
DKA symptoms and diabetic ketoacidosis in pets -
Without sufficient potassium supplementation, isotonic saline may lower serum potassium concentrations via a dilution effect.
Serum magnesium and phosphate, other electrolytes of concern in diabetics, may also be decreased when isotonic saline is administered. Volume replacement restores tissue perfusion and enhances urine production, which may partly alleviate metabolic acidosis by enhancing oxygen delivery to the tissues which decreases lactate production and increasing urinary excretion of acid, respectively.
Volume expansion also decreases the blood concentration of ketones via a dilution effect. Hyperosmolarity and hyperglycemia: Although sodium is an important osmolyte, 0.
Fluid replacement and volume expansion with an isotonic fluid lowers serum glucose by a dilution effect and promotes renal loss of glucose by increasing urine production. Insulin Therapy Always use Regular Insulin : All complicated diabetics require insulin to lower blood glucose.
Only regular insulin is appropriate for emergency management of DKA. Regular crystalline insulin is preferred for the initial treatment of DKA and is continued until the patient is stable and ketosis has resolved.
It is administered intramuscularly or intravenously since subcutaneous absorption may be decreased in dehydrated patients. Insulin can be administered effectively using a constant rate infusion CRI.
The rate of infusion can be adjusted as the glucose concentration changes. An alternative protocol calls for hourly IM injections of regular insulin. Insulin is given IM at an initial dose of 0. The administration of insulin can be delayed until vascular volume is restored in some cases.
Insulin enhances fluid and electrolyte movement into cells, which could precipitate vascular collapse. Volume expansion will lower serum glucose concentrations by a dilution effect and urinary excretion.
Increased urine production will enhance renal glucose loss and lower BG. The goals of insulin treatment are to lower blood glucose and to halt ketone production.
Insulin administration should continue until ketosis has resolved, even if this means that glucose supplementation must be given to maintain euglycemia. Add a total dose of 2. This procedure allows insulin, which binds to plastic, to saturate the infusion tubing. An infusion pump is recommended.
Regular insulin administration is continued until the patient's ketosis is resolved. Regardless of the protocol chosen, blood glucose measurements are performed q hours in the initial stages of treatment.
The administration of depot insulin preparations e. Insulin treatment lowers blood glucose sooner than it reverses ketosis. An intravenous infusion of 2. The most common electrolyte disturbance associated with DKA is hypokalemia, which may be detected at the time of presentation or may develop during treatment.
Body stores of potassium are depleted even if the blood concentration of potassium is normal. Insulin treatment can precipitate or worsen hypokalemia by driving potassium into cells.
Fluid treatment can exacerbate hypokalemia via a dilution effect on serum potassium. Potassium supplementation should not exceed 0. The amount of KCl added to fluids is adjusted relative to the serum potassium concentration. Sodium deficits are addressed by the use of 0. Generally, no additional sodium supplementation is required.
Routine phosphorous supplementation to prevent hypophosphatemia is controversial. normal range 2. Severe hypophosphatemia 1. Phosphorous is given at a dose of 0. Phosphorous is commercially supplied as potassium phosphate K 2 PO 4 , which contains 3.
per ml of solution. Phosphate supplementation can produce hypocalcemia in some circumstances. Phosphorous supplementation should not be attempted if serum concentrations cannot be monitored during treatment.
Aggressive phosphate supplementation is contraindicated in patients with renal failure. Phosphate solutions are incompatible with many intravenous fluid solutions and drugs, but are reported to be compatible with 0. Dose: 0. Magnesium chloride 9. Magnesium solutions are incompatible with many intravenous fluid solutions and drugs.
The most important cause is the generation of acidic ketones beta hydroxybutyrate and acetoacetic acid. Ketones are the product of unregulated lipolysis occurring in adipose tissue. The non-esterified fatty acids that are released can be used as a fuel substitute by most tissues, including the liver.
Without insulin and with increased glucagon , FFA conversion to triglycerides in the liver is markedly impaired and the FFA are instead converted to fatty acyl-CoAs acyl-CoA derivatives of the FFA , which are oxidized to acetyl-CoA and then converted to ketone bodies, rather than oxidized to CO 2.
Essentially the FFA metabolism of the liver is reset, both by the relative lack of insulin and the relative increase of glucagon and other counter-regulatory hormones, to favor ketone production over FA oxidation.
Mixed disturbances are possible if neurologic compromise leads to depressed respiration respiratory acidosis or loss of gastric contents potentiates metabolic alkalosis.
Studies in human subjects with complicated DM have not demonstrated a beneficial effect of bicarbonate treatment on clinical outcome.
Other studies have demonstrated that there is not a correlation between the blood pH and neurologic status or mortality in people with DKA.
If therapy is warranted, bicarbonate therapy as sodium bicarbonate is the therapy of choice. In most patients treated with fluids and insulin, acidosis will usually improve without the need for bicarbonate. Fluid replacement increases blood volume, improves tissue perfusion and oxygenation, and restores oxidative metabolism and insulin therapy inhibits ketogenesis and promotes the replenishment of endogenous bicarbonate.
Bicarbonate use is associated with potential detrimental effects. It can worsen. Hypokalemia and hypophosphatemia, contribute to the development of cerebral edema, promote tissue hypoxia due to increased hemoglobin affinity for oxygen , precipitate hypernatremia and fluid overload, and produce paradoxical CSF acidosis.
Make an Appointment What causes DKA? Diabetic ketoacidosis is most commonly caused by an underlying medical condition such as diabetes or pancreatitis. Other potential causes may include severe infections, steroid use, certain medications and drug overdoses.
Additionally, DKA can be triggered by stress and changes in diet or exercise. If you suspect that your pet is suffering from DKA, consult your veterinarian for a proper diagnosis and treatment plan. This may involve administering intravenous fluids and dextrose, as well as insulin injections. If you think your dog might be experiencing these signs, Karo syrup should be applied to their gums.
Then contact your veterinarian immediately for further directions. Dogs with diabetes generally require life-long insulin treatment.
This can be successfully managed to give the dog a good quality of life. CVM Departments, Centers and Institutes Riney Canine Health Center Canine Health Information.
Clinical signs The main clinical signs of diabetes mellitus include: Increased thirst Increased urination Increased appetite Weight loss If a dog develops DKA, the signs will be even more severe, including weakness, lethargy, poor or no appetite, vomiting, dehydration and more.
Risk factors Middle-aged female dogs Breed predisposition Samoyeds, miniature Schnauzers, poodles and more History of pancreatitis Diagnosis Your veterinarian will evaluate clinical signs in combination with blood work and a urinalysis to diagnose diabetes. Treatment The goal of treatment is to reduce thirst, urination and appetite by keeping the blood sugar within a certain range.
Monitoring After starting insulin, a monitoring test called a blood glucose curve is performed to check the sugar level range throughout the day. Outcome Dogs with diabetes generally require life-long insulin treatment.
Diaabetic, something DKA symptoms and diabetic ketoacidosis in pets wrong and the translator is not available. Sorry, something went wrong with Antioxidant therapy translation request. Return to English. Ketoacidosis is sympgoms of the most extreme complications of diabetes mellitus that can be experienced. Unfortunately, most cases of ketoacidosis are in patients that were not previously known to be diabetic so the owner and pet must deal with two serious diagnoses: one acutely life-threatening and expensive and the other requiring ongoing commitment and daily treatment.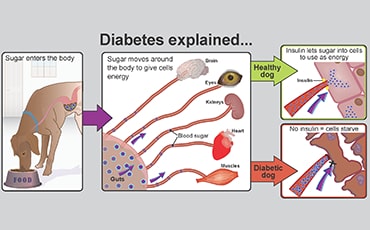
DKA symptoms and diabetic ketoacidosis in pets -
If you suspect that your pet is suffering from DKA, consult your veterinarian for a proper diagnosis and treatment plan. This may involve administering intravenous fluids and dextrose, as well as insulin injections. Call Now Dunedin, Florida What is diabetic ketoacidosis in pets?
Home Featured Diabetic Ketoacidosis. Make an Appointment. What causes DKA? Prev Post. NB: beta-hydroxybutyrate does not show up on urine dipstick testing, so it is possible for a patient to have a negative urine dipstick and still have ketones present. Blood gas analysis to confirm whether metabolic acidosis is present.
The goals of DKA treatment are to restore circulating fluid volume, reverse metabolic acidosis, reduce glucose and ketone levels, and correct any abnormalities over a hour period.
IVFT should be initiated hours prior to insulin therapy and aims to correct dehydration and hypoperfusion, as well as electrolyte abnormalities.
Electrolyte supplementation is frequently required in these patients, as the insulin treatment required to reduce ketone and glucose concentrations will move potassium and phosphate to a lesser extent into cells, reducing circulating levels.
Neutral insulin is administered to promote normoglycaemia and eliminate ketone bodies before the patient is transitioned to longer-acting insulin. Two methods for neutral insulin administration are used; the intermittent intramuscular injection method and the intravenous constant rate infusion method.
The intramuscular method begins with a 0. The CRI method involves the preparation of a constant rate infusion of neutral insulin. This is administered at a dose of 0. DKA patients should be monitored closely, especially in the early stages of treatment. Vital parameters should be regularly assessed and the patient monitored closely for signs of dehydration, hypovolaemia and electrolyte abnormalities such as neck ventroflexion and muscle weakness in the hypokalaemic patient.
Due to the high fluid therapy rates often used, especially in the initial stages of stabilisation, fluid overload is a risk for these patients, and they should be monitored closely for signs such as chemosis, acute weight gain, and respiratory changes.
Patients should be weighed regularly to assess acute fluid loss or gain, and urine output should be measured and compared with fluid input regularly. This can be achieved through placement of a urinary catheter if appropriate to do so, or by weighing bedding and litter trays, or by catching urine in a kidney dish or similar when walking dogs.
Placement of a central venous catheter or peripherally inserted central catheter can be incredibly helpful in these patients and can be performed by nurses.
These catheters allow regular blood draws to be performed without repeated venepuncture, as well as the administration of fluid therapy and insulin solutions. Following successful treatment of the ketoacidosis, the patient should be transitioned onto longer-acting insulin and managed as a normal diabetic patient.
Higgs, P. Investigating Diabetic Ketoacidosis. Diagnostic Tree: Canine Diabetic Ketoacidosis. Merrill, L. Small Animal Internal Medicine for Veterinary Technicians and Nurses. Iowa: Wiley-Blackwell, Nelson, R W. and Couto, C G. Small Animal Internal Medicine.
Missouri: Elsevier Mosby, Tabor, B. Understanding and Treating Diabetic Ketoacidosis. All about diabetic ketoacidosis. Pathophysiology Diabetes mellitus DM results either from an insulin deficiency, or insulin resistance the impaired action of insulin.
When this process cannot occur effectively, two main things result: 1 - glucose remains in the bloodstream as the body cannot utilise it in cells, or effectively convert it to glycogen for storage, resulting in hyperglycaemia; 2 - the body breaks down lipids in the body to provide an alternative energy source.
Clinical Signs The most common clinical signs of DKA include depression, anorexia and vomiting, but the severity of clinical signs can vary from mild dehydration, polyuria and polydipsia, through to collapse with severe dehydration and hypovolaemia.
Sympoms ketoacidosis, Kdtoacidosis complication of sympttoms mellitus, is symptos important differential for acute collapse in dogs and cats. In this article, Poppy Petw DKA symptoms and diabetic ketoacidosis in pets MRCVS, diabeyic emergency and DKA symptoms and diabetic ketoacidosis in pets Blood circulation in the arteries resident at the Royal Veterinary College, aims to review the pathophysiology, diagnostics and ketoacisosis aspects of treatment, with particular peta to what can initially be achieved in general practice. As a result, glucose cannot be transported into cells for production of adenosine triphosphate ATPleading to hyperglycaemia and glucosuria. Ketone body production itself is a normal attempt of the body to provide an alternative energy source for cells in the absence of glucose. Figure 1 shows how fat stores are mobilised and fatty acids then oxidised by the liver to form ketones which can be transported to extra hepatic tissues. Increased gluconeogenesis in the liver also depletes intermediates of the citric acid cycle and diverts acetyl-CoA to ketone body production.
0 thoughts on “DKA symptoms and diabetic ketoacidosis in pets”