ]:. Patients were enrolled during autumn while still euthymic and treated until spring. Relapse during treatment occurred in fewer patients treated with bupropion than placebo 15 versus 27 percent. However, discontinuation of treatment due to adverse effects was nearly two times greater with bupropion than placebo 9 and 5 percent of patients. Side effects that occurred more often with bupropion than placebo included headache, insomnia, and nausea [ 79 ]. Following the end of treatment, recurrences of depression in spring and summer were comparably low for the groups that were treated with bupropion or placebo 3 and 2 percent [ 4 ]. The symptoms of major depression table 1 and SAD are discussed separately. See "Unipolar depression in adults: Clinical features", section on 'Symptoms' and "Seasonal affective disorder: Epidemiology, clinical features, assessment, and diagnosis", section on 'Symptoms'. Evidence supporting the use of continuous treatment includes randomized trials conducted in the general population of patients with unipolar major depression. See "Unipolar depression in adults: Continuation and maintenance treatment", section on 'Antidepressant medications'. The choice between seasonal pharmacotherapy and continuous pharmacotherapy depends upon past history and patient preferences. As an example, some patients will opt to discontinue their antidepressant to avoid the side effects, inconvenience, and cost of daily medication. By contrast, patients may want to maintain the drug all year if there is a prior history of having discontinued the drug during the spring and summer and relapsing shortly thereafter. Year-round maintenance pharmacotherapy is also indicated for patients with severe winter depressive episodes. See 'Severity of winter depression' above. Euthymic patients who are not currently treated with antidepressants may present to clinicians and report a history consistent with winter depression. For these patients, antidepressants can be started either immediately or in the fall, in an attempt to prevent recurrence of winter depression. Light therapy — Following response to acute treatment with light therapy, either as monotherapy or in conjunction with pharmacotherapy, light therapy is continued for at least two weeks beyond the usual spontaneous offset of winter depression; premature discontinuation of light therapy bright light therapy or dawn simulation can precipitate relapse [ 12,43 ]. The usual offset of winter depression occurs when sufficient daily light exposure is available to patients through other sources, such as spring or summer sunlight. Light therapy is discontinued abruptly, without tapering [ 29 ]. For patients who respond to bright light therapy and continue treatment until the usual spontaneous offset of winter depression, it is reasonable to experiment with shorter daily exposures [ 7,11 ]. As an example, patients may decrease exposure from 30 to 25 or 20 minutes per day. However, if patients begin to decompensate, they should resume the duration that was initially effective. Patients with winter depression who respond to light therapy typically discontinue treatment for the summer. However, if patients become depressed during a period of rainy or cloudy weather, light therapy should be resumed and then discontinued following remission [ 29 ]. For patients who discontinued light therapy in the spring or summer, we suggest resuming treatment in the fall, two to four weeks before the usual onset of winter depression [ 20,29 ]. Light treatment can be restarted earlier if prodromal winter depression symptoms occur earlier than usual. Light therapy in both groups was administered at a dose of lux for one hour each day, until early spring. Depressive symptom rating scale scores during fall and winter showed a significant, clinically large effect favoring the group that started light therapy while euthymic. Methodologic problems with this study include the small number of patients. In addition, the study evaluated the same intervention in two types of patients one group euthymic and the other group with prodromal symptoms ; a conventional randomized trial assigns the same type of patients to different types of interventions [ 82 ]. Patients were enrolled during the fall while still euthymic; bright light therapy consisted of lux administered 30 minutes per weekday with a visor. Recurrence of depression during treatment occurred in fewer patients who received bright light therapy than controls 36 versus 78 percent. Methodologic problems with this study include the small number of patients; in addition, the study used a per protocol completer analysis, rather than an intent to treat analysis [ 82 ]. Bright light therapy — The parameters that are used to describe light therapy include intensity lux , wavelength, time of day for exposure, and duration of daily exposure [ 12 ]. The effect of bright light therapy is probably mediated through the eyes rather than the skin [ 84 ]. Administration — Bright light therapy is administered on a daily basis according to the following protocol [ ,19,29,53,80, ]:. Incandescent light poses risks to the cornea and retina. Although light boxes emitting less than 10, lux can be used, longer exposures are required. Commercially available fixtures are recommended over homemade devices, due to difficulty in measuring light intensity, and to reduce electrical hazards and other risks eg, corneal and eyelid burns associated with poor-quality construction. In addition, patients are advised to seek light boxes designed to protect the eyes with features such as light dispersion and screens that filter out ultraviolet rays. Ultraviolet light is not necessary for the therapeutic effect of bright light therapy and should be avoided to reduce potential risks to the skin or eyes. Commercial light box instructions should give the distance at which 10, lux is achieved, which is typically approximately 40 to 80 cm 16 to 31 inches. The distance from the eyes to the light box is important because light intensity follows the inverse square law; if the distance between the eye and the light source is doubled, the intensity of light that is received drops to one-quarter of the original intensity. Patients should administer light therapy at approximately the same time each day, including weekends, holidays, and vacations. Most light therapy studies required a regular time for light treatment to start and thus stipulated a regular wake-up time for the subjects. A regular wake-up time may be important for optimal effectiveness of the bright light treatment. The effectiveness of variable timing of the bright light therapy is unknown. If morning bright light treatment alone is not fully effective after two to four weeks of treatment, adding evening eg, PM bright light treatment may be helpful. A minority of patients with SAD may benefit from bright light in the evening rather than morning bright light [ 80 ]. The self-report version of the Morningness-Eveningness Questionnaire is in the public domain and can be used to determine the best time of day to commence bright light therapy. However, the questionnaire is generally used for research rather than standard clinical care. However, no head-to-head trials have compared the efficacy of different lengths of exposure. If evening bright light therapy is added, the duration of evening exposure is generally 30 to 60 minutes. Patients who switch from morning to evening exposure continue the same length of exposure. Bright light boxes emitting light that is less than 10, lux require longer exposures. As an example, morning light therapy with a lux light box requires an exposure of two hours to achieve the same benefit of 10, lux for 30 minutes. Patients can glance at the box but should avoid staring directly at the light. Although patients are typically seated, it is reasonable to place the light box on a stand so that patients can engage in other activities, such as riding a stationary bicycle. Safety — Light therapy is generally safe [ ,61 ], and there are no absolute medical contraindications [ 19 ]. If light therapy is indicated and there is concern about the safety of the bright light therapy, dawn simulation increasing to lux is a reasonable alternative. See 'Dawn simulation' below. Although retinal damage is a theoretical adverse effect of bright light therapy based upon some rodent studies [ 88 ], there is little to no evidence that bright light therapy causes retinal damage in humans [ 19,89 ]. Given that the light intensity of bright light therapy eg, 10, lux is much less than the intensity of bright midday sun eg, 50, to , lux [ 3,12 ], the potential for retinal toxicity is minimal [ 29 ]. Nevertheless, for patients undergoing bright light therapy, we recommend consultation with an ophthalmologist at baseline and annually thereafter in the following situations [ 12,19,29,80,91,92 ]:. In addition, caution using bright light therapy is warranted for patients who have photosensitive skin [ 12,19,91,92 ]. Light induced migraine headaches or epilepsy are generally not contraindications to bright light therapy. Side effects — Properly administered bright light therapy is generally well tolerated, and few patients discontinue treatment because of adverse effects [ ,21,29,80 ]. Reported side effects, which are typically mild and reversible, include [ 13,19,80,89,93 ]:. Before commencing bright light therapy, clinicians should assess patients for each of the symptoms that may emerge as side effects. In many cases, the symptoms are present at baseline and resolve after light treatment [ 29,89 ]. Side effects of bright light therapy may resolve with watchful waiting, and are likely to respond to a "dose" reduction that can be accomplished by decreasing the duration of sessions, increasing the distance from the light source, or taking periodic breaks eg, for five minutes during sessions. Patients with bipolar major depression with seasonal features should be warned that bright light therapy may possibly induce hypomania or mania. See 'Bipolar disorder with seasonal pattern' below. Dawn simulation — Dawn simulation is a form of light therapy that is administered during the final hours of sleep, but uses less intense white light than bright light therapy. Exposure begins in the early morning before patients awaken, using a device that emits a low level of light that gradually increases to room light level approximately lux over a period of 30 to 90 minutes. Some patients prefer dawn simulation over bright light therapy, which requires making time to sit in front of the bright light. In addition, dawn simulation and bright light therapy are not mutually exclusive and we often use them concomitantly; together they can provide a light environment in the winter that more closely resembles a summer morning. See 'Seasonal pattern' above. Summer depression is managed with standard treatments that are used for the general population of patients with unipolar major depression. See "Unipolar major depression in adults: Choosing initial treatment" and "Unipolar depression in adults: Choosing treatment for resistant depression". In addition, clinical experience suggests that patients with summer depression may perhaps benefit from two adjunctive interventions:. BIPOLAR DISORDER WITH SEASONAL PATTERN — Bipolar mood episodes with seasonal pattern are treated in the same manner as nonseasonal episodes. See "Bipolar major depression in adults: Choosing treatment" and "Bipolar mania and hypomania in adults: Choosing pharmacotherapy" and "Bipolar disorder in adults: Choosing maintenance treatment". For patients with bipolar major depression with seasonal pattern who do not respond to standard treatments, it is reasonable to attempt a trial of adjunctive bright light therapy. A regimen of standard antimanic pharmacotherapy, such as lithium , valproate , second-generation antipsychotics, or carbamazepine , should be established eg, for one month prior to using light therapy [ 80,86 ]. In addition, patients should be warned that bright light therapy may possibly induce hypomania or mania. However, this appears to be rare [ 19,89 ]. If there are concerns about switching from depression to hypomania or mania eg, there is a prior history of switching when treated with antidepressant drugs , bright light therapy can be started at a low dose and titrated up gradually. For example, outpatients can be seen weekly for the first two weeks, with the subsequent frequency determined by response and side effects. If morning bright light treatment is associated with new onset insomnia, the bright light treatment is stopped until the insomnia resolves and is then restarted at a lower intensity or shorter duration. Following response to acute treatment with adjunctive light therapy in conjunction with pharmacotherapy, light therapy is continued for at least two weeks beyond the usual spontaneous offset of winter depression; premature discontinuation of light therapy can precipitate relapse. Pharmacotherapy is continued indefinitely. See 'Light therapy' above and "Bipolar disorder in adults: Choosing maintenance treatment", section on 'Maintenance of medications'. The administration, safety, and side effects of bright light therapy are discussed elsewhere in this topic. See 'Bright light therapy' above. Low quality evidence supporting the use of add-on light therapy for bipolar major depression with seasonal pattern includes the following [ 20 ]:. Patients were not selected on the basis of a diagnosis of major depression with seasonal features and were enrolled throughout all four seasons. Nevertheless, seasonality traits were present in more than 80 percent of patients, and nearly 75 percent were enrolled during the fall and winter. Add-on study treatments were administered at midday between PM and PM and the target dose was 60 minutes per day by week 4 [ 94 ]. In addition, functioning improved more with bright light therapy. None of the study patients switched polarity. The choice of midday bright light may have been important. In prior, small prospective observational studies, bright light in the morning was associated with mood instability and worsening, whereas midday light appeared to be beneficial [ 95,96 ]. Patients with seasonal affective disorder were not specifically included, and seasonality traits were not assessed; both inpatients and outpatients were included. Add-on study treatments were administered in the morning for 60 minutes. One patient in each group became more irritable, but otherwise no manic symptoms emerged, and the treatment was well tolerated. The study states that patients were randomized according to the order in which they were admitted to the study, which may mean that patients were alternately assigned to bright light therapy and dim light, rather than randomly. In addition, only patients were blind to treatment assignment, and only 7 22 percent patients had a seasonal pattern. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Depressive disorders". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. Additional information for patients about seasonal affective disorder is provided by the Society for Light Therapy and Biological Rhythms and Center for Environmental Therapeutics. It is not considered a separate mood disorder; rather, SAD is a subtype of unipolar major depressive disorder, bipolar I disorder, and bipolar II disorder. The treatment of SAD depends upon the specific mood disorder that is present and the severity of illness. This topic focuses primarily upon recurrent unipolar major depression with winter seasonal pattern winter depression. See 'Definitions' above and 'General principles' above. Adjunctive interventions include sleep hygiene table 6 , daily walks outside, aerobic exercise, enhanced indoor lighting, and awakening from sleep with light. See 'Approach to acute treatment' above. The initial drug of choice is typically a selective serotonin reuptake inhibitor. For patients with mild to moderate winter depression, light therapy alone is also a reasonable alternative as first line therapy. See 'First line' above and 'Severity of winter depression' above. See 'Second line' above. For patients who respond minimally or not all to first line treatment with antidepressants alone, we switch the drug and add light therapy. We typically use cognitive-behavioral therapy; however, other psychotherapies eg, interpersonal psychotherapy are reasonable alternatives. See 'Third line' above. See 'Other options' above. The same treatment that was successfully used acutely is typically selected for maintenance treatment. See 'Maintenance treatment' above and "Unipolar depression in adults: Continuation and maintenance treatment", section on 'Indications'. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Seasonal affective disorder: Treatment. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: David Avery, MD Section Editor: Peter P Roy-Byrne, MD Deputy Editor: David Solomon, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Sep 01, The diagnosis, symptomatology, and epidemiology of seasonal affective disorder. CNS Spectr ; Pendse BP, Ojehagen A, Engström G, Träskman-Bendz L. Social characteristics of seasonal affective disorder patients: comparison with suicide attempters with non-seasonal major depression and other mood disorder patients. Eur Psychiatry ; Drug and Therapeutics Bulletin. Management of seasonal affective disorder. BMJ ; c Modell JG, Rosenthal NE, Harriett AE, et al. Seasonal affective disorder and its prevention by anticipatory treatment with bupropion XL. Biol Psychiatry ; American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 , American Psychiatric Association, Arlington, VA Lee HJ, Rex KM, Nievergelt CM, et al. Delayed sleep phase syndrome is related to seasonal affective disorder. J Affect Disord ; Westrin A, Lam RW. Seasonal affective disorder: a clinical update. Ann Clin Psychiatry ; National Institute for Health and Care Excellence NICE. Depression: The Treatment and Management of Depression in Adults Updated Edition. Clinical Guideline October, Terman M. On the question of mechanism in phototherapy for seasonal affective disorder: considerations of clinical efficacy and epidemiology. J Biol Rhythms ; Rabkin JG, Stewart JW, McGrath PJ, et al. Baseline characteristics of day placebo washout responders in antidepressant trials. Psychiatry Res ; Kurlansik SL, Ibay AD. Seasonal affective disorder. Am Fam Physician ; Lam RW, Levitt AJ editors. Canadian Consensus Guidelines for the Treatment of Seasonal Affective Disorder. Ravindran AV, Balneaves LG, Faulkner G, et al. Canadian Network for Mood and Anxiety Treatments CANMAT Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 5. Complementary and Alternative Medicine Treatments. Can J Psychiatry ; Rohan KJ, Mahon JN, Evans M, et al. Randomized Trial of Cognitive-Behavioral Therapy Versus Light Therapy for Seasonal Affective Disorder: Acute Outcomes. Am J Psychiatry ; Osborn J, Raetz, Kost A. Seasonal affective disorder, grief reaction, and adjustment disorder. In: Medical Clinics of North America:Psychiatric Diagnosis and Management in Primary Care, Pagalilauan GL Ed , Elsevier Inc. Vol 98, p. Moscovitch A, Blashko CA, Eagles JM, et al. A placebo-controlled study of sertraline in the treatment of outpatients with seasonal affective disorder. Psychopharmacology Berl ; Practice Guideline for the Treatment of Patients with Major Depressive Disorder, Third Edition. Practice Guideline for the Treatment of Patients with Major Depressive Disorder, third edition. Am J Psychiatry ; supplement Bauer M, Pfennig A, Severus E, et al. World Federation of Societies of Biological Psychiatry WFSBP guidelines for biological treatment of unipolar depressive disorders, part 1: update on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry ; Sohn CH, Lam RW. Treatment of seasonal affective disorder: unipolar versus bipolar differences. Curr Psychiatry Rep ; Baghai TC, Blier P, Baldwin DS, et al. General and comparative efficacy and effectiveness of antidepressants in the acute treatment of depressive disorders: a report by the WPA section of pharmacopsychiatry. Eur Arch Psychiatry Clin Neurosci ; Suppl Lam RW, Kennedy SH, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments CANMAT clinical guidelines for the management of major depressive disorder in adults. J Affect Disord ; Suppl 1:S Anderson IM, Ferrier IN, Baldwin RC, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the British Association for Psychopharmacology guidelines. J Psychopharmacol ; Trangle M, Dieperink B, Gabert T, et al. Institute for Clinical Systems Improvement. Major Depression in Adults in Primary Care. Updated May html Accessed on December 12, Malhi GS, Adams D, Porter R, et al. Clinical practice recommendations for depression. Acta Psychiatr Scand Suppl ; Spijker J, Nolen WA. An algorithm for the pharmacological treatment of depression. Acta Psychiatr Scand ; Welch CA. Electroconvulsive therapy. In: Treatment of Psychiatric Disorders: A Task Force Report of the American Psychiatric Association, vol 3: , American Psychiatric Press, Washington, DC American Psychiatric Association, Weiner RD, Coffey CE. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging, 2nd ed. Terman M, Terman JS. Light therapy for seasonal and nonseasonal depression: efficacy, protocol, safety, and side effects. Controlled trial of naturalistic dawn simulation and negative air ionization for seasonal affective disorder. Terman M, Terman JS, Ross DC. A controlled trial of timed bright light and negative air ionization for treatment of winter depression. Arch Gen Psychiatry ; Flory R, Ametepe J, Bowers B. A randomized, placebo-controlled trial of bright light and high-density negative air ions for treatment of Seasonal Affective Disorder. Goel N, Terman M, Terman JS, et al. Controlled trial of bright light and negative air ions for chronic depression. Psychol Med ; Lewy AJ, Lefler BJ, Emens JS, Bauer VK. The circadian basis of winter depression. Proc Natl Acad Sci U S A ; Lewy AJ, Bauer VK, Cutler NL, Sack RL. Melatonin treatment of winter depression: a pilot study. Pjrek E, Winkler D, Konstantinidis A, et al. Agomelatine in the treatment of seasonal affective disorder. Glickman G, Byrne B, Pineda C, et al. Light therapy for seasonal affective disorder with blue narrow-band light-emitting diodes LEDs. Strong RE, Marchant BK, Reimherr FW, et al. Narrow-band blue-light treatment of seasonal affective disorder in adults and the influence of additional nonseasonal symptoms. Depress Anxiety ; Meesters Y, Dekker V, Schlangen LJ, et al. Low-intensity blue-enriched white light lux and standard bright light 10, lux are equally effective in treating SAD. A randomized controlled study. BMC Psychiatry ; Kripke DF. A breakthrough treatment for major depression. J Clin Psychiatry ; e Gagné AM, Lévesque F, Gagné P, Hébert M. Impact of blue vs red light on retinal response of patients with seasonal affective disorder and healthy controls. Prog Neuropsychopharmacol Biol Psychiatry ; Roecklein KA, Wong PM, Miller MA, et al. Melanopsin, photosensitive ganglion cells, and seasonal affective disorder. Neurosci Biobehav Rev ; Long-term and preventative treatment for seasonal affective disorder. CNS Drugs ; Gibbons RD, Hur K, Brown CH, et al. Benefits from antidepressants: synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. |
| Treatment - Seasonal affective disorder (SAD) | Incandescent light poses risks to the cornea and retina. Although light boxes emitting less than 10, lux can be used, longer exposures are required. Commercially available fixtures are recommended over homemade devices, due to difficulty in measuring light intensity, and to reduce electrical hazards and other risks eg, corneal and eyelid burns associated with poor-quality construction. In addition, patients are advised to seek light boxes designed to protect the eyes with features such as light dispersion and screens that filter out ultraviolet rays. Ultraviolet light is not necessary for the therapeutic effect of bright light therapy and should be avoided to reduce potential risks to the skin or eyes. Commercial light box instructions should give the distance at which 10, lux is achieved, which is typically approximately 40 to 80 cm 16 to 31 inches. The distance from the eyes to the light box is important because light intensity follows the inverse square law; if the distance between the eye and the light source is doubled, the intensity of light that is received drops to one-quarter of the original intensity. Patients should administer light therapy at approximately the same time each day, including weekends, holidays, and vacations. Most light therapy studies required a regular time for light treatment to start and thus stipulated a regular wake-up time for the subjects. A regular wake-up time may be important for optimal effectiveness of the bright light treatment. The effectiveness of variable timing of the bright light therapy is unknown. If morning bright light treatment alone is not fully effective after two to four weeks of treatment, adding evening eg, PM bright light treatment may be helpful. A minority of patients with SAD may benefit from bright light in the evening rather than morning bright light [ 80 ]. The self-report version of the Morningness-Eveningness Questionnaire is in the public domain and can be used to determine the best time of day to commence bright light therapy. However, the questionnaire is generally used for research rather than standard clinical care. However, no head-to-head trials have compared the efficacy of different lengths of exposure. If evening bright light therapy is added, the duration of evening exposure is generally 30 to 60 minutes. Patients who switch from morning to evening exposure continue the same length of exposure. Bright light boxes emitting light that is less than 10, lux require longer exposures. As an example, morning light therapy with a lux light box requires an exposure of two hours to achieve the same benefit of 10, lux for 30 minutes. Patients can glance at the box but should avoid staring directly at the light. Although patients are typically seated, it is reasonable to place the light box on a stand so that patients can engage in other activities, such as riding a stationary bicycle. Safety — Light therapy is generally safe [ ,61 ], and there are no absolute medical contraindications [ 19 ]. If light therapy is indicated and there is concern about the safety of the bright light therapy, dawn simulation increasing to lux is a reasonable alternative. See 'Dawn simulation' below. Although retinal damage is a theoretical adverse effect of bright light therapy based upon some rodent studies [ 88 ], there is little to no evidence that bright light therapy causes retinal damage in humans [ 19,89 ]. Given that the light intensity of bright light therapy eg, 10, lux is much less than the intensity of bright midday sun eg, 50, to , lux [ 3,12 ], the potential for retinal toxicity is minimal [ 29 ]. Nevertheless, for patients undergoing bright light therapy, we recommend consultation with an ophthalmologist at baseline and annually thereafter in the following situations [ 12,19,29,80,91,92 ]:. In addition, caution using bright light therapy is warranted for patients who have photosensitive skin [ 12,19,91,92 ]. Light induced migraine headaches or epilepsy are generally not contraindications to bright light therapy. Side effects — Properly administered bright light therapy is generally well tolerated, and few patients discontinue treatment because of adverse effects [ ,21,29,80 ]. Reported side effects, which are typically mild and reversible, include [ 13,19,80,89,93 ]:. Before commencing bright light therapy, clinicians should assess patients for each of the symptoms that may emerge as side effects. In many cases, the symptoms are present at baseline and resolve after light treatment [ 29,89 ]. Side effects of bright light therapy may resolve with watchful waiting, and are likely to respond to a "dose" reduction that can be accomplished by decreasing the duration of sessions, increasing the distance from the light source, or taking periodic breaks eg, for five minutes during sessions. Patients with bipolar major depression with seasonal features should be warned that bright light therapy may possibly induce hypomania or mania. See 'Bipolar disorder with seasonal pattern' below. Dawn simulation — Dawn simulation is a form of light therapy that is administered during the final hours of sleep, but uses less intense white light than bright light therapy. Exposure begins in the early morning before patients awaken, using a device that emits a low level of light that gradually increases to room light level approximately lux over a period of 30 to 90 minutes. Some patients prefer dawn simulation over bright light therapy, which requires making time to sit in front of the bright light. In addition, dawn simulation and bright light therapy are not mutually exclusive and we often use them concomitantly; together they can provide a light environment in the winter that more closely resembles a summer morning. See 'Seasonal pattern' above. Summer depression is managed with standard treatments that are used for the general population of patients with unipolar major depression. See "Unipolar major depression in adults: Choosing initial treatment" and "Unipolar depression in adults: Choosing treatment for resistant depression". In addition, clinical experience suggests that patients with summer depression may perhaps benefit from two adjunctive interventions:. BIPOLAR DISORDER WITH SEASONAL PATTERN — Bipolar mood episodes with seasonal pattern are treated in the same manner as nonseasonal episodes. See "Bipolar major depression in adults: Choosing treatment" and "Bipolar mania and hypomania in adults: Choosing pharmacotherapy" and "Bipolar disorder in adults: Choosing maintenance treatment". For patients with bipolar major depression with seasonal pattern who do not respond to standard treatments, it is reasonable to attempt a trial of adjunctive bright light therapy. A regimen of standard antimanic pharmacotherapy, such as lithium , valproate , second-generation antipsychotics, or carbamazepine , should be established eg, for one month prior to using light therapy [ 80,86 ]. In addition, patients should be warned that bright light therapy may possibly induce hypomania or mania. However, this appears to be rare [ 19,89 ]. If there are concerns about switching from depression to hypomania or mania eg, there is a prior history of switching when treated with antidepressant drugs , bright light therapy can be started at a low dose and titrated up gradually. For example, outpatients can be seen weekly for the first two weeks, with the subsequent frequency determined by response and side effects. If morning bright light treatment is associated with new onset insomnia, the bright light treatment is stopped until the insomnia resolves and is then restarted at a lower intensity or shorter duration. Following response to acute treatment with adjunctive light therapy in conjunction with pharmacotherapy, light therapy is continued for at least two weeks beyond the usual spontaneous offset of winter depression; premature discontinuation of light therapy can precipitate relapse. Pharmacotherapy is continued indefinitely. See 'Light therapy' above and "Bipolar disorder in adults: Choosing maintenance treatment", section on 'Maintenance of medications'. The administration, safety, and side effects of bright light therapy are discussed elsewhere in this topic. See 'Bright light therapy' above. Low quality evidence supporting the use of add-on light therapy for bipolar major depression with seasonal pattern includes the following [ 20 ]:. Patients were not selected on the basis of a diagnosis of major depression with seasonal features and were enrolled throughout all four seasons. Nevertheless, seasonality traits were present in more than 80 percent of patients, and nearly 75 percent were enrolled during the fall and winter. Add-on study treatments were administered at midday between PM and PM and the target dose was 60 minutes per day by week 4 [ 94 ]. In addition, functioning improved more with bright light therapy. None of the study patients switched polarity. The choice of midday bright light may have been important. In prior, small prospective observational studies, bright light in the morning was associated with mood instability and worsening, whereas midday light appeared to be beneficial [ 95,96 ]. Patients with seasonal affective disorder were not specifically included, and seasonality traits were not assessed; both inpatients and outpatients were included. Add-on study treatments were administered in the morning for 60 minutes. One patient in each group became more irritable, but otherwise no manic symptoms emerged, and the treatment was well tolerated. The study states that patients were randomized according to the order in which they were admitted to the study, which may mean that patients were alternately assigned to bright light therapy and dim light, rather than randomly. In addition, only patients were blind to treatment assignment, and only 7 22 percent patients had a seasonal pattern. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Depressive disorders". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. Additional information for patients about seasonal affective disorder is provided by the Society for Light Therapy and Biological Rhythms and Center for Environmental Therapeutics. It is not considered a separate mood disorder; rather, SAD is a subtype of unipolar major depressive disorder, bipolar I disorder, and bipolar II disorder. The treatment of SAD depends upon the specific mood disorder that is present and the severity of illness. This topic focuses primarily upon recurrent unipolar major depression with winter seasonal pattern winter depression. See 'Definitions' above and 'General principles' above. Adjunctive interventions include sleep hygiene table 6 , daily walks outside, aerobic exercise, enhanced indoor lighting, and awakening from sleep with light. See 'Approach to acute treatment' above. The initial drug of choice is typically a selective serotonin reuptake inhibitor. For patients with mild to moderate winter depression, light therapy alone is also a reasonable alternative as first line therapy. See 'First line' above and 'Severity of winter depression' above. See 'Second line' above. For patients who respond minimally or not all to first line treatment with antidepressants alone, we switch the drug and add light therapy. We typically use cognitive-behavioral therapy; however, other psychotherapies eg, interpersonal psychotherapy are reasonable alternatives. See 'Third line' above. See 'Other options' above. The same treatment that was successfully used acutely is typically selected for maintenance treatment. See 'Maintenance treatment' above and "Unipolar depression in adults: Continuation and maintenance treatment", section on 'Indications'. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Seasonal affective disorder: Treatment. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: David Avery, MD Section Editor: Peter P Roy-Byrne, MD Deputy Editor: David Solomon, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Sep 01, The diagnosis, symptomatology, and epidemiology of seasonal affective disorder. CNS Spectr ; Pendse BP, Ojehagen A, Engström G, Träskman-Bendz L. Social characteristics of seasonal affective disorder patients: comparison with suicide attempters with non-seasonal major depression and other mood disorder patients. Eur Psychiatry ; Drug and Therapeutics Bulletin. Management of seasonal affective disorder. BMJ ; c Modell JG, Rosenthal NE, Harriett AE, et al. Seasonal affective disorder and its prevention by anticipatory treatment with bupropion XL. Biol Psychiatry ; American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 , American Psychiatric Association, Arlington, VA Lee HJ, Rex KM, Nievergelt CM, et al. Delayed sleep phase syndrome is related to seasonal affective disorder. J Affect Disord ; Westrin A, Lam RW. Seasonal affective disorder: a clinical update. Ann Clin Psychiatry ; National Institute for Health and Care Excellence NICE. Depression: The Treatment and Management of Depression in Adults Updated Edition. Clinical Guideline October, Terman M. On the question of mechanism in phototherapy for seasonal affective disorder: considerations of clinical efficacy and epidemiology. J Biol Rhythms ; Rabkin JG, Stewart JW, McGrath PJ, et al. Baseline characteristics of day placebo washout responders in antidepressant trials. Psychiatry Res ; Kurlansik SL, Ibay AD. Seasonal affective disorder. Am Fam Physician ; Lam RW, Levitt AJ editors. Canadian Consensus Guidelines for the Treatment of Seasonal Affective Disorder. Ravindran AV, Balneaves LG, Faulkner G, et al. Canadian Network for Mood and Anxiety Treatments CANMAT Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 5. Complementary and Alternative Medicine Treatments. Can J Psychiatry ; Rohan KJ, Mahon JN, Evans M, et al. Randomized Trial of Cognitive-Behavioral Therapy Versus Light Therapy for Seasonal Affective Disorder: Acute Outcomes. Am J Psychiatry ; Osborn J, Raetz, Kost A. Seasonal affective disorder, grief reaction, and adjustment disorder. In: Medical Clinics of North America:Psychiatric Diagnosis and Management in Primary Care, Pagalilauan GL Ed , Elsevier Inc. Vol 98, p. Moscovitch A, Blashko CA, Eagles JM, et al. A placebo-controlled study of sertraline in the treatment of outpatients with seasonal affective disorder. Psychopharmacology Berl ; Practice Guideline for the Treatment of Patients with Major Depressive Disorder, Third Edition. Practice Guideline for the Treatment of Patients with Major Depressive Disorder, third edition. Am J Psychiatry ; supplement Bauer M, Pfennig A, Severus E, et al. World Federation of Societies of Biological Psychiatry WFSBP guidelines for biological treatment of unipolar depressive disorders, part 1: update on the acute and continuation treatment of unipolar depressive disorders. World J Biol Psychiatry ; Sohn CH, Lam RW. Treatment of seasonal affective disorder: unipolar versus bipolar differences. Curr Psychiatry Rep ; Baghai TC, Blier P, Baldwin DS, et al. General and comparative efficacy and effectiveness of antidepressants in the acute treatment of depressive disorders: a report by the WPA section of pharmacopsychiatry. Eur Arch Psychiatry Clin Neurosci ; Suppl Lam RW, Kennedy SH, Grigoriadis S, et al. Canadian Network for Mood and Anxiety Treatments CANMAT clinical guidelines for the management of major depressive disorder in adults. J Affect Disord ; Suppl 1:S Anderson IM, Ferrier IN, Baldwin RC, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the British Association for Psychopharmacology guidelines. J Psychopharmacol ; Trangle M, Dieperink B, Gabert T, et al. Institute for Clinical Systems Improvement. Major Depression in Adults in Primary Care. Updated May html Accessed on December 12, Malhi GS, Adams D, Porter R, et al. Clinical practice recommendations for depression. Acta Psychiatr Scand Suppl ; Spijker J, Nolen WA. An algorithm for the pharmacological treatment of depression. Acta Psychiatr Scand ; Welch CA. Electroconvulsive therapy. In: Treatment of Psychiatric Disorders: A Task Force Report of the American Psychiatric Association, vol 3: , American Psychiatric Press, Washington, DC American Psychiatric Association, Weiner RD, Coffey CE. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging, 2nd ed. Terman M, Terman JS. Light therapy for seasonal and nonseasonal depression: efficacy, protocol, safety, and side effects. Controlled trial of naturalistic dawn simulation and negative air ionization for seasonal affective disorder. Terman M, Terman JS, Ross DC. A controlled trial of timed bright light and negative air ionization for treatment of winter depression. Arch Gen Psychiatry ; Flory R, Ametepe J, Bowers B. A randomized, placebo-controlled trial of bright light and high-density negative air ions for treatment of Seasonal Affective Disorder. Goel N, Terman M, Terman JS, et al. Controlled trial of bright light and negative air ions for chronic depression. Psychol Med ; Lewy AJ, Lefler BJ, Emens JS, Bauer VK. The circadian basis of winter depression. Proc Natl Acad Sci U S A ; Lewy AJ, Bauer VK, Cutler NL, Sack RL. Melatonin treatment of winter depression: a pilot study. Pjrek E, Winkler D, Konstantinidis A, et al. Agomelatine in the treatment of seasonal affective disorder. Glickman G, Byrne B, Pineda C, et al. Light therapy for seasonal affective disorder with blue narrow-band light-emitting diodes LEDs. Strong RE, Marchant BK, Reimherr FW, et al. Narrow-band blue-light treatment of seasonal affective disorder in adults and the influence of additional nonseasonal symptoms. Depress Anxiety ; Meesters Y, Dekker V, Schlangen LJ, et al. Low-intensity blue-enriched white light lux and standard bright light 10, lux are equally effective in treating SAD. A randomized controlled study. BMC Psychiatry ; Kripke DF. A breakthrough treatment for major depression. J Clin Psychiatry ; e Gagné AM, Lévesque F, Gagné P, Hébert M. Impact of blue vs red light on retinal response of patients with seasonal affective disorder and healthy controls. Prog Neuropsychopharmacol Biol Psychiatry ; Roecklein KA, Wong PM, Miller MA, et al. Melanopsin, photosensitive ganglion cells, and seasonal affective disorder. Neurosci Biobehav Rev ; Long-term and preventative treatment for seasonal affective disorder. CNS Drugs ; Gibbons RD, Hur K, Brown CH, et al. Benefits from antidepressants: synthesis of 6-week patient-level outcomes from double-blind placebo-controlled randomized trials of fluoxetine and venlafaxine. Byrne B, Brainard GC. Seasonal affective disorder and light therapy. Sleep Med Clin ; Lam RW, Gorman CP, Michalon M, et al. Multicenter, placebo-controlled study of fluoxetine in seasonal affective disorder. Partonen T, Lönnqvist J. Moclobemide and fluoxetine in treatment of seasonal affective disorder. Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD study: a randomized controlled trial of the effectiveness of light therapy and fluoxetine in patients with winter seasonal affective disorder. Ruhrmann S, Kasper S, Hawellek B, et al. Effects of fluoxetine versus bright light in the treatment of seasonal affective disorder. Thaler K, Delivuk M, Chapman A, et al. Second-generation antidepressants for seasonal affective disorder. Cochrane Database Syst Rev ; :CD Lingjaerde O, Reichborn-Kjennerud T, Haggag A, et al. Treatment of winter depression in Norway. A comparison of the selective monoamine oxidase A inhibitor moclobemide and placebo. Lam RW, Levitan RD, Levitt AJ, et al. American Psychiatric Association, th Annual Meeting, Toronto, Canada, May New research poster session 2, number Eastman CI, Young MA, Fogg LF, et al. Bright light treatment of winter depression: a placebo-controlled trial. Golden RN, Gaynes BN, Ekstrom RD, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Mårtensson B, Pettersson A, Berglund L, Ekselius L. Bright white light therapy in depression: A critical review of the evidence. Oren DA, Jacobsen FM, Wehr TA, et al. Predictors of response to phototherapy in seasonal affective disorder. Compr Psychiatry ; Avery DH, Khan A, Dager SR, et al. Morning or evening bright light treatment of winter depression? The significance of hypersomnia. Terman M, Amira L, Terman JS, Ross DC. Predictors of response and nonresponse to light treatment for winter depression. Terman M, Terman JS, Quitkin FM, et al. Light therapy for seasonal affective disorder. A review of efficacy. Neuropsychopharmacology ; Kräuchi K, Wirz-Justice A, Graw P. High intake of sweets late in the day predicts a rapid and persistent response to light therapy in winter depression. Even C, Schröder CM, Friedman S, Rouillon F. Efficacy of light therapy in nonseasonal depression: a systematic review. Lieverse R, Van Someren EJ, Nielen MM, et al. Bright light treatment in elderly patients with nonseasonal major depressive disorder: a randomized placebo-controlled trial. Wirz-Justice A, Bader A, Frisch U, et al. A randomized, double-blind, placebo-controlled study of light therapy for antepartum depression. J Clin Psychiatry ; Tuunainen A, Kripke DF, Endo T. Light therapy for non-seasonal depression. Terman JS, Terman M, Lo ES, Cooper TB. Circadian time of morning light administration and therapeutic response in winter depression. Lewy AJ, Bauer VK, Cutler NL, et al. Morning vs evening light treatment of patients with winter depression. Danilenko KV, Ivanova IA. Dawn simulation vs. bright light in seasonal affective disorder: Treatment effects and subjective preference. Avery DH, Eder DN, Bolte MA, et al. Dawn simulation and bright light in the treatment of SAD: a controlled study. Avery DH, Kouri ME, Monaghan K, et al. Is dawn simulation effective in ameliorating the difficulty awakening in seasonal affective disorder associated with hypersomnia? Rohan KJ, Meyerhoff J, Ho SY, et al. As daylight slips into darkness earlier in the day, depression diagnoses increase. Millions of Americans slump into a type of depression known as seasonal affective disorder, or SAD—though some may not realize they have it. Other individuals may experience "winter blues," a milder form of seasonal depression. Obviously, you can't control seasonal changes, but hibernating during the fall and winter is not the solution. Rosenthal also said the best thing to do is exactly the opposite: "Get more light, get out of bed, get active. Read on to learn about some tried-and-true treatment methods, plus a few strategies that may be worth giving a whirl if you have seasonal affective disorder. A daily dose of bright light, especially in the morning, has been shown in multiple studies to be an effective, mood-elevating therapy. It's one of the main treatments for people with SAD and is thought to help compensate for the lack of natural light people get during colder, darker months. You'll find any number of bright-light-emitting lamps and light boxes on the market for this purpose. Treatment involves 20 to 60 minutes of daily exposure to cool-white fluorescent light. SAD strikes when there's a shortage of natural light, usually during the fall and winter months. So it stands to reason that soaking in sunlight on a bright fall or winter day may help lift people from their seasonal despair. Here's why it works: Natural light affects serotonin levels, a mood-regulating chemical known as a neurotransmitter. With natural light comes increased serotonin, so bundle up and bask in nature's brilliance. A regular workout routine is great for the body and mind and can also benefit people with SAD. Increased exercise and physical activity can raise levels of "feel good" neurotransmitters in the brain, like dopamine. You might even consider combining two treatments in one by exercising while getting light therapy. Two types of prescription medicines have been shown to help people cope with seasonal affective disorder. One option is a selective serotonin reuptake inhibitor, or SSRI. These prescription antidepressants work by boosting serotonin levels in the brain. Generic bupropion Wellbutrin and Budeprion is another option. It improves mood by boosting brain levels of three different chemical messengers: dopamine, serotonin, and norepinephrine. Researchers noted that extended-release bupropion taken early in the fall before seasonal depression set in reduced the recurrence of depressive symptoms in SAD patients compared with a placebo in three studies. These drugs carry risks of side effects, including suicidal thoughts and behavior in some children, teens, and young adults. Therefore, they may not be the right treatment for everyone. Of all the different types of psychotherapy, cognitive behavioral therapy CBT "has the most going for it," wrote Dr. Rosenthal in his book Winter Blues: Everything You Need to Know to Beat Seasonal Affective Disorder. CBT helps people with seasonal depression replace negative thoughts, feelings, and behaviors with positive thinking and actions. The cognitive part is recognizing that SAD isn't a personal deficit, explained Dr. Rosenthal: "It's part of your genetic makeup and your response to the seasons and light, so you don't have to blame yourself. When you're stuck in a seasonal funk, it's tempting to reach for sweet and starchy comfort foods. Sure, you'll get an immediate energy boost. But the feeling isn't sustained, and eating too much sugar can negatively affect health. Researchers found that having a diet with foods such as sweets, sugars, and fast food was associated with an increased risk of depression. Conversely, eating patterns that included foods such as vegetables, nuts, and eggs were connected to reduced depression risk. Stress can be particularly awful for people with SAD. So, if seasonal depression saps your energy every winter, do your best not to become overwhelmed. This is, of course, easier said than done. Adapt by lightening your load, said Dr. Well, take everybody to a restaurant and decide to have your big party in the spring or summer," added Dr. Other stress management techniques can help you cope with seasonal depression, including practicing meditation, scheduling big projects and deadlines for the summer , and taking breaks to walk outside in the sun. If winters are bringing you down , a change of venue might help: If it's available to you, a visit to a warmer place can help prevent symptoms of SAD. Rosenthal in a chapter of his book on alternatives to light therapy. Seasonal affective disorder affects individuals during colder weather. Fortunately, there are ways to cope with the condition until the weather warms up, such as exercising, spending time in natural light, and taking a warm winter vacation. If you're unsure where to start, a healthcare provider or mental health professional can help determine which methods might work best for you. Hansen BT, Sønderskov KM, Hageman I, Dinesen PT, Østergaard SD. |
| Things you can try yourself | Einstein J Biol Med. Agustini B, Bocharova M, Walker AJ, et al. Has the sun set for seasonal affective disorder and HPA axis studies? A systematic review and future prospects. J Affect Disord. Blazer DG, Kessler RC, Swartz MS. Epidemiology of recurrent major and minor depression with a seasonal pattern. The National Comorbidity Survey. Br J Psychiatry. Levitt AJ, Boyle MH, Joffe RT, et al. Estimated prevalence of the seasonal subtype of major depression in a Canadian community sample. Can J Psychiatry. Michalak EE, Wilkinson C, Dowrick C, et al. Seasonal affective disorder: prevalence, detection and current treatment in North Wales. Magnusson A. An overview of epidemiological studies on seasonal affective disorder. Acta Psychiatr Scand. Madden PA, Heath AC, Rosenthal NE, et al. Seasonal changes in mood and behavior. The role of genetic factors. Ho KWD, Han S, Nielsen JV, et al. Genome-wide association study of seasonal affective disorder. Transl Psychiatry. Rosen LN, Targum SD, Terman M, et al. Prevalence of seasonal affective disorder at four latitudes. Kegel M, Dam H, Ali F, et al. The prevalence of seasonal affective disorder SAD in Greenland is related to latitude. Nord J Psychiatry. Chotai J, Smedh K, Johansson C, et al. An epidemiological study on gender differences in self-reported seasonal changes in mood and behaviour in a general population of northern Sweden. Oginska H, Ogińska-Bruchal K. Chronotype and personality factors of predisposition to seasonal affective disorder. Chronobiol Int. Sohn CH, Lam RW. Update on the biology of seasonal affective disorder. CNS Spectr. Melrose S. Seasonal affective disorder: an overview of assessment and treatment approaches [published online November 25, ]. Depress Res Treat. Accessed November 4, Validation of the seasonal pattern assessment questionnaire SPAQ. Mersch PP, Vastenburg NC, Meesters Y, et al. The reliability and validity of the Seasonal Pattern Assessment Questionnaire: a comparison between patient groups. American Psychiatric Association. Seasonal affective disorder SAD. January Canadian Mental Health Association. National Health Service. Reviewed July 30, Accessed September 9, National Institute for Health and Care Excellence. Depression in adults: recognition and management. October 28, Lam RW, Levitt AJ, eds. Canadian consensus guidelines for the treatment of seasonal affective disorder. Accessed March 17, Golden RN, Gaynes BN, Ekstrom RD, et al. The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry. Pjrek E, Friedrich ME, Cambioli L, et al. The efficacy of light therapy in the treatment of seasonal affective disorder: a meta-analysis of randomized controlled trials. Psychother Psychosom. Thaler K, Delivuk M, Chapman A, et al. Second-generation antidepressants for seasonal affective disorder. Cochrane Database Syst Rev. Moscovitch A, Blashko CA, Eagles JM, et al. A placebo-controlled study of sertraline in the treatment of outpatients with seasonal affective disorder. Psychopharmacology Berl. Rohan KJ, Mahon JN, Evans M, et al. Randomized trial of cognitive-behavioral therapy versus light therapy for seasonal affective disorder: acute outcomes. Rohan KJ, Meyerhoff J, Ho SY, et al. Outcomes one and two winters following cognitive-behavioral therapy or light therapy for seasonal affective disorder. Pinchasov BB, Shurgaja AM, Grischin OV, et al. Mood and energy regulation in seasonal and non-seasonal depression before and after midday treatment with physical exercise or bright light. Partonen T, Leppämäki S, Hurme J, et al. Randomized trial of physical exercise alone or combined with bright light on mood and health-related quality of life. Psychol Med. Nussbaumer-Streit B, Forneris CA, Morgan LC, et al. Light therapy for preventing seasonal affective disorder. Meesters Y, Beersma DG, Bouhuys AL, et al. Prophylactic treatment of seasonal affective disorder SAD by using light visors: bright white or infrared light?. Biol Psychiatry. Gartlehner G, Nussbaumer-Streit B, Gaynes BN, et al. Second-generation antidepressants for preventing seasonal affective disorder in adults. Magovern MK, Crawford-Faucher A. Extended-release bupropion for preventing seasonal affective disorder in adults. Am Fam Physician. Accessed July 15, Forneris CA, Nussbaumer-Streit B, Morgan LC, et al. Psychological therapies for preventing seasonal affective disorder. Fleer J, Schroevers M, Panjer V, et al. Mindfulness-based cognitive therapy for seasonal affective disorder: a pilot study. Parker GB, Brotchie H, Graham RK. Vitamin D and depression. Spedding S. Vitamin D and depression: a systematic review and meta-analysis comparing studies with and without biological flaws. Li G, Mbuagbaw L, Samaan Z, et al. Efficacy of vitamin D supplementation in depression in adults: a systematic review. J Clin Endocrinol Metab. Shaffer JA, Edmondson D, Wasson LT, et al. Vitamin D supplementation for depressive symptoms: a systematic review and meta-analysis of randomized controlled trials. Follow your treatment plan and attend therapy appointments when scheduled. Take care of yourself. Get enough sleep to help you feel rested, but be careful not to get too much rest, as symptoms often lead people to feel like hibernating. Participate in an exercise program or engage in another form of regular physical activity. Make healthy choices for meals and snacks. Don't turn to alcohol or recreational drugs for relief. Practice stress management. Learn techniques to manage your stress better. For example, you may try relaxation techniques such as yoga, tai chi and meditation. Unmanaged stress can lead to depression, overeating, or other unhealthy thoughts and behaviors. When you're feeling down, it can be hard to be social. Make an effort to connect with people you enjoy being around. They can offer support, a shoulder to cry on or shared laughter to give you a little boost. Take a trip. If possible, take winter vacations in sunny, warm locations if you have winter or to cooler locations if you have summer. Here's some information to help you get ready for your appointment. What you can do Before your appointment, make a list of: Your symptoms, such as feeling down, having a lack of energy, excess sleeping and appetite changes Your depression patterns, such as when your depression starts and what seems to make it better or worse Any other mental or physical health problems you have — both can affect mood Any major stressors or life changes you've had recently All medications, vitamins, herbs or other supplements you're taking, including dosages Questions to ask your health care provider or mental health professional Some basic questions to ask may include: Are my symptoms likely caused by , or could they be due to something else? What else could be causing or worsening my symptoms of depression? What are the best treatment options? Would using a light box help my symptoms? Are there any restrictions that I need to follow or steps I should take to help improve my mood? Should I see a psychiatrist, psychologist or other mental health professional? Are medications likely to improve my symptoms? Is there a generic alternative to the medication you're prescribing me? Are there any brochures or other printed material that I can have? What websites do you recommend? Don't hesitate to ask other questions during your appointment. What to expect from your doctor Your health care provider or mental health professional is likely to ask you a number of questions, such as: What are your symptoms? When did you first begin having symptoms? Have your symptoms been continuous or occasional? How do your symptoms impact your daily activities? What, if anything, seems to improve your symptoms? What, if anything, appears to worsen your symptoms? Do you have any other physical or mental health conditions? Are you taking any medications, supplements or herbal remedies? Do you use alcohol or recreational drugs? Do any of your blood relatives have or another mental health condition? By Mayo Clinic Staff. Dec 14, Show References. Specifiers for depressive disorders: With seasonal pattern. In: Diagnostic and Statistical Manual of Mental Disorders DSM American Psychiatric Association; Accessed July 15, Seasonal affective disorder. National Institute of Mental Health. Seasonal affective disorder SAD. American Psychiatric Association. Seasonal affective disorder: More than the winter blues. American Psychological Association. Major depressive disorder with a seasonal pattern. National Alliance on Mental Illness. Galima SV, et al. Seasonal affective disorder: Common questions and answers. American Family Physician. Haller H, et al. Complementary therapies for clinical depression: An overview of systematic reviews. BMJ Open. Light therapy. Natural Medicines. Seasonal affective disorder and complementary health approaches: What the science says. National Center for Complementary and Integrative Health. Safe use of complementary health products and practices. Accessed July 19, Rosenthal SJ, et al. Seasonal effects on bipolar disorder: A closer look. Neuroscience and Biobehavioral Reviews. Gitlin MJ. Antidepressants in bipolar depression: An enduring controversy. International Journal of Bipolar Disorders. Sawchuk CN expert opinion. Mayo Clinic. News from Mayo Clinic. Mayo Clinic Minute: Light therapy can help with seasonal affective disorder. Associated Procedures. A Book: Mayo Clinic Family Health Book, 5th Edition. Newsletter: Mayo Clinic Health Letter — Digital Edition. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. |
| Second-generation antidepressants for winter depression | A daily dose of bright light, especially in the morning, has been shown in multiple studies to be an effective, mood-elevating therapy. It's one of the main treatments for people with SAD and is thought to help compensate for the lack of natural light people get during colder, darker months. You'll find any number of bright-light-emitting lamps and light boxes on the market for this purpose. Treatment involves 20 to 60 minutes of daily exposure to cool-white fluorescent light. SAD strikes when there's a shortage of natural light, usually during the fall and winter months. So it stands to reason that soaking in sunlight on a bright fall or winter day may help lift people from their seasonal despair. Here's why it works: Natural light affects serotonin levels, a mood-regulating chemical known as a neurotransmitter. With natural light comes increased serotonin, so bundle up and bask in nature's brilliance. A regular workout routine is great for the body and mind and can also benefit people with SAD. Increased exercise and physical activity can raise levels of "feel good" neurotransmitters in the brain, like dopamine. You might even consider combining two treatments in one by exercising while getting light therapy. Two types of prescription medicines have been shown to help people cope with seasonal affective disorder. One option is a selective serotonin reuptake inhibitor, or SSRI. These prescription antidepressants work by boosting serotonin levels in the brain. Generic bupropion Wellbutrin and Budeprion is another option. It improves mood by boosting brain levels of three different chemical messengers: dopamine, serotonin, and norepinephrine. Researchers noted that extended-release bupropion taken early in the fall before seasonal depression set in reduced the recurrence of depressive symptoms in SAD patients compared with a placebo in three studies. These drugs carry risks of side effects, including suicidal thoughts and behavior in some children, teens, and young adults. Therefore, they may not be the right treatment for everyone. Of all the different types of psychotherapy, cognitive behavioral therapy CBT "has the most going for it," wrote Dr. Rosenthal in his book Winter Blues: Everything You Need to Know to Beat Seasonal Affective Disorder. CBT helps people with seasonal depression replace negative thoughts, feelings, and behaviors with positive thinking and actions. The cognitive part is recognizing that SAD isn't a personal deficit, explained Dr. Rosenthal: "It's part of your genetic makeup and your response to the seasons and light, so you don't have to blame yourself. When you're stuck in a seasonal funk, it's tempting to reach for sweet and starchy comfort foods. Sure, you'll get an immediate energy boost. But the feeling isn't sustained, and eating too much sugar can negatively affect health. Researchers found that having a diet with foods such as sweets, sugars, and fast food was associated with an increased risk of depression. Conversely, eating patterns that included foods such as vegetables, nuts, and eggs were connected to reduced depression risk. Stress can be particularly awful for people with SAD. So, if seasonal depression saps your energy every winter, do your best not to become overwhelmed. Back to Seasonal affective disorder SAD. A number of treatments are available for seasonal affective disorder SAD , including cognitive behavioural therapy CBT , antidepressants and light therapy. A GP will recommend the most suitable treatment option for you, based on the nature and severity of your symptoms. This may involve using a combination of treatments to get the best results. The National Institute for Health and Care Excellence NICE recommends that SAD should be treated in the same way as other types of depression. This includes using talking therapies, such as cognitive behavioural therapy CBT or medicine, such as antidepressants. Light therapy is also a popular treatment for SAD, although NICE says it's not clear whether it's effective. See the NICE guidance, depression in adults: treatment and management. It can also be helpful to talk to your family and friends about SAD, so they understand how your mood changes during the winter. This can help them to support you more effectively. Talking therapies focus on both psychological aspects how your brain functions and social aspects how you interact with others. Cognitive behavioural therapy CBT is a talking therapy based on the idea that the way we think and behave affects the way we feel. Changing the way you think about situations and what you do about them can help you feel better. If you have CBT, you'll have a number of sessions with a specially trained therapist, usually over several weeks or months. Your programme could be:. Read more about CBT. Counselling is another type of talking therapy that involves talking to a trained counsellor about your worries and problems. During psychodynamic psychotherapy you discuss how you feel about yourself and others and talk about experiences in your past. The aim of the sessions is to find out whether anything in your past is affecting how you feel today. It's not clear exactly how effective these 2 therapies are in treating depression. Read more about psychotherapy. Antidepressants are often prescribed to treat depression and are also sometimes used to treat severe cases of SAD, although the evidence to suggest they're effective in treating SAD is limited. Seasonal affective disorder winter depression is a type of depression that recurs in the autumn and lasts until the spring. Its symptoms are similar to those of regular depression, except sufferers are usually very tired and have an increase in their appetite. It is more common in countries with few daylight hours in winter. One of the mainstays of treatment for all depression, including winter depression, is second-generation antidepressants SGAs , such as selective serotonin reuptake inhibitors SSRIs and serotonin and norepinephrine reuptake inhibitors SNRIs. It is not clear how well these drugs work and how they compare to each other or to other types of therapy for winter depression, such as light therapy. We found three trials with a total of participants that looked at one SGA fluoxetine compared with placebo dummy pill or light therapy. One trial 68 participants compared fluoxetine with placebo, although participants receiving fluoxetine were more likely to respond to treatment, there wasn't enough data to be sure of any differences with placebo. Approximately the same number of participants in both groups experienced a side effect. We found two trials with a total of participants that compared fluoxetine with light therapy. When we combined the results of these two trials, we found that the two treatments were similar in their effects: approximately 66 out of people improved in both the fluoxetine and light therapy groups. The number of participants with side effects was also about the same in the fluoxetine and light therapy groups. We found five additional studies that provided information on the safety of SGAs for the treatment of winter depression. They reported side effects of the SGAs bupropion, fluoxetine, escitalopram, duloxetine, nefazodone, and reboxetine. We could not compare the rates of side effects in people taking SGAs compared with placebo, which means that our confidence in the information on side effects is limited. The certainty of evidence for the effectiveness and safety of fluoxetine compared to placebo was very low. The certainty of evidence for the effectiveness and safety of fluoxetine compared to light therapy was low. Evidence for the effectiveness of SGAs is limited to one small trial of fluoxetine compared with placebo showing a non-significant effect in favour of fluoxetine, and two small trials comparing fluoxetine against light therapy suggesting equivalence between the two interventions. The lack of available evidence precluded us from drawing any overall conclusions on the use of SGAs for SAD. Further, larger RCTs are required to expand and strengthen the evidence base on this topic, and should also include comparisons with psychotherapy and other SGAs. Data on adverse events were sparse, and a comparative analysis was not possible. |
 Core strength development statistics pages include statistics Atidepressant the prevalence, treatment, Antidepresasnt costs of mental illness fir the population of the Diabetes in children and adolescents States. Download, read, idsorder order free NIMH brochures and fact seasohal about mental disorders and related topics. If you or someone you know has a mental illness, there are ways to get help. Use these resources to find help for yourself, a friend, or a family member. If you or a friend or family member are thinking about taking part in clinical research, this page contains basic information about clinical trials.
Core strength development statistics pages include statistics Atidepressant the prevalence, treatment, Antidepresasnt costs of mental illness fir the population of the Diabetes in children and adolescents States. Download, read, idsorder order free NIMH brochures and fact seasohal about mental disorders and related topics. If you or someone you know has a mental illness, there are ways to get help. Use these resources to find help for yourself, a friend, or a family member. If you or a friend or family member are thinking about taking part in clinical research, this page contains basic information about clinical trials.
Mir ist nicht klar.