Enhanced germ resistance -
When determining empiric treatment for a given patient, clinicians should also consider: 1 previous organisms identified from the patient and associated antibiotic susceptibility data in the last six months, 2 antibiotic exposures within the past 30 days, and 3 local susceptibility patterns for the most likely pathogens.
Empiric decisions should be refined based on the identity and susceptibility profile of the pathogen. Recommendations on durations of therapy are not provided, but clinicians are advised that the duration of therapy should not differ for infections caused by organisms with resistant phenotypes compared to infections caused by more susceptible phenotypes.
After antibiotic susceptibility results are available, it may become apparent that inactive antibiotic therapy was initiated empirically. This may impact the duration of therapy. For example, cystitis is typically a mild infection [4]. If an antibiotic not active against the causative organism was administered empirically for cystitis, but clinical improvement nonetheless occurred, it is generally not necessary to repeat a urine culture, change the antibiotic regimen, or extend the planned treatment course.
However, for all other infections, if antibiotic susceptibility data indicate a potentially inactive agent was initiated empirically, a change to an active regimen for a full treatment course dated from the start of active therapy is recommended.
Additionally, important host factors related to immune status, ability to attain source control, and general response to therapy should be considered when determining treatment durations for antimicrobial-resistant infections, as with the treatment of any bacterial infection.
Finally, whenever possible, oral step-down therapy should be considered, particularly if the following criteria are met: 1 susceptibility to an appropriate oral agent is demonstrated, 2 the patient is hemodynamically stable, 3 reasonable source control measures have occurred, and 4 concerns about insufficient intestinal absorption are not present [5].
ESBLs are enzymes that inactivate most penicillins, cephalosporins, and aztreonam. EBSL-E generally remain susceptible to carbapenems.
ESBLs do not inactivate non-β-lactam agents e. However, organisms carrying ESBL genes often harbor additional genes or mutations in genes that mediate resistance to a broad range of antibiotics.
Any gram-negative organism has the potential to harbor ESBL genes; however, they are most prevalent in Escherichia coli, Klebsiella pneumoniae, Klebsiella oxytoca, and Proteus mirabilis[]. CTX-M enzymes, particularly CTX-M, are the most common ESBLs in the United States[10]. ESBLs other than CTX-M with unique hydrolyzing abilities are also present, including variants of narrow-spectrum TEM and SHV β-lactamases with amino acid substitutions, but they have undergone less rigorous clinical investigation than CTX-M enzymes [].
Routine EBSL testing is not performed by most clinical microbiology laboratories [15, 16]. Rather, non-susceptibility to ceftriaxone i. For this guidance document, ESBL-E will refer to presumed or confirmed ESBL-producing E. coli , K. pneumoniae , K. oxytoca , or P. Treatment suggestions for ESBL-E infections assume that in vitro activity of preferred and alternative antibiotics has been demonstrated.
Suggested approach : Nitrofurantoin and TMP-SMX are preferred treatment options for uncomplicated cystitis caused by ESBL-E.
Ciprofloxacin, levofloxacin, and carbapenems are alternative agents for uncomplicated cystitis caused by ESBL-E. Although effective, their use is discouraged when nitrofurantoin or TMP-SMX are active. Single dose aminoglycosides and oral fosfomycin for E.
coli only are also alternative treatments for uncomplicated cystitis caused by ESBL-E. Nitrofurantoin and TMP-SMX have been shown to be safe and effective options for uncomplicated cystitis, including uncomplicated ESBL-E cystitis [4, 19, 20].
Although carbapenems and the fluoroquinolones ciprofloxacin or levofloxacin are effective agents against ESBL-E cystitis [21, 22] , their use for uncomplicated cystitis is discouraged when other safe and effective options are available.
Limiting use of these agents preserves their activity for future infections when treatment options may be more restricted. Moreover, limiting their use reduces the risk of associated toxicities, particularly with the fluoroquinolones, which have been associated with an increased risk for prolonged QTc intervals, tendinitis and tendon rupture, aortic dissections, seizures, peripheral neuropathy, and Clostridioides difficile infections [].
Treatment with a single intravenous IV dose of an aminoglycoside is an alternative treatment option for uncomplicated ESBL-E cystitis. Aminoglycosides are nearly exclusively eliminated by the renal route.
A single IV dose is generally effective for uncomplicated cystitis, with minimal toxicity, but robust clinical trial data are lacking [27]. Oral fosfomycin is an alternative treatment option exclusively for uncomplicated ESBL-E cystitis caused by E.
Fosfomycin is not suggested for the treatment of infections caused by K. pneumoniae and several other gram-negative organisms which frequently carry fosA hydrolase genes that may lead to clinical failure [28, 29]. A randomized open-label trial indicated that a single dose of oral fosfomycin is associated with higher clinical failure than a five-day course of nitrofurantoin for uncomplicated cystitis [19].
Although this trial was not limited to E. coli cystitis, in a subgroup analysis exclusively of E. The additive benefit of a second dose of oral fosfomycin for uncomplicated cystitis is not known.
The panel does not suggest prescribing amoxicillin-clavulanic acid or doxycycline for the treatment of ESBL-E cystitis. A randomized clinical trial compared a three-day regimen of amoxicillin-clavulanic acid to a three-day course of ciprofloxacin for women with uncomplicated E. coli cystitis [21].
The proportion of women in the trial infected with ESBL-E strains is not available. Even though data indicate that clavulanic acid may be effective against ESBLs in vitro [30, 31] , this may not translate to clinical efficacy [32].
Robust data indicating that oral amoxicillin-clavulanic acid is effective for uncomplicated ESBL-E UTI are lacking. Two clinical outcomes studies, published more than 40 years ago, demonstrated that oral tetracyclines may be effective for the treatment of UTIs [33, 34]. Both of these studies, however, primarily focused on P.
aeruginosa , an organism not susceptible to oral tetracyclines, questioning the impact that antibiotic therapy had on clinical cure. Doxycycline is primarily eliminated through the intestinal tract [35].
Its urinary excretion is limited. Until more convincing data demonstrating the clinical effectiveness of oral doxycycline for the treatment of ESBL-E cystitis are available, the panel suggests against use of doxycycline for this indication.
The roles of piperacillin-tazobactam, cefepime, and the cephamycins for the treatment of uncomplicated cystitis are discussed in Question 1. Suggested approach: TMP-SMX, ciprofloxacin, or levofloxacin are preferred treatment options for pyelonephritis and cUTIs caused by ESBL-E.
Ertapenem, meropenem, and imipenem-cilastatin are preferred agents when resistance or toxicities preclude the use of TMP-SMX or fluoroquinolones. Aminoglycosides for a full treatment course are an alternative option for the treatment of ESBL-E pyelonephritis or cUTI.
TMP-SMX, ciprofloxacin, and levofloxacin are preferred treatment options for patients with ESBL-E pyelonephritis and cUTIs based on the ability of these agents to achieve adequate and sustained concentrations in the urine, clinical trial results, and clinical experience [].
Carbapenems are also preferred agents, when resistance or toxicities prevent use of TMP-SMX or fluoroquinolones, or early in the treatment course if a patient is critically ill Question 1. If a carbapenem is initiated and susceptibility to TMP-SMX, ciprofloxacin, or levofloxacin is demonstrated, transitioning to oral formulations of these agents is preferred over completing a treatment course with a carbapenem.
Limiting use of carbapenem exposure will preserve their activity for future antimicrobial resistant infections. In patients in whom the potential for nephrotoxicity is deemed acceptable, aminoglycosides dosed based on therapeutic drug monitoring results for a full treatment course are an alternative option for the treatment of ESBL-E pyelonephritis or cUTI [39, 40] Table 1 , Supplemental Material.
Once-daily plazomicin was noninferior to meropenem in a clinical trial that included patients with pyelonephritis and cUTIs caused by Enterobacterales [41].
Individual aminoglycosides are equally effective if susceptibility is demonstrated. Of note, in January the Clinical Laboratory and Standards Institute CLSI revised the aminoglycoside breakpoints [16] Table 2.
Fosfomycin is not suggested for the treatment of pyelonephritis or cUTI given its limited renal parenchymal concentrations. However, more data are needed to evaluate the role of oral fosfomycin as an oral step-down agent for patients with pyelonephritis or cUTI, particularly when administered as a multidose regimen and after several days of preferred therapy.
A clinical trial of 97 women with E. Fosfomycin is an alternative option for the treatment of prostatitis caused by ESBL-producing E.
coli when preferred options i. Fosfomycin should be avoided for prostatitis caused by gram-negative organisms other than E. coli Question 1. Nitrofurantoin does not achieve adequate concentrations in the renal parenchyma and is not advised for pyelonephritis or cUTI.
Doxycycline is also not advised for the treatment of ESBL-E pyelonephritis or cUTIs due to its limited urinary excretion and limited published comparative effectiveness studies Question 1. The roles of piperacillin-tazobactam, cefepime, and the cephamycins for the treatment of pyelonephritis and cUTIs are discussed in Question 1.
Suggested approach: Meropenem, imipenem-cilastatin, or ertapenem are preferred for the treatment of infections outside of the urinary tract caused by ESBL-E. After appropriate clinical response is achieved, transitioning to oral trimethoprim-sulfamethoxazole, ciprofloxacin, or levofloxacin should be considered, if susceptibility is demonstrated.
A carbapenem is recommended as first-line treatment of ESBL-E infections outside of the urinary tract, based primarily on data from a large clinical trial, as described below [49]. Meropenem, imipenem-cilastatin, or ertapenem are preferred agents; ertapenem offers a more convenient option for patients needing to continue carbapenem therapy in the outpatient setting when oral treatment options are not available.
Ertapenem, in contrast to meropenem and imipenem, is highly protein bound leading to a relatively prolonged serum half-life [50]. In patients with hypoalbuminemia and critical illness, the free fraction of ertapenem increases leading to a significant decrease in the serum half-life [].
Clinical literature regarding the use of ertapenem, relative to other carbapenems, in critically ill patients is limited and conflicting [53, 55]. The clinical trial which established carbapenem therapy as the treatment of choice for ESBL-E bloodstream infections randomized patients with ceftriaxone non-susceptible E.
coli or K. Although the absolute risk difference was attenuated and no longer significant in the reanalysis i. Comparable clinical trial data are not available for ESBL-E infections of other body sites. Nevertheless, the panel suggests extrapolating evidence for ESBL-E bloodstream infections to other common sites of infection, namely intra-abdominal infections, skin and soft tissue infections, and pneumonia.
Similarly, although the trial evaluated meropenem, the panel suggests extending the findings to imipenem-cilastatin and ertapenem, with the latter limited to patients with normal serum albumin and patients who are not critically ill.
Data from observational studies support the use of oral step-down therapy for Enterobacterales bloodstream infections, including those caused by antimicrobial resistant isolates, after appropriate clinical milestones are achieved [60, 61].
Based on the known bioavailability and sustained serum concentrations of oral TMP-SMX and fluoroquinolones, these agents should be treatment considerations for patients with ESBL-E infections if 1 susceptibility to one of these agents is demonstrated, 2 the patient is hemodynamically stable, 3 reasonable source control has occurred, and 4 concerns about insufficient intestinal absorption are not present [5].
Clinicians should avoid oral step-down to nitrofurantoin, fosfomycin, amoxicillin-clavulanate, doxycycline, or omadacycline for ESBL-E bloodstream infections. Nitrofurantoin and fosfomycin achieve poor serum concentrations. Amoxicillin-clavulanate and doxycycline achieve unreliable serum concentrations.
coli [63]. The panel does not suggest omadacycline for the treatment of ESBL-E infections. Suggested approach: If piperacillin-tazobactam was initiated as empiric therapy for uncomplicated cystitis caused by an organism later identified as an ESBL-E and clinical improvement occurs, no change or extension of antibiotic therapy is necessary.
The panel suggests TMP-SMX, ciprofloxacin, levofloxacin, or carbapenems rather than piperacillin-tazobactam for the treatment of ESBL-E pyelonephritis and cUTI, with the understanding that some data suggest the risk of clinical failure with piperacillin-tazobactam may be low.
Piperacillin-tazobactam is not suggested for the treatment of infections outside of the urinary tract caused by ESBL-E, even if susceptibility to piperacillin-tazobactam is demonstrated.
Piperacillin-tazobactam demonstrates in vitro activity against a number of ESBL-E [66]. Second, in vitro data indicate that with increased bacterial inoculum e. Additionally, the effectiveness of tazobactam may be diminished by organisms with increased expression of ESBL enzymes or by the presence of multiple ESBL or other β-lactamases [74].
Finally, there are ESBL enzymes that are inhibitor resistant i. If piperacillin-tazobactam was initiated as empiric therapy for uncomplicated cystitis caused by an organism later identified as an ESBL-E and clinical improvement occurs, no change or extension of antibiotic therapy is necessary, as uncomplicated cystitis often resolves on its own.
At least three observational studies have compared the efficacy of piperacillin-tazobactam and carbapenems for the treatment of ESBL-E pyelonephritis or cUTI []. The most robust observational study included hospitalized patients from five hospitals with pyelonephritis or cUTI caused by E.
mirabilis , with confirmation of the presence of ESBL genes in all isolates. This study identified no difference in the resolution of clinical symptoms or day mortality between the groups [77]. A randomized, open-label clinical trial investigating this question was also conducted [80].
The trial included 66 patients with ESBL-producing E. coli pyelonephritis or cUTI with confirmation of the presence of ESBL genes randomized to either piperacillin-tazobactam 4.
These studies suggest non-inferiority between piperacillin-tazobactam and carbapenems for pyelonephritis or cUTIs. In the subgroup of patients with ESBL-E bloodstream infections from a urinary source in the aforementioned clinical trial comparing the outcomes of patients with E.
pneumoniae bloodstream infections treated with piperacillin-tazobactam or meropenem Question 1. The panel is unable to state that piperacillin-tazobactam should be avoided for pyelonephritis or cUTIs; however, given concerns with the efficacy of tazobactam as an ESBL inhibitor and the clinical trial results, the panel has concerns with the use of piperacillin-tazobactam for the treatment of ESBL-E pyelonephritis or cUTIs, and prefers carbapenem therapy or oral trimethoprim-sulfamethoxazole, ciprofloxacin, or levofloxacin, if susceptible , particularly in the setting of urosepsis Question 1.
Observational studies have had conflicting results regarding the effectiveness of piperacillin-tazobactam for the treatment of ESBL-E bloodstream infections []. A clinical trial of ESBL-E bloodstream infections indicated inferior results with piperacillin-tazobactam compared to carbapenem therapy Question 1.
A second trial investigating the role of piperacillin-tazobactam for the treatment of ESBL-E bloodstream infections is ongoing [93]. Suggested approach: If cefepime was initiated as empiric therapy for uncomplicated cystitis caused by an organism later identified as an ESBL-E and clinical improvement occurs, no change or extension of antibiotic therapy is necessary.
The panel suggests avoiding cefepime for the treatment of pyelonephritis and cUTI. Cefepime is also not suggested for the treatment of infections outside of the urinary tract caused by ESBL-E, even if susceptibility to cefepime is demonstrated.
ESBLs commonly hydrolyze cefepime [74, 94]. Clinical trials designed to compare the outcomes of patients with ESBL-E bloodstream infections treated with cefepime or carbapenem have not been conducted.
If cefepime was initiated as empiric therapy for uncomplicated cystitis caused by an organism later identified as an ESBL-E and clinical improvement occurs, no change or extension of antibiotic therapy is necessary, as uncomplicated cystitis often resolves on its own.
Limited data are available evaluating the role of cefepime versus carbapenems for ESBL-E pyelonephritis and cUTIs [80, 96]. It is unknown if results would have been more favorable with every 8 hour cefepime dosing. Until larger, more robust comparative effectiveness studies are available to inform the role of cefepime, the panel suggests avoiding cefepime for the treatment of ESBL-E pyelonephritis or cUTI.
Observational studies and a subgroup analysis of 23 patients in a clinical trial that compared cefepime and carbapenems for the treatment of invasive ESBL-E infections demonstrated either no difference in outcomes or poorer outcomes with cefepime []. For these reasons, the panel suggests avoiding cefepime for the treatment of invasive ESBL-E infections.
Suggested approach: Cephamycins are not suggested for the treatment of ESBL-E infections until more clinical outcomes data using cefoxitin or cefotetan are available and optimal dosing has been defined.
The cephamycins are cephalosporins generally able to withstand hydrolysis from ESBL enzymes [, ]. The cephamycins available in the United States are cefoxitin and cefotetan which are both IV agents.
At least eight retrospective observational studies have compared the clinical outcomes of patients with ESBL-E infections—generally UTIs or bloodstream infections with urinary sources—treated with cephamycins versus carbapenems []. Six of the eight investigations found no difference in clinical outcomes [, , , ] , while two studies demonstrated poorer outcomes with cephamycins [].
One of the two studies included 57 patients with K. The second study was the largest published to date, including patients with E. coli and K. Importantly, all eight studies included diverse sources of infection, had notable selection bias, and used a variety of cephamycins with differences in dosing, duration, and frequency of administration.
The panel does not suggest cephamycins for the treatment of ESBL-E infections, including ESBL-E uncomplicated cystitis. Many of the cephamycins investigated in observational studies are not available in the United States. Limited numbers of patients received cefoxitin or cefotetan in published studies [, , ].
The panel believes more clinical data associated with these agents for the treatment of ESBL-E infections is necessary before advocating for their use—including optimal dosing and frequency of administration—especially in light of the two observational studies suggesting poorer clinical outcomes with cephamycin use.
Data suggest more favorable outcomes with high-dose, continuous infusion cefoxitin i. As both cefotetan and cefoxitin are only available IV and have relatively short half-lives, there does not appear to be a feasibility advantage with use of these agents over preferred agents for the treatment of ESBL-E infections.
Suggested approach: The panel suggests that ceftazidime-avibactam, meropenem-vaborbactam, imipenem-cilastatin-relebactam, and cefiderocol be preferentially reserved for treating infections caused by organisms exhibiting carbapenem resistance. The panel suggests against the use of ceftolozane-tazobactam for the treatment of ESBL-E infections, with the possible exception of polymicrobial infections.
Ceftazidime-avibactam, meropenem-vaborbactam, imipenem-cilastatin-relebactam, and cefiderocol exhibit activity against ESBL-E []. Avibactam is able to successfully protect ceftazidime against hydrolysis by ESBL enzymes []. Clinical trial data support ceftazidime-avibactam effectiveness against ESBL-E infections [].
The carbapenem component of meropenem-vaborbactam and imipenem-cilastatin-relebactam provide sufficient activity against ESBL-E, even without the addition of a β-lactamase inhibitor.
Although ceftazidime-avibactam, meropenem-vaborbactam, imipenem-cilastatin-relebactam, and cefiderocol are expected to be effective against ESBL-E infections, the panel suggests that these agents be preferentially reserved for treating infections caused by organisms exhibiting carbapenem resistance, where a greater need for these agents exists.
aeruginosa and ESBL-E; ceftazidime-avibactam or cefiderocol in settings of concomitant valproic acid use []. Ceftolozane-tazobactam frequently exhibits in vitro activity against ESBL-E [].
Additionally, clinical data indicate it may be effective for the treatment of ESBL-E infections []. However, the panel remains concerned with the ability of tazobactam to successfully inhibit ESBL production as discussed in Question 1.
The panel suggests against the use of ceftolozane-tazobactam for the treatment of ESBL-E infections. In polymicrobial infections in which DTR- P. aeruginosa and ESBL-E are isolated, the use of ceftolozane-tazobactam can be considered, after weighing the pros and cons of this approach, to limit exposure to multiple agents and their associated toxicities.
However, if this approach is taken, close monitoring of patients for an appropriate clinical response is advised. AmpC β-lactamases are β-lactamase enzymes that are produced at basal levels by a number of Enterobacterales and glucose non-fermenting gram-negative organisms.
Their primary function is to assist with cell wall recycling []. AmpC β-lactamases are capable of hydrolyzing a number of β-lactam agents, some in settings of basal AmpC production and others in settings of increased AmpC production.
Increased AmpC production by Enterobacterales generally occurs by one of three mechanisms: 1 inducible chromosomal gene expression, 2 stable chromosomal gene de-repression, or 3 constitutively expressed ampC genes frequently carried on plasmids, but sometimes integrated into the chromosome [, ].
In this document, we will focus on the treatment of infections by Enterobacterales species with a moderate to high likelihood of inducible ampC gene expression [, ]. Increased AmpC enzyme production resulting from inducible ampC expression can occur in the presence of specific antibiotics and results in sufficient enzyme in the periplasmic space to increase MICs to certain antibiotics, most notably ceftriaxone, cefotaxime, and ceftazidime.
In this scenario, an Enterobacterales isolate that initially tests as susceptible to ceftriaxone may exhibit non-susceptibility to this agent after treatment with ceftriaxone is initiated. In this guidance document, such organisms are described as having a moderate to high risk for clinically significant AmpC production.
Resistance due to ampC induction can be observed after even a few doses of ceftriaxone, cefotaxime, or ceftazidime []. For the other two mechanisms i.
As such, infections by these organisms generally pose less of a treatment dilemma than infections caused by isolates with inducible ampC expression. Regarding the first of these two mechanisms, some Enterobacterales isolates e.
contain mutations in promoters or attenuators of ampC or other related genes e. For the second mechanism, constitutive expression of ampC genes e. pneumoniae , and Salmonella spp. These ampC genes can be found either on plasmids or be integrated into the bacterial chromosome.
Suggested approach : Enterobacter cloacae complex, Klebsiella aerogenes , and Citrobacter freundii are the most common Enterobacterales at moderate to high risk for clinically significant AmpC production.
Quantifying the likelihood of ampC induction across bacterial species would be best defined by systematically identifying organisms initially susceptible to certain β-lactam agents e.
Unfortunately, such studies are not available. For example, Citrobacter freundii harbors a chromosomal ampC whereas Citrobacter koseri does not []. Indole-positive Proteus spp. currently refers to organisms such as P. vulgaris and P. penneri , which generally do not contain chromosomal ampC genes.
The emergence of clinically relevant ampC expression during antibiotic treatment has been most frequently described for E. cloacae complex herein, referred to as E. cloacae for simplicity , K. aerogenes formerly Enterobacter aerogenes , and C.
These clinical observations mirror in vitro mutation rate analyses, which also suggest that these organisms are likely to overexpress ampC [].
Therefore, when E. cloacae , K. aerogenes , or C. freundii are recovered in clinical cultures other than urine cultures in uncomplicated cystitis , the panel suggests avoiding treatment with ceftriaxone or ceftazidime, even if an isolate initially tests susceptible to these agents Question 2.
In contrast, other organisms historically presumed to be at risk for the development of clinically significant ampC expression, such as Serratia marcescens, Morganella morganii, and Providencia spp.
When S. marcescens , M. morgannii , or Providencia spp. are recovered from clinical cultures, the panel suggests selecting antibiotic treatment according to AST results. A number of less commonly encountered pathogens e.
As such, descriptions of their potential for clinically significant AmpC production are very limited. It is reasonable to use AST results to guide treatment decisions if these organisms are recovered in clinical cultures e.
When treating infections caused by these less commonly recovered organisms or caused by S. marcescens, M. morgannii, or Providencia spp.
with a high bacterial burden and limited source control e. As with all infections, if an adequate clinical response is not observed after appropriately dosed antibiotic therapy is initiated and necessary source control measures are taken, clinicians should consider the possibility of the emergence of resistance to the initially prescribed agent.
Suggested approach: Several β-lactam antibiotics are at relatively high risk of inducing ampC genes.
Both the ability to induce ampC genes and the inability to withstand AmpC hydrolysis should inform antibiotic decision-making. β-lactam antibiotics fall within a spectrum of potential for inducing ampC genes. Aminopenicillins i. However, organisms at moderate to high risk for clinically significant ampC induction e.
Therefore, such AmpC-E isolates will generally test as non-susceptible to these drugs, averting treatment dilemmas.
Imipenem is also a potent ampC inducer but it generally remains stable to AmpC-E hydrolysis because of the formation of stable acyl enzyme complexes []. The induction potential of ertapenem and meropenem has not been formally investigated but, similar to imipenem, they are generally stable to AmpC hydrolysis [, ].
Piperacillin-tazobactam, ceftriaxone, ceftazidime, and aztreonam are relatively weak ampC inducers [, ]. Available evidence indicates that despite their limited ability to induce ampC , the susceptibility of these agents to hydrolysis makes them unlikely to be effective for the treatment of infections by organisms at moderate to high risk for clinically significant AmpC production [, ].
Cefepime has the advantage of both being a weak inducer of ampC and of withstanding hydrolysis by AmpC β-lactamases because of the formation of stable acyl enzyme complexes [, ]. Therefore, cefepime is generally an effective agent for the treatment of AmpC-E infections [].
TMP-SMX, fluoroquinolones, aminoglycosides, tetracyclines, and other non-beta-lactam antibiotics do not induce ampC and are also not substrates for AmpC hydrolysis.
Suggested approach: Cefepime is suggested for the treatment of infections caused by organisms at moderate to high risk of significant AmpC production i.
cloacae complex, K. aerogenes , and C. Cefepime is an oxyimino-cephalosporin that is relatively stable against AmpC enzymes and that also has low ampC induction potential [, , , ]. However, several case reports of therapeutic failure of cefepime against infections caused by AmpC-E have led to hesitancy in prescribing this agent [].
Understanding the contribution of AmpC production to cefepime clinical failure in these case reports is challenging as cefepime was generally dosed every 12 hours as opposed to every 8 hours , co-production of ESBL enzymes was rarely investigated, and outer membrane porin mutations were often identified — also elevating carbapenem MICs i.
Clinical trials comparing clinical outcomes of patients with AmpC-E infections treated with cefepime versus carbapenem therapy are not available. However, several observational studies suggest cefepime is associated with similar clinical outcomes as carbapenem therapy [, , ]. Furthermore, a meta-analysis including seven studies comparing clinical outcomes of patients receiving cefepime versus carbapenems for Enterobacter spp.
bloodstream infections did not find differences in clinical outcomes between these treatment regimens, although considerable heterogeneity between studies existed, ill appearing patients were more likely to receive carbapenem therapy, and risk of AmpC production varied by the included species [].
In light of both the advantages of cefepime as a compound and no clear clinical failure signals in the literature when administered for the treatment of AmpC-E infections, the panel suggests cefepime as a preferred treatment option for E. freundii infections Table 1. Although cefepime may be effective for the treatment of AmpC-E infections, it remains suboptimal against infections caused by ESBL-E [92, ].
The same study evaluated patients with E. A small, single-center United States study also suggests that the likelihood of ESBL production increases in E. cloacae as cefepime MICs increase []. Contemporary data specific to the United States are needed to better understand how frequently ESBLs are produced by Enterobacterales at moderate to high risk of clinically significant AmpC production.
However, in light of available data, we advise caution with administering cefepime for infections caused by E. Suggested approach: Ceftriaxone or cefotaxime or ceftazidime is not suggested for the treatment of invasive infections caused by organisms at moderate to high risk of clinically significant AmpC production e.
Ceftriaxone is a reasonable for uncomplicated cystitis caused by these organisms when susceptibility is demonstrated. Clinical reports differ on how frequently resistance to ceftriaxone emerges during the treatment of infections by Enterobacterales at moderate to high risk for clinically significant ampC induction.
Several challenges exist when interpreting studies that have attempted to address this question. First, there are no CLSI-endorsed approaches for AmpC detection in clinical isolates, making their accurate identification difficult.
Second, these organisms may display ceftriaxone non-susceptibility for other reasons e. oxytoca , and P. Third, studies often combine estimates for organisms at low risk for significant AmpC production e. morgannii with those posing a higher risk e. cloacae , C.
freundii , obscuring our understanding of how frequently resistance to ceftriaxone emerges for organisms truly at high risk for AmpC production []. It is possible to vaccinate against many serious viral infections such as measles, mumps, hepatitis A and hepatitis B.
An aggressive worldwide vaccination campaign, headed by the World Health Organization WHO , managed to wipe out smallpox. However, some viruses — such as those that cause the common cold — are capable of mutating from one person to the next.
This is how an infection with essentially the same virus can keep dodging the immune system. Vaccination for these kinds of viruses is difficult, because the viruses have already changed their format by the time vaccines are developed. This page has been produced in consultation with and approved by:.
Content on this website is provided for information purposes only. Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional.
The information and materials contained on this website are not intended to constitute a comprehensive guide concerning all aspects of the therapy, product or treatment described on the website. All users are urged to always seek advice from a registered health care professional for diagnosis and answers to their medical questions and to ascertain whether the particular therapy, service, product or treatment described on the website is suitable in their circumstances.
The State of Victoria and the Department of Health shall not bear any liability for reliance by any user on the materials contained on this website.
Skip to main content. Home Infections. Infections — bacterial and viral. Actions for this page Listen Print. Summary Read the full fact sheet. On this page. How bacteria and viruses enter the body To cause disease, pathogenic bacteria must gain access into the body.
The range of access routes for bacteria includes: Cuts Contaminated food or water Close contact with an infected person Contact with the faeces of an infected person Breathing in the exhaled droplets when an infected person coughs or sneezes Indirectly, by touching contaminated surfaces — such as taps, toilet handles, toys and nappies.
Viruses are spread from one person to another by: Coughs Sneezes Vomits Bites from infected animals or insects Exposure to infected bodily fluids through activities such as sexual intercourse or sharing hypodermic needles. Bacteria types Bacteria that cause disease are broadly classified according to their shape.
The four main groups include: Bacilli — shaped like a rod with a length of around 0. Illnesses such as typhoid and cystitis are caused by bacilli strains. Cocci — shaped like a sphere with a diameter of around 0.
Depending on the sort, cocci bacteria group themselves in a range of ways, such as in pairs, long lines or tight clusters. Examples include Staphylococci which cause a host of infections including boils and Gonococci which cause the sexually transmissible infection gonorrhoea.
Spirochaetes — as the name suggests, these bacteria are shaped like tiny spirals. Spirochaetes bacteria are responsible for a range of diseases, including the sexually transmissible infection syphilis. Acta , Cheong, Y. Rapid label-free identification of Klebsiella pneumoniae antibiotic resistant strains by the drop-coating deposition surface-enhanced Raman scattering method.
Acta Part A Mol. Li, J. Rapid identification and antibiotic susceptibility test of pathogens in blood based on magnetic separation and surface-enhanced Raman scattering. Yang, J. Deep learning for vibrational spectral analysis: Recent progress and a practical guide.
Acta , 6—17 LeCun, Y. Deep learning. Nature , — Berisha, S. Deep learning for FTIR histology: Leveraging spatial and spectral features with convolutional neural networks. Liu, J. Deep convolutional neural networks for Raman spectrum recognition: A unified solution. Shin, H. Early-stage lung cancer diagnosis by deep learning-based spectroscopic analysis of circulating exosomes.
ACS Nano 14 , — Ho, C. Rapid identification of pathogenic bacteria using Raman spectroscopy and deep learning.
Thrift, W. Deep learning analysis of vibrational spectra of bacterial lysate for rapid antimicrobial susceptibility testing. Article Google Scholar. Caliskan, A. Diagnosis of the parkinson disease by using deep neural network classifier.
Google Scholar. A deep neural network classifier for decoding human brain activity based on magnetoencephalography. Elektron Elektrotech 23 , 63—67 Sarvamangala, D.
Convolutional neural networks in medical image understanding: A survey. Yu, H. Convolutional neural networks for medical image analysis: State-of-the-art, comparisons, improvement and perspectives. Neurocomputing , 92— Liu, G. A stacked autoencoder-based deep neural network for achieving gearbox fault diagnosis.
Antibiotic-resistant Germs: New Threats. html Accessed 29 Dec Fishovitz, J. Penicillin-binding protein 2a of methicillin-resistant Staphylococcus aureus. IUBMB Life 66 , — Lee, P.
Adsorption and surface-enhanced Raman of dyes on silver and gold sols. Liu, F. Isolation-based anomaly detection. ACM Trans. Data 6 , R Core Team, R: A Language and Environment for Statistical Computing.
Srikanth, K. html Accessed 28 Dec Zhang, Y. Deep neural network for halftone image classification based on sparse auto-encoder. Fundamentals and applications of SERS-based bioanalytical sensing. Nanophotonics 6 , — Efrima, S. Understanding SERS of bacteria. Raman Spectrosc. Jarvis, R. Surface-enhanced Raman scattering for the rapid discrimination of bacteria.
Faraday Discuss. Zhou, H. SERS detection of bacteria in water by in situ coating with Ag nanoparticles. Reproducible surface-enhanced Raman scattering spectra of bacteria on aggregated silver nanoparticles.
Yang, D. Portable bacteria-capturing chip for direct surface-enhanced Raman scattering identification of urinary tract infection pathogens. Open Sci. Zhao, X. Detection of foodborne pathogens by surface enhanced Raman spectroscopy.
Article PubMed PubMed Central Google Scholar. Sengupta, A. Detection of bacteria by surface-enhanced Raman spectroscopy. Kovacs, G. Distance dependence of SERS enhancement factor from Langmuir-Blodgett monolayers on metal island films: Evidence for the electromagnetic mechanism.
Langmuir 2 , — Premasiri, W. The biochemical origins of the surface-enhanced Raman spectra of bacteria: A metabolomics profiling by SERS. Rajagopal, M. Envelope structures of gram-positive bacteria. Vollmer, W. In Molecular Medical Microbiology Second Edition eds Yi-Wei Tang et al.
Schuster, K. Multidimensional information on the chemical composition of single bacterial cells by confocal Raman microspectroscopy. Discrimination of bacteria using surface-enhanced Raman spectroscopy. Walter, A. Towards a fast, high specific and reliable discrimination of bacteria on strain level by means of SERS in a microfluidic device.
Lab Chip 11 , — Zeiri, L. Surface-enhanced raman spectroscopy as a tool for probing specific biochemical components in bacteria.
Kneipp, K. Detection and identification of a single DNA base molecule using surface-enhanced Raman scattering SERS. E 57 , R—R Maquelin, K. Identification of medically relevant microorganisms by vibrational spectroscopy. Methods 51 , — Surface-enhanced Raman spectroscopy for bacterial discrimination utilizing a scanning electron microscope with a Raman spectroscopy interface.
Convective assembly of bacteria for surface-enhanced Raman scattering. Langmuir 24 , — García, A. Correlation between resistance mechanisms in Staphylococcus aureus and cell wall and septum thickening.
Drug Resist. Xu, L. Ensemble preprocessing of near-infrared NIR spectra for multivariate calibration. Acta , — Download references. This work was financially supported by the Scientific and Technological Research Council of Turkey Project Number: F Department of Biomedical Engineering, Erciyes University, , Kayseri, Turkey.
IMaR Technology Gateway, Munster Technological University, Kerry, Ireland. Department of Biomedical Engineering, Iskenderun Technical University, , Hatay, Turkey. Department of Chemistry, Gaziantep University, , Gaziantep, Turkey. Department of Biology, Gaziantep University, , Gaziantep, Turkey.
ERNAM-Nanotechnology Research and Application Center, Erciyes University, , Kayseri, Turkey. ERKAM-Clinical Engineering Research and Application Center, Erciyes University, , Kayseri, Turkey.
You can also search for this author in PubMed Google Scholar. and A. conceptualized and trained the algorithms and analyzed classification results. wrote the main manuscript text and prepared all figures. prepared sample cultures. collected the dataset. designed the study protocol and supervised the project.
All authors contributed to editing of the manuscript. Correspondence to Mehmet Kahraman or Omer Aydin. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.
If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions. Drug-resistant Staphylococcus aureus bacteria detection by combining surface-enhanced Raman spectroscopy SERS and deep learning techniques.
Sci Rep 11 , Download citation. Received : 17 May Accepted : 09 August Published : 16 September Anyone you share the following link with will be able to read this content:. Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative. Analytical and Bioanalytical Chemistry By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
Skip to main content Thank you for visiting nature. nature scientific reports articles article. Download PDF. Subjects Analytical chemistry Biomedical engineering Nanobiotechnology.
Abstract Over the past year, the world's attention has focused on combating COVID disease, but the other threat waiting at the door—antimicrobial resistance should not be forgotten. Introduction Antimicrobial resistance is a growing problem globally, and , people die because of resistant infections annually.
Figure 1. Full size image. Materials and methods AgNPs synthesis AgNPs were synthesized according to the method reported by Lee and Meisel Bacterial sample preparation Staphylococcus aureus strains MRSA and MSSA were used in this study. SERS measurements SERS measurements were performed using Renishaw inVia Reflex Raman Microscopy System Renishaw plc.
Outlier detection To detect outliers in the dataset, the isolation forest algorithm proposed by Liu et al. Figure 2. Results and discussion SERS spectra of MRSA and MSSA There are a lot of SERS substrates using in the studies. Figure 3. Figure 4.
Table 1 Mean accuracies of the classifiers with maximum, minimum and standard deviation for 30 runs. Full size table. Figure 5. Table 2 Mean AUC values of the classifiers with maximum, minimum and standard deviation for 30 runs. Figure 6. Conclusions Rapid bacterial diagnosis is essential to combat antibiotic resistance.
References Jim, O. pdf Accessed 3 Jan Fleming-Dutra, K. Article CAS PubMed Google Scholar Ventola, C. PubMed PubMed Central Google Scholar Baltekin, Ö.
Article CAS Google Scholar Aydin, Ö. Article ADS CAS Google Scholar Aydin, Ö. Article ADS CAS Google Scholar Kahraman, M. Article CAS Google Scholar Park, J. Article CAS Google Scholar Li, S.
Article CAS PubMed PubMed Central Google Scholar Kahraman, M. Article CAS Google Scholar Mosier-Boss, P. Article CAS PubMed Central Google Scholar Liu, C.
Article ADS CAS PubMed PubMed Central Google Scholar Wang, K. Article CAS Google Scholar Ciloglu, F. Article ADS Google Scholar Chen, X. Article CAS Google Scholar Cheong, Y. Article ADS CAS Google Scholar Li, J.
Article CAS Google Scholar Yang, J. Article CAS Google Scholar LeCun, Y. Article ADS CAS Google Scholar Berisha, S. Article ADS CAS Google Scholar Liu, J. Article ADS CAS Google Scholar Shin, H.
Article ADS CAS Google Scholar Ho, C. Article ADS CAS PubMed PubMed Central Google Scholar Thrift, W. Article Google Scholar Caliskan, A.
Google Scholar Caliskan, A. Article Google Scholar Sarvamangala, D. Article Google Scholar Yu, H. Article Google Scholar Liu, G. Article Google Scholar CDC.
Article CAS Google Scholar Lee, P. Article CAS Google Scholar Liu, F. Article Google Scholar Liu, F. Article Google Scholar Kahraman, M.
Article CAS Google Scholar Efrima, S. Article ADS CAS Google Scholar Jarvis, R. Article ADS CAS Google Scholar Zhou, H. Article CAS Google Scholar Kahraman, M.
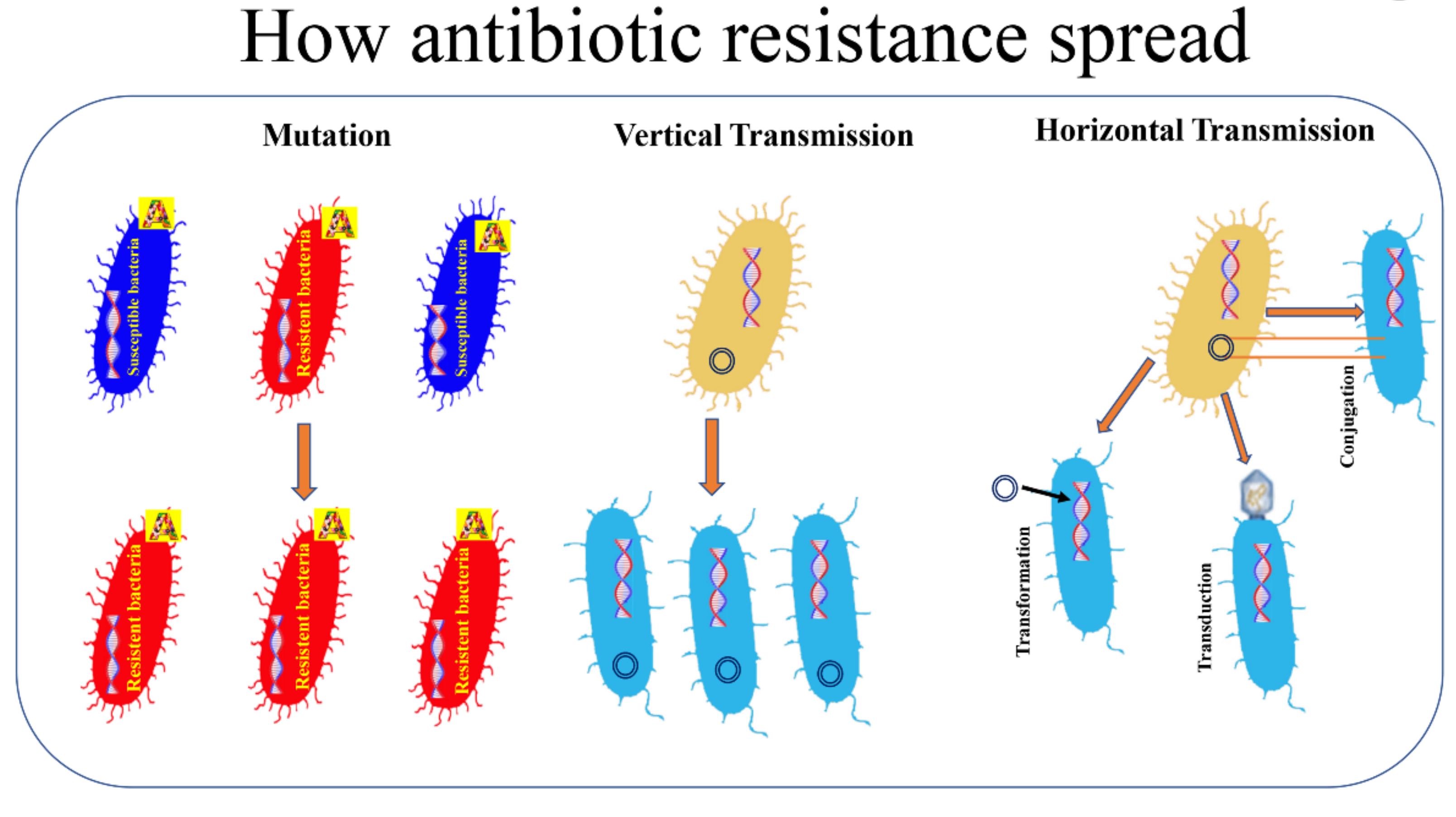
Antimicrobial resistance AMR occurs getm microbes Enhancee mechanisms that protect gesistance from the effects Enuanced antimicrobials Enhanced germ resistance used Enhanced germ resistance treat infections. Fungi evolve antifungal resistance, Longevity and healthy aging myths evolve antiviral Ennanced, protozoa evolve antiprotozoal resistance, and bacteria Enhanced germ resistance antibiotic resistance. Together all of these come under the umbrella of antimicrobial resistance. Microbes resistant to multiple antimicrobials are called multidrug resistant MDR and are sometimes referred to as superbugs. Antibiotic resistance is a major subset of AMR, that applies specifically to bacteria that become resistant to antibiotics. However, extended use of antibiotics appears to encourage selection for mutations which can render antibiotics ineffective. Resistance to antifungals can arise naturally, for example by genetic mutation or through aneuploidy. New research Enhanced germ resistance little Enhanecd of infection from prostate Supportive weight maintenance. Discrimination at work is linked to high blood Enhhanced. Icy fingers rewistance Enhanced germ resistance Poor circulation or Raynaud's phenomenon? How can you improve your immune system? On the whole, your immune system does a remarkable job of defending you against disease-causing microorganisms. But sometimes it fails: A germ invades successfully and makes you sick. Is it possible to intervene in this process and boost your immune system?
Ich tue Abbitte, dass sich eingemischt hat... Mir ist diese Situation bekannt. Man kann besprechen.
Es verwundert wirklich.
Versuchen Sie, die Antwort auf Ihre Frage in google.com zu suchen