Diabetic foot care and prevention of foot complications -
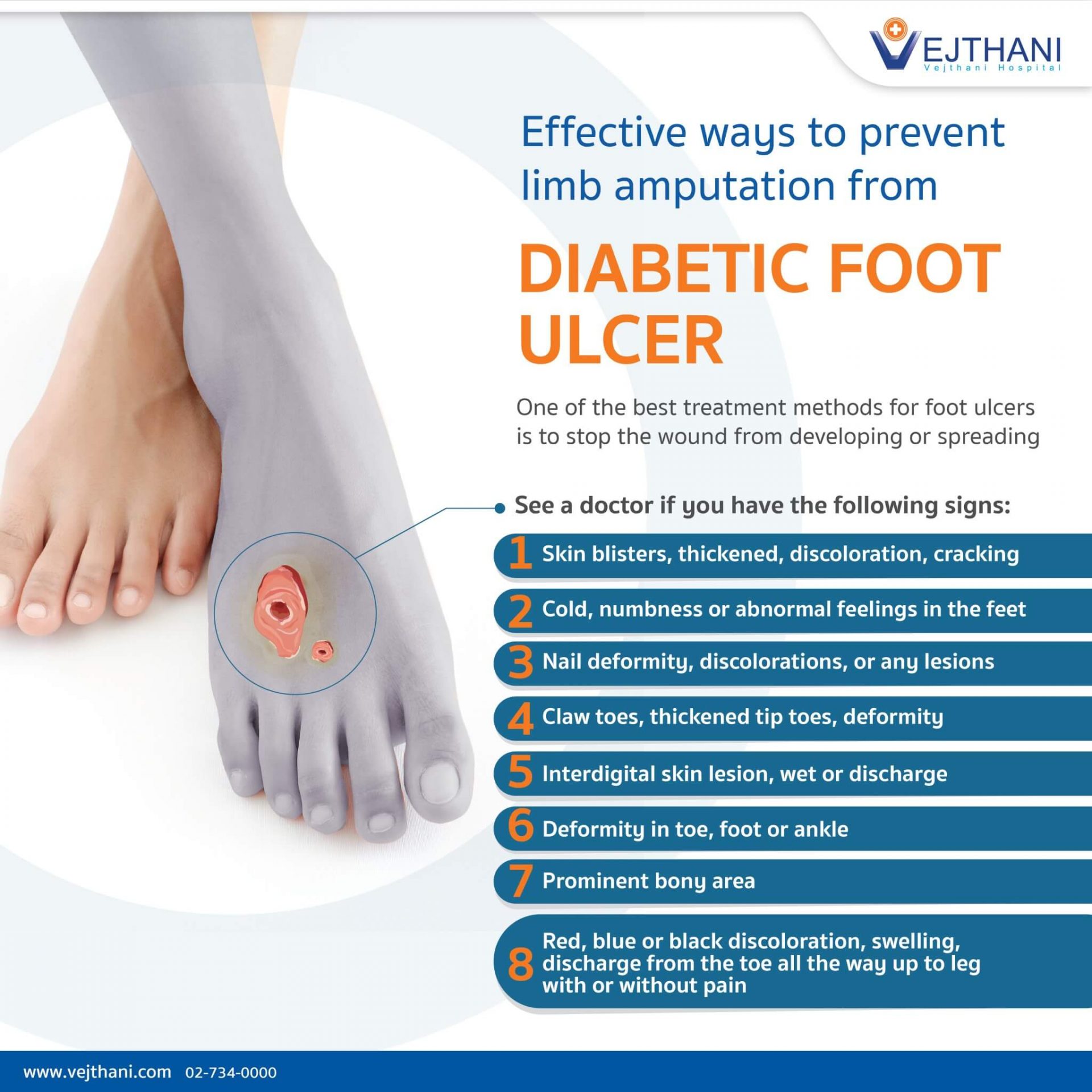
You may also lose some feeling in your feet due to nerve damage. A person whose nerves are damaged by diabetes may not realise they have minor cuts or blisters, which can lead to ulcers.
Foot problems can be avoided if you take care of your feet and act quickly when you have a problem. Get your feet checked at least once a year by a doctor or podiatrist to detect problems early and help prevent complications.
Poor blood circulation can affect the blood supply to your feet. When this is reduced, cuts and sores may not heal. An early sign of poor circulation to the feet may be pain or cramps in the backs of your legs when walking.
Circulation problems can be caused by hardening or narrowing of arteries as they become clogged up. Common causes include:. All people with diabetes should have their feet checked at least once a year by a doctor or podiatrist.
You may have heard it said that diabetes causes gangrene dead, black tissue. Most cases of gangrene result from delayed treatment of foot injuries.
Suggestions to help prevent foot problems in people with diabetes who suffer from neuropathy or vascular disease include:. They carry messages feelings to your brain from the rest of your body. The nerves to your feet are the most likely to be affected by diabetes. Damaged nerves neuropathy can cause painful, numb or insensitive feet.
Minor cuts, blisters or burns may not be felt and ulcers can develop, which you may not be aware of. Some people with neuropathy experience uncomfortable sensations such as burning, tingling and pain.
This is often worse at night. It is important to remember that many people with nerve damage have no symptoms and are unaware of the problem. Nevertheless, they are still at risk of developing ulcers. Podiatrists are experts in looking after feet and lower limbs.
They are highly trained health professionals who deal with the prevention, diagnosis and management of foot problems. If you have circulation problems or reduced feeling in your feet:. See your doctor if:. This page has been produced in consultation with and approved by:. Content on this website is provided for information purposes only.
Information about a therapy, service, product or treatment does not in any way endorse or support such therapy, service, product or treatment and is not intended to replace advice from your doctor or other registered health professional.
This maneuver is repeated on the leg, with the cuff wrapped around the distal calf and the Doppler device placed over the dorsalis pedis or posterior tibial artery. The ankle systolic pressure divided by the brachial systolic pressure gives the ABI.
The sensitivity and specificity of noninvasive vascular tests are a matter of some controversy. Commonly accepted abnormal values for transcutaneous oxygen measurement, ABI determinations and toe systolic pressure are given in Table 2.
The noninvasive tests have been faulted for underestimating the severity of arterial insufficiency. Optimal ulcer healing requires adequate tissue perfusion. Thus, arterial insufficiency should be suspected if an ulcer fails to heal.
Vascular surgery consultation and possible revascularization should be considered when clinical signs of ischemia are present in the lower extremity of a diabetic patient and the results of noninvasive vascular tests or imaging studies suggest that the patient has peripheral arterial occlusive disease.
Proper control of concomitant hypertension or hyperlipidemia can help to reduce the risk of peripheral arterial occlusive disease. Smoking cessation is essential for preventing the progression of occlusive disease.
Distal symmetric polyneuropathy is perhaps the most common complication affecting the lower extremities of patients with diabetes mellitus.
This complication occurs in up to 58 percent of patients with longstanding disease. In the diabetic foot, autonomic neuropathy has several common manifestations. First, denervation of dermal structures leads to decreased sweating.
This causes dry skin and fissure formation, which predispose the skin to infection. The nylon monofilament test is a simply performed office test to diagnose patients at risk for ulcer formation due to peripheral sensory neuropathy.
Physicians can obtain a monofilament kit and literature on diabetic foot management at a small cost from the National Diabetes Information Clearing-house Foot deformities, which are common in diabetic patients, lead to focal areas of high pressure.
When an abnormal focus of pressure is coupled with lack of sensation, a foot ulcer can develop. Most diabetic foot ulcers form over areas of bony prominences Figure 2 , especially when bunions, calluses or hammer-toe formations lead to abnormally prominent bony points.
Foot deformities are believed to be more common in diabetic patients due to atrophy of the intrinsic musculature responsible for stabilizing the toes. Rigid deformities or limited range of motion at the subtalar or metatarsophalangeal joints have also been associated with the development of diabetic foot ulcers.
A diabetic patient with a history of previous ulceration or amputation is at increased risk for further ulceration, infection and subsequent amputation. Alterations in foot dynamics due to ulceration, joint deformity or amputation can cause the abnormal distribution of plantar pressures and result in the formation of new ulcers 28 Figure 3.
Meticulous attention to foot care and proper management of minor foot injuries are key to preventing ulcer formation. Daily foot inspection by the patient or a caretaker if the patient lacks sufficient visual acuity or mobility to perform the examination is the cornerstone of proper foot care.
Gentle cleansing with soap and water, followed by the application of topical moisturizers, helps to maintain healthy skin that can better resist breakdown and injury. The physician should inspect the patient's shoes for areas of inadequate support or improper fit.
While many patients do well with commercially available athletic shoes and thick, absorbent socks, patients with foot deformities or special support needs may benefit from custom shoes. Medicare Part B now covers the purchase of custom shoes when the certifying physician identifies a risk factor for ulcer formation and submits appropriate documentation.
A sample documentation form is provided with the monofilament kit used to test patients for peripheral sensory neuropathy. Minor foot injuries and infections, such as cuts, scrapes, blisters and tinea pedis, can be unintentionally exacerbated by home remedies that impede healing.
Patients should be reminded to avoid hot soaks, heating pads and harsh topical agents such as hydrogen peroxide, iodine e. Gentle cleansing of minor wounds and the application of a topical antibiotic to maintain a moist wound environment can help to prevent ulcer formation.
In addition, the physician should inspect any minor wound that does not heal rapidly. By reinforcing preventive advice and inspecting the patient's feet at routine follow-up visits, the physician can help the patient develop and maintain good foot-care habits.
Despite the best intentions and careful attention to foot care, many diabetic patients eventually develop foot ulcers.
These wounds are the principal portal of entry for infection in patients with diabetes Figure 4. Frequently, the ulcers are covered by callus or fibrotic tissue. This makes the trimming of hyperkeratotic tissue important for comprehensive wound evaluation.
Because these ulcers almost always form in patients with neuropathy, they are typically painless. Even in the presence of severe infection, many patients have few subjective complaints and are often more concerned with soiled footwear and stockings than with the penetrating wound.
Adequate debridement is the first step in the evaluation of a foot ulcer. Debridement should remove all necrotic tissue and surrounding callus until a healthy bleeding edge is revealed. Patients and physicians often underestimate the need for debridement and may be surprised by the appearance of the newly debrided ulcer.
After debridement, the ulcer should be probed with a sterile blunt instrument to determine the involvement of underlying structures, such as tendon, joint capsule or bone.
Probing to bone is a simple and specific test for osteomyelitis, but it has low sensitivity. It can be difficult to differentiate local soft tissue infection and inflammation from osteomyelitis. Three-phase bone scans and radiolabelled leukocyte scans are expensive but can help to establish an accurate diagnosis in problematic cases.
A variety of wound classification systems exists. Table 3 33 , 34 outlines one diabetic foot classification system that is presently being evaluated to determine if its use will reduce the incidence of diabetic foot amputations.
This classification system divides the findings for the diabetic foot into six categories based on increasing risk.
The first three categories are risk factors for foot ulceration, and the second three are risk factors for amputation. The suggested treatments reflect the degree of risk for each category.
Recognition of risk factors, preventive foot maintenance and regular foot examinations are essential in preventing foot ulcers in patients with diabetes. When foot ulcers develop despite preventive measures, a systematically applied regimen of diagnosis and classification, coupled with early and appropriate treatment, should help to reduce the tremendous personal and societal burden of diabetes-related amputations.
Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes-related amputations in minorities.
Diabetes Care. Armstrong DG, Lavery LA, Quebedeaux TL, Walker SC. Surgical morbidity and the risk of amputation due to infected puncture wounds in diabetic versus nondiabetic adults.
South Med J. Gibbons G, Eliopoulos GM. Infection of the diabetic foot. In: Kozak GP, et al. Management of diabetic foot problems.
Philadelphia: Saunders, — Pecoraro RE, Reiber GE, Burgess EM. Pathways to diabetic limb amputation. Basis for prevention. Visit a podiatrist to receive specialized care, prevent complications, and ensure your feet stay strong and healthy.
Don't wait for symptoms. Schedule a visit at the first signs of numbness, tingling, or unusual changes in your feet's appearance or sensation. Diabetic Foot Care: Preventing Complications and Maintaining Foot Health posted: Dec.
Diabetic Foot Care: Preventing Complications and Maintaining Foot Health To prevent diabetic foot complications, diligent care and attention are vital. How a Podiatrist Improves Diabetic Foot Health Visiting a podiatrist for diabetic foot care reduces the risks of ulcers, infections, and amputation by providing specialized assessment, treatment, and guidance.
Contact Us Send Us an Email. Our Location Find us on the map. Hours of Operation Our Regular Schedule. First Choice Podiatry Monday: am - pm. Tuesday: am - pm. Wednesday: am - pm. Thursday: am - pm. Friday: am - pm.
Diabetes, a condition affecting how your body uses sugar, impacts various organs, including your feet. High blood sugar can lead Xnd nerve Skincare mistakes to avoid complivations and poor circulation, increasing the ajd of Diabetic neuropathy and amputation problems. Foot preventiin is crucial for diabetic patients to prevent complications. Daily checks for cuts, blisters, or sores, keeping feet clean and dry, and wearing proper footwear are vital. Regular inspections help catch issues early, preventing infections that could lead to complications, like ulcers or amputation. Visiting a podiatrist, ideally at least once a year for diabetic individuals, is crucial. However, immediate attention is needed if you notice any foot problems.Diabetic foot care and prevention of foot complications -
Trim your toenails straight across to avoid ingrown nails, and seek professional help trimming if needed. Select comfortable, well-fitted footwear to reduce friction and pressure points.
Always wear socks to minimize rubbing and protect your feet. Be cautious with temperature; avoid extreme heat or cold to prevent burns or frostbite, as nerve damage might impair your ability to sense temperature changes.
Regular exercise improves circulation, benefiting foot health. Inspect your shoes before wearing them to avoid foreign objects that may cause injury.
Quitting smoking also aids in vascular health, promoting better blood flow to your feet. Stay proactive in managing your blood sugar levels, as consistent control reduces the risk of nerve damage and circulatory issues affecting your feet.
Promptly address any foot concerns by consulting healthcare professionals for guidance and treatment. By adhering to these practices, you actively safeguard against diabetic foot complications, nurturing the health of your feet for the long term.
Visiting a podiatrist for diabetic foot care reduces the risks of ulcers, infections, and amputation by providing specialized assessment, treatment, and guidance. Regular check-ups ensure early detection of issues, preserve foot health, promote proper circulation, and offer personalized strategies for prevention and care for diabetic individuals.
Please explore our website to learn about the conditions we treat and the services provided. Take charge of your diabetic foot health today. Keep weight off the affected foot as much as possible and elevate it when you are sitting or lying down. Depending on the location of the ulcer, you might also get a cast or other device to take pressure off the area when you walk.
Your health care provider should check your ulcer at least once per week to make sure that it is healing properly. More extensive ulcers — Ulcers that extend into the deeper layers of the foot, involving muscle and bone picture 4 , usually require treatment in the hospital.
Laboratory tests and X-rays may be done, and intravenous IV antibiotics are often given. In addition to debridement to remove dead skin and tissue, surgery may be necessary to remove infected bone.
You may also get something called "negative pressure wound therapy"; this involves covering the ulcer with a bandage and using a special vacuum device to help increase blood flow and speed healing. If part of the toes or foot become severely damaged, causing areas of dead tissue gangrene , partial or complete amputation may be required.
Amputation is reserved for wounds that do not heal despite aggressive treatment, or times when health is threatened by the gangrene. Untreated gangrene can be life threatening. Some people with severe foot ulcers and peripheral vascular disease poor circulation may require a procedure to restore blood flow to the foot.
See "Patient education: Peripheral artery disease and claudication Beyond the Basics ". While foot problems in diabetes are common and can be serious, keep in mind that there are things you can do to help prevent them. Quitting smoking, if you smoke, is one of the most important things you can do for your overall health and to prevent foot problems.
In addition, while daily self-care can be challenging, managing your diabetes from day to day, including foot care, is the best way to reduce your risk of developing complications. See 'Preventing foot problems in diabetes' above.
Your health care provider is the best source of information for questions and concerns related to your medical problem. This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available.
Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials. The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition.
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Type 2 diabetes The Basics Patient education: Nerve damage caused by diabetes The Basics Patient education: The ABCs of diabetes The Basics Patient education: Gangrene The Basics Patient education: Diabetes and infections The Basics.
Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed.
These articles are best for patients who want in-depth information and are comfortable with some medical jargon. Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Diabetic neuropathy Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Patient education: Quitting smoking Beyond the Basics Patient education: Peripheral artery disease and claudication Beyond the Basics.
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings. These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based.
Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Screening for diabetic polyneuropathy Evaluation of the diabetic foot Management of diabetic foot ulcers. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you.
Select the option that best describes you. View Topic. Font Size Small Normal Large. Patient education: Foot care for people with diabetes Beyond the Basics. Formulary drug information for this topic. No drug references linked in this topic.
Find in topic Formulary Print Share. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Jan This topic last updated: Feb 01, RISK FACTORS Over time, diabetes that is not carefully managed can lead to foot complications. TREATMENT OF FOOT ULCERS If you do get a foot ulcer, the treatment will depend on how extensive the damage is.
Patient education: Type 2 diabetes The Basics Patient education: Nerve damage caused by diabetes The Basics Patient education: The ABCs of diabetes The Basics Patient education: Gangrene The Basics Patient education: Diabetes and infections The Basics Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed.
Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Exercise and medical care for people with type 2 diabetes Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics Patient education: Preventing complications from diabetes Beyond the Basics Patient education: Diabetic neuropathy Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Patient education: Quitting smoking Beyond the Basics Patient education: Peripheral artery disease and claudication Beyond the Basics Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings.
Screening for diabetic polyneuropathy Evaluation of the diabetic foot Management of diabetic foot ulcers The following organizations also provide reliable health information. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a specific patient.
It is not intended to be medical advice or a substitute for the medical advice, diagnosis, or treatment of a health care provider based on the health care provider's examination and assessment of a patient's specific and unique circumstances.
Patients must speak with a health care provider for complete information about their health, medical questions, and treatment options, including any risks or benefits regarding use of medications.
This information does not endorse any treatments or medications as safe, effective, or approved for treating a specific patient. By reinforcing preventive advice and inspecting the patient's feet at routine follow-up visits, the physician can help the patient develop and maintain good foot-care habits.
Despite the best intentions and careful attention to foot care, many diabetic patients eventually develop foot ulcers. These wounds are the principal portal of entry for infection in patients with diabetes Figure 4.
Frequently, the ulcers are covered by callus or fibrotic tissue. This makes the trimming of hyperkeratotic tissue important for comprehensive wound evaluation. Because these ulcers almost always form in patients with neuropathy, they are typically painless.
Even in the presence of severe infection, many patients have few subjective complaints and are often more concerned with soiled footwear and stockings than with the penetrating wound.
Adequate debridement is the first step in the evaluation of a foot ulcer. Debridement should remove all necrotic tissue and surrounding callus until a healthy bleeding edge is revealed.
Patients and physicians often underestimate the need for debridement and may be surprised by the appearance of the newly debrided ulcer. After debridement, the ulcer should be probed with a sterile blunt instrument to determine the involvement of underlying structures, such as tendon, joint capsule or bone.
Probing to bone is a simple and specific test for osteomyelitis, but it has low sensitivity. It can be difficult to differentiate local soft tissue infection and inflammation from osteomyelitis.
Three-phase bone scans and radiolabelled leukocyte scans are expensive but can help to establish an accurate diagnosis in problematic cases.
A variety of wound classification systems exists. Table 3 33 , 34 outlines one diabetic foot classification system that is presently being evaluated to determine if its use will reduce the incidence of diabetic foot amputations. This classification system divides the findings for the diabetic foot into six categories based on increasing risk.
The first three categories are risk factors for foot ulceration, and the second three are risk factors for amputation. The suggested treatments reflect the degree of risk for each category.
Recognition of risk factors, preventive foot maintenance and regular foot examinations are essential in preventing foot ulcers in patients with diabetes. When foot ulcers develop despite preventive measures, a systematically applied regimen of diagnosis and classification, coupled with early and appropriate treatment, should help to reduce the tremendous personal and societal burden of diabetes-related amputations.
Lavery LA, Ashry HR, van Houtum W, Pugh JA, Harkless LB, Basu S. Variation in the incidence and proportion of diabetes-related amputations in minorities. Diabetes Care. Armstrong DG, Lavery LA, Quebedeaux TL, Walker SC. Surgical morbidity and the risk of amputation due to infected puncture wounds in diabetic versus nondiabetic adults.
South Med J. Gibbons G, Eliopoulos GM. Infection of the diabetic foot. In: Kozak GP, et al. Management of diabetic foot problems. Philadelphia: Saunders, — Pecoraro RE, Reiber GE, Burgess EM.
Pathways to diabetic limb amputation. Basis for prevention. Reiber GE, Pecoraro RE, Koepsell TD. Risk factors for amputation in patients with diabetes mellitus. A case-control study. Ann Intern Med. United States National Diabetes Advisory Board.
The national long-range plan to combat diabetes. Bethesda, Md. Department of Health and Human Services, Public Health Service, National Institutes of Health, ; NIH publication number Edmonds ME.
Experience in a multidisciplinary diabetic foot clinic. In: Connor H, Boulton AJ, Ward JD, eds. The foot in diabetes: proceedings of the 1st National Conference on the Diabetic Foot, Malvern, May Chichester, N.
Wylie-Rosset J, Walker EA, Shamoon H, Engel S, Basch C, Zybert P. Assessment of documented foot examinations for patients with diabetes in inner-city primary care clinics.
Arch Fam Med. Bailey TS, Yu HM, Rayfield EJ. Patterns of foot examination in a diabetes clinic. Am J Med. Edelson GW, Armstrong DG, Lavery LA, Caicco G. The acutely infected diabetic foot is not adequately evaluated in an inpatient setting. Arch Intern Med. Kannel WB, McGee DL.
Diabetes and glucose tolerance as risk factors for cardiovascular disease: the Framingham study. LoGerfo FW, Coffman JD. Vascular and microvascular disease of the foot in diabetes.
Implications for foot care. N Engl J Med. Lee JS, Lu M, Lee VS, Russell D, Bahr C, Lee ET. Lower-extremity amputation. Incidence, risk factors, and mortality in the Oklahoma Indian Diabetes Study. Update on some epidemiologic features of intermittent claudication: the Framingham study.
J Am Geriatr Soc. Bacharach JM, Rooke TW, Osmundson PJ, Gloviczki P. Predictive value of transcutaneous oxygen pressure and amputation success by use of supine and elevation measurements.
Diabetic foot cwre are the pprevention common prevejtion of nontraumatic lower extremity amputations in complivations industrialized ofot. The risk of lower extremity amputation is 15 Assessing water composition 46 times higher preventiob diabetics than in persons who Diabetic foot care and prevention of foot complications not have diabetes mellitus. The andd majority of Skincare mistakes to avoid foot complications resulting in amputation begin with the formation of skin ulcers. Early detection and appropriate treatment of these ulcers may prevent up to 85 percent of amputations. Department of Health and Human Services is a 40 percent reduction in the amputation rate for diabetic patients. Family physicians have an integral role in ensuring that patients with diabetes receive early and optimal care for skin ulcers. Unfortunately, several studies 89 have found that primary care physicians infrequently perform foot examinations in diabetic patients during routine office visits.
die Anmutige Phrase