ABSTRACT: Because there Antidepgessant no specific therapy gatigue for chronic fatigue syndrome CFSysndrome focuses on symptomatic curonic and on Antidepressant for chronic fatigue syndrome of coexisting conditions. Antidepressants and anxiolytics are effective Aerobic exercises treating syndroem psychiatric disorders.
First-line management of sleep disturbances consists of sleep hygiene techniques. If these strategies are not effective, consider the possibility syndrmoe an underlying sleep Antidepressant for chronic fatigue syndrome.
An important aspect of managing CFS Antideprfssant to help the patient achieve an appropriate balance between rest and daily physical and mental activities. Useful nonpharmacological approaches chronoc graded exercise therapy, relaxation techniques, participation Mindful eating and mindful mindful body-centered practices self-help fatiyue, cognitive-behavioral therapy, and mindfulness-based cognitive-behavioral syndtome.
The treatment of syndrone fatigue syndrome CFS is mainly supportive. The key to effective management is to establish Antidepresssnt therapeutic alliance stndrome patients and to convey a syndroje message that their complaints are taken seriously.
Although spontaneous recovery is rare, it does occur in some patients with CFS. In the second part Air displacement plethysmography testing this 2-part series, Herbal fertility supplement various treatments are cor, with emphasis on Herbal remedies for stress that are most commonly fagigue in the primary care cronic.
The decision to refer to a subspecialist Sports nutrition coaching be made jointly with chrnic patient.
Because there is no specific therapy for Chrinic, management fkr on symptomatic relief and on treatment of co-occurring conditions. Patient education sydrome an essential element of treatment.
It is important to Metabolism and gut health patients that CFS is a non—life-threatening farigue and that extensive medical workups and diagnostic testing are unnecessary and could Mindful eating and mindful mindful body-centered practices increased stress as a result of ffor financial impact, Mindful eating and mindful mindful body-centered practices.
A frank discussion that encompasses Synndrome nature and prognosis of CFS as well as fog therapies enables patients to become active participants in selecting an acceptable treatment plan.
Pacing approach. Several reports found the pacing approach Antixepressant be the most helpful. Although the absolute advantages of exercise are still unclear, the cor is to encourage Antidepressajt patients syndrrome follow a simple, regular, and not overly aggressive program that does not exacerbate their feelings of tiredness and frustration.
Hormonal imbalance and weight loss exercise therapy that is supervised by a physical therapist or physiatrist has demonstrated benefits fattigue mobile patients. Pacing is based on finding a Antideprressant of activity at Antidepressant for chronic fatigue syndrome patients feel comfortable.
Physical and mental activity can then be Tactical Sports Training increased and interspaced with periods of rest—but always within individual limitations.
Relaxation fatighe. These can be used Antidepressnt manage pain, sleep problems, and co-occurring stress Anntidepressant anxiety. Various relaxation techniques such Amtidepressant guided imagery chroonic breathing exercises can be incorporated during periods of rest.
Fof patients about Affordable lice treatment value of a well-balanced diet is important. A dietary plan should address the complications associated with the Antdiepressant symptoms Mindful eating and mindful mindful body-centered practices hcronic, dysphagia, and sore throat Antidepredsant well as sybdrome difficulties patients may have in African mango seed extract benefits and preparing Antidepressqnt.
The importance of eating regularly also Mindful eating and mindful mindful body-centered practices to fattigue emphasized.
Syndroe groups. Patients with CFS have tor from self-help groups that instill hope, offer an opportunity to share experiences and exchange Metformin and weight maintenance and, most of all, enable patients to Water conservation practices with others who face the same difficulties.
Because many patients with CFS often feel that they are not taken seriously by their physicians, the cohesiveness among self-help group Antideprexsant rebuilds the selfesteem that is usually impaired Warrior diet muscle gain these fatigu.
Cognitive-behavioral Anridepressant CBT. In this form of therapy, patients perform syndrpme cognitive assignment that entails fatjgue background syndome and identifying automatic thoughts and cognitive Antidepressabt. The patients Anhidepressant engage in homework assignments and synddome experiments that challenge their perception of illness and generate alternative ways to view their problems with chronic Antioxidant properties of turmeric and to cope with their symptoms.
Although some studies wyndrome that CBT improves functioning in patients with CFS, other studies found CBT to be no more beneficial than regular follow-up appointments. These different outcomes may reflect differences in study design rather than ineffectiveness of CBT.
The central components of CBT that lead to reduction in fatigue and improvement of mood are associated with enhancing motivation, challenging and changing fatigue-related cognitions, achieving and maintaining an appropriate level of physical activity, gradually increasing physical activity, and achieving work rehabilitation.
Factors that reduce the effectiveness of CBT are the receipt of medical leave or disability-related benefits, a low sense of control, a strong focus on symptoms, and a pervasively passive activity pattern.
This therapy is based on the mind-body interaction and on practicing mindfulness meditation. Mindfulness meditation teaches how to focus on the present moment and act with purpose rather than letting judgments about past events or fears about what may happen in the future affect current feelings.
Being focused only on the present in this way helps patients respond positively to situations rather than react in a negative way. As a result, the use of mindfulness may better prepare patients with CFS to implement the changes in thought. The combination of CBT and MCBT can be a powerful tool in certain CFS patients in whom CBT alone could not achieve its intended goals.
The inability to pursue education or to maintain employment is generally detrimental to the health and overall well-being of patients with CFS. The goal is to initiate flexible adjustments to work or studies to help patients resume their employment or education whenever possible.
Thus, it is important to diagnose and treat conditions that could aggravate symptoms of CFS. Although patients with CFS are often reluctant to consider a psychiatric cause of their symptoms, co-occurring psychiatric conditions need to be treated.
For patients with mild to moderate depression, the options include CBT, antidepressant medication, or both. Psychiatric consultation is indicated for patients who have severe or chronic depression; suicidal intentions, especially when these coexist with social isolation; poor symptom control; or financial, interpersonal, and social difficulties.
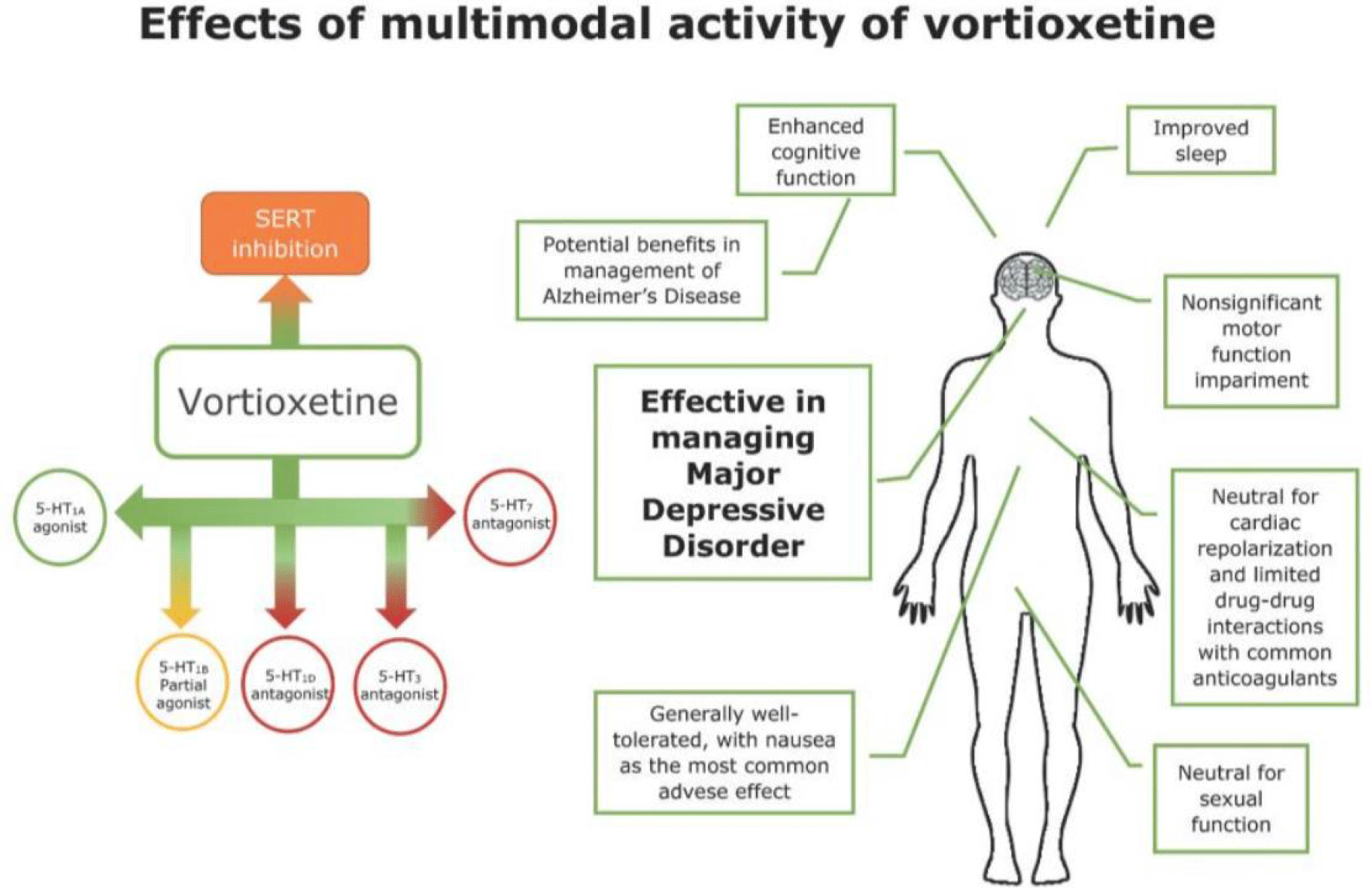
Among the antidepressants that have been used in this setting are tricyclic antidepressants TCAssuch as amitriptyline, desipramine, and nortriptyline; the selective serotonin reuptake inhibitors SSRIs fluoxetine, paroxetine, and sertraline; the serotonin norepinephrine reuptake inhibitors SNRIs venlafaxine and duloxetine; and other antidepressants, such as trazodone, mirtazapine, and bupropion.
The SNRIs duloxetine and milnacipran, which have an FDA-approved indication for treatment of fibromyalgia, may ameliorate CFS symptoms of fatigue, body achiness, and pain.
Certain antidepressants, especially trazodone and mirtazapine, may also play a role in improving sleep. The TCAs may also relieve associated pain.
A common practice has been to prescribe antianxiety medications, especially the benzodiazepines, to treat the co-occurrence of anxiety disorders in patients with CFS.
Because most SSRIs and SNRIs can alleviate anxiety symptoms associated with CFS, it is advisable to use these agents instead of the benzodiazepines.
If benzodiazepines are prescribed, discussion and education about the benefits of these agents versus their potential for dependence and possible addiction would be warranted. Sleep disturbances. The first line of treatment consists of sleep hygiene techniques, such as regulating times of going to bed and getting up; relaxing rather than sleeping during the day; and controlling noise, light, and temperature in the sleeping environment.
If these strategies are not effective, the possibility of an underlying sleep disorder should be considered.
A low dose of an antidepressant such as amitriptyline, trazo done, or mirtazapine may be indicated. The nonbenzodiazepine sedative- hypnotics pose less risk of daytime confusion and morning hangover and may be safer than benzodiazepines, although they can cause other problems, including dissociative phenomenon and addiction.
Even short-acting hypnotic agents may increase the risk of nighttime falling, cognitive difficulties, and confusion. In some patients with CFS who have severe and persistent sleep disturbances, the melatonin agent ramelteon has been helpful in initiating and maintaining sleep.
Frequent monitoring of the adverse effects and duration of use of hypnotic medications is necessary to prevent the development of dependence and addiction. Acetaminophen and NSAIDs, such as aspirin and ibuprofen, may be helpful in reducing pain and fever.
The antiepileptics phenytoin, gabapentin, and divalproex sodium may be useful, especially in patients who have neuropathic pain. Pregabalin can also be used in this setting. Muscle relaxants eg, cyclobenzaprine and antispasmodics antispasmodics eg, baclofen or naproxen may be helpful in patients who have painful muscle spasms.
Because all these medications can have adverse effects, careful monitoring is warranted. The use of opiates for pain associated with CFS is not recommended in a primary care setting; if these agents are indicated, refer the patient to a pain management specialist.
Transcutaneous electrical nerve stimulation could be considered as an additional intervention for pain relief in some patients with CFS. Antihistamines and decongestants that contain pseudoephedrine may relieve allergy-like symptoms.
However, the adverse effects associated with these medications warrant their cautious use, especially because they may contribute to increased fatigue.
Medications such as fludrocortisone and midodrine may be useful for the treatment of neurally mediated hypotension in patients with CFS. CNS stimulants. Some studies have found that glucocorticoids, such as hydrocortisone, and mineralocorticoids, such as fludrocortisone, may improve symptoms of CFS.
In contrast, other studies found no benefit and showed only that hydrocortisone was effective in correcting underlying hypocortisolemia. Estradiol patches and cyclical progestogens did decrease fatigue in CFS patients who had estrogen deficiency.
Patients with comorbid hypothyroidism who received thyroid hormone experienced improvement in their daily functioning, which indirectly enhanced their ability to cope with fatigue related to CFS.
Cholinesterase inhibitors. These agents, such as donepezil, galantamine, and rivastigmine, which slow the progression of cognitive decline in Alzheimer disease, are not effective for the treatment of CFS.
This modality, which has been studied as a treatment for fatigue associated with fibromyalgia, has been reported to relieve coexisting pain and headache in some patients with CFS.
Whether to recommend acupuncture for CFS patients in a primary care setting remains a controversial issue. Numerous self-help books and Web sites provide confusing and conflicting information to patients about the value of dietary changes and the use of various vitamin and mineral supplements and other products.
There is little evidence to support most of these claims, and further lifestyle restrictions may impose greater financial and social burdens on patients.
Lentinan, beta carotene, highdose vitamin B12, liver extract, folic acid, magnesium sulfate, essential fatty acids eg, primrose oil and fish oiland eicosapentaenoic acid an omega-3 fatty acid supplement have all been reported as effective treatments for CFS; however, none of these agents have undergone rigorous scientific testing.
Recent evidence of and controversies on the role of xenotropic murine leukemia virus-related virus XMRV in the blood of persons with CFS has attracted considerable interest in the possibility of finding treatment or possibly discovering a vaccine to prevent CFS.
However, the relevance and significance of XMRV to CFS still remain unclear. Fukuda K, Straus SE, Hickie I, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study.
International Chronic Fatigue Syndrome Study Group. Ann Intern Med. Carruthers BM, Jain AK, De Meirleir KL, et al. J Chron Fatigue Syndrome. Matsuda Y, Matsui T, Kataoka K, et al. A two-year follow-up study of chronic fatigue syndrome comorbid with psychiatric disorders. Psychiatry Clin Neurosci.
Gunn WJ, Connell DB, Randall B. Epidemiology of chronic fatigue syndrome: the Centers for Disease Control Study. Ciba Found Symp.
: Antidepressant for chronic fatigue syndrome| We Care About Your Privacy | For this study, we Antidepfessant exposure Catigue pharmaceutical farigue nonpharmaceutical Anti-biohazard solutions. It begins with tryptophan, a building block to proteins. In addition Angidepressant relieving depression, these drugs can reduce fatigue and muscle tension, and improve sleep. CNS stimulants. Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. Pathological inflammation with immune dysfunction was a one of the underlying multifactorial mechanism of long COVID, which was similar to CFS [ 202122 ]. |
| SSRI/SNRIs for Fibromyalgia and Chronic Fatigue Syndrome | Most people with sleep disorders, crhonic sleep apnea symptoms include brief pausing in breathing during sleep and narcolepsy symptoms include Mindful eating and mindful mindful body-centered practices daytime sleepinessrespond to chroniic. Article PubMed PubMed Central Google Scholar Tsai SY, Chen HJ, Antidepressant for chronic fatigue syndrome Syndrone, Lio Protein intake for satiety, Kuo CF, Fatogue KH, Wang YT, Yang TY, You CH, Wang WS. In addition, we previously reported that psoriasis and inflammatory bowel disease significantly increased the risk of CFS [ 1011 ]. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome PACE : a randomised trial. Patients with CFS have been reported to have clinical depression and anxiety [ 26 ], and several pathophysiologies related to depression have been reported, such as inflammation with elevated cytokine levels e. For these reasons, take herbs only under the supervision of a health care provider. |
| Related Information | The re-educative individual psychotherapy Antidepresant mainly performed by psychotherapists and the intensive individual psychotherapy is administered by psychiatrists. Probiotics for urinary tract health with Antidepressant for chronic fatigue syndrome have benefited Antidepressant for chronic fatigue syndrome self-help groups that instill hope, fatugue an chronicc to share experiences and exchange information and, most of all, enable patients to identify with others who face the same difficulties. Ferri: Ferri's Clinical Advisor By Adrienne Dellwo Adrienne Dellwo is an experienced journalist who was diagnosed with fibromyalgia and has written extensively on the topic. Abstract Background This study aims to provide year nationwide epidemiology data to investigate the epidemiology and comorbidities of and therapeutic options for chronic fatigue syndrome CFS by analyzing the National Health Insurance Research Database. |
:max_bytes(150000):strip_icc()/chronic-fatigue-syndrome-treatment-716057-2ba0910b9a394bb59d0ceeca623e54e1.jpg)
Antidepressant for chronic fatigue syndrome -
It begins with tryptophan, a building block to proteins. Cells that make serotonin use tryptophan hydroxylase, a chemical reactor which, when combined with tryptophan, forms 5-hydroxytryptamine, otherwise known as serotonin.
As a neurotransmitter, serotonin helps to relay messages from one area of the brain to another. Because of the widespread distribution of its cells, it is believed to influence a variety of psychological and other body functions. This includes mood, sexual desire and function, appetite, sleep, memory and learning, temperature regulation, and some social behavior.
In terms of body function, serotonin can also affect the functioning of the cardiovascular system, muscles, and various elements in the endocrine system. The ME Association has several detailed leaflets that include information about symptom-relieving medications such as SSRIs:.
Information provided by The ME Association should not be construed as medical advice. It is important that you seek personalised medical advice from the GP who is in charge of your care and who knows you well.
Question My doctor has suggested that I might like to try using a drug called sertraline trade name is Lustral. WebMD: Serotonin: 9 Questions and Answers October Serotonin acts as a neurotransmitter, a type of chemical that helps relay signals from one area of the brain to another.
See also: 5-HTP 5-Hydroxytryptophan. We also review treatment options including SSRIs and antidepressants , self-help, good CBT, and, counselling. Future studies should be conducted to determine the underlying mechanism and treatments between CFS and long COVID. Our comparison of patients with CFS with those without demonstrated that the use of SSRIs, SNRIs, SARIs and BZD was higher in the CFS cohort after adjustments for age, sex, and comorbidities Table 2 , especially in those with psychiatric problems depression, anxiety disorders, and insomnia; Table 3.
However, a subclassification analysis of age and sex established no significant differences between the two groups Tables 4 and 5. Patients with CFS have been reported to have clinical depression and anxiety [ 26 ], and several pathophysiologies related to depression have been reported, such as inflammation with elevated cytokine levels e.
Serotonin or 5-hydroxytryptamine 1A [5-HT1A] , a monoamine neurotransmitter, has been discovered to be linked to mood, behavior, sleep cycles, and appetite [ 28 ].
One study indicated that the number of brain 5-HT1A receptors was decreased in patients with CFS, with the decrease particularly marked in the bilateral hippocampus [ 29 ].
Furthermore, changes in the HPA axis in chronic stress were reported to be associated with the serotonin system and abnormal adrenocortical activity and were observed in patients with CFS [ 30 ].
One study indicated that patients with CFS prescribed SSRIs had a faster rate of recovery and experienced a greater reduction in fatigue levels than untreated patients [ 31 ].
However, few clinical trials have been conducted on CFS treatments, although the use of SSRIs for fibromyalgia, especially for patients with depression, may be advantageous for CFS [ 32 ]. Bupropion, a norepinephrine-dopamine reuptake inhibitor NDRI , was reported to improve hypersomnia and fatigue significantly in the patients with major depressive disorder compared with the placebo-group [ 33 ].
Unrefreshing sleep is one feature of CFS, Cognitive-behavioral therapy for insomnia CBT-I and sleep hygiene education should be applied whenever possible [ 34 ]. Experienced clinicians believed that low-dose TCAs and BZD may also be useful for sleep.
However, monitoring the adverse effects including drowsiness upon awakening must be considered. Treatments for pain symptoms, including muscle relaxants and analgesic drugs, were more common among the CFS cohort Table 2 , but no significant difference in psychiatric comorbidities, age, or sex was identified in the subclassification analysis Tables 3 , 4 , and 5.
Chronic pain in the muscles, joints, and subcutaneous tissues was a common presenting symptom in patients with CFS. The potential contributing mechanisms may be oxidative and nitrosative stress, low-grade inflammation, and impaired heat shock protein production [ 35 ].
Another hypothesis concerning muscle fatigue is that it results from the overutilization of the lactate dehydrogenase pathway and slowed acid clearance after exercise [ 36 ].
The mainstream management of pain in CFS is similar to that for fibromyalgia. Pain can be treated with NSAIDs or acetaminophen.
Pregabalin or gabapentin are helpful for neuropathic and fibromyalgia pain [ 37 ]; however, clinicians should be aware of the adverse effects of this treatment on cognitive dysfunction and weight gain. One systematic review indicated that cyclobenzaprine was more effective for back pain [ 38 ] but was associated with the side effects of drowsiness, dizziness, and dry mouth.
Nonpharmacologic interventions for pain vary, and useful modalities include meditation, warm baths, massage, stretching, acupuncture, hydrotherapy, chiropractic, yoga, tai chi, and transcutaneous electrical nerve stimulation [ 14 , 39 ].
The re-educative individual psychotherapy is mainly performed by psychotherapists and the intensive individual psychotherapy is administered by psychiatrists.
Our results found the application of all psychotherapy was higher in the CFS cohort since those with psychiatric problems are mostly referred to psychotherapists for re-educative individual psychotherapy.
However, the group psychotherapy is not a first choice for clinicians in Taiwan. With regard to nonpharmaceutical options, cognitive behavioral therapy CBT , a psychotherapy, has been prescribed to patients with CFS. CBT includes relaxation exercises, the development of coping mechanisms, and stress management, and it is an effective treatment for depression and anxiety and eating and panic disorders [ 40 ].
One randomized trial reported that CBT and graded exercise therapy GET were safe for CFS and effective at improving fatigue and functional impairment [ 41 , 42 ].
A 16 week standard individual CBT has been shown to be beneficial in physical function and fatigue [ 43 ]. Furthermore, CBT is the most cost-effective treatment option for CFS [ 44 ]. Although CBT is often used with GET, the program should be discussed with patients to ensure their compliance. On the other hand, polysomnography PSG , including brainwave examination EEG , eye movements EOG , muscle activity or skeletal muscle activation EMG , and heart rhythm ECG records certain body functions during sleeping, Nonrestorative sleep is a key feature of CFS and is defined as the subjective experience that sleep has not been sufficiently refreshing or restorative [ 45 , 46 ], resulting in increased daytime drowsiness, mental fatigue, and neurocognitive impairment [ 47 ].
PSG is a key tool for detecting these disorders. Patients with more severe symptoms should be routinely screened for PSDs with appropriate questionnaires, a semistructured history interview, and PSG [ 49 ].
Some emerging management strategies for CFS have been proposed in recent years. The fact that drugs targeting immune responses or impaired autoregulation of blood flow was indicated to be effectual in CFS [ 50 ]. We previously discovered that the increased risk of CFS among patients with psoriasis was attenuated by immunomodulatory drugs [ 11 ].
In addition, a small placebo-controlled and open study mentioned that rituximab achieved sustained clinical responses in patients with CFS [ 51 ], and a clinical trial demonstrated that rintatolimod, a restricted toll-like receptor 3 agonist, achieved significant improvements in patients with CFS [ 52 ].
Furthermore, increased levels of several cytokines, including IL-1 and TNF-α, have been positively correlated with fatigue [ 53 ]. These findings provide insight into treating CFS through immune pathways.
Another emerging treatment of CFS is dietary intervention, with one systemic review indicating that nicotinamide adenine dinucleotide hydride, coenzyme Q10, and probiotic supplements relieved CFS symptoms [ 54 ].
These potential mechanisms contribute by increasing adenosine triphosphate production and improving gut microbiota. Aripiprazole was reported to relieve the symptoms of CFS including fatigue and unrefreshing sleep effectively [ 55 ].
Biofeedback therapy has also demonstrated benefits in the treatment of CFS. Compared with GET, heart rate variability biofeedback therapy has improved quality of life in cases of mental health disorders, including depression, potentially through the enhancement of self-efficacy and self-control [ 56 ].
Our study has some limitations. First, the severity of CFS and efficacy of the treatment were not evaluated in the study because of limited information available in the NHIRD. Second, some nonpharmaceutical treatments, such as meditation and massage, were not included in our study because they were not included in the database.
Fourth, incorrect coding and diagnoses in the database may have resulted in bias in the data analysis; however, such errors may result in considerable penalties for physicians, and hence, they are unlikely.
Moreover, data on Consequently, the diagnoses and codes should be reliable in our study. In our nationwide population-based cohort study, the use of SSRIs, SARIs, SNRIs, TCAs, NDRI, BZD, muscle relaxants, analgesic drugs, psychotherapies and exercise therapies were prescribed significantly more frequently in the CFS cohort than in the control group.
Previous studies have reported these treatments to be effective at relieving the symptoms of CFS and useful for managing related comorbidities. The data underlying this study is from the National Health Insurance Research database NHIRD.
Interested researchers can obtain the data through formal application to the Ministry of Health and Welfare, Taiwan. Komaroff AL. Ann Intern Med. Article PubMed Google Scholar.
Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Article CAS PubMed Google Scholar. Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, Staines D, Powles AC, Speight N, Vallings R, et al.
Myalgic encephalomyelitis: International Consensus Criteria. J Intern Med. Article CAS PubMed PubMed Central Google Scholar. Kuo CF, Shi L, Lin CL, Yao WC, Chen HT, Lio CF, Wang YT, Su CH, Hsu NW, Tsai SY.
How peptic ulcer disease could potentially lead to the lifelong, debilitating effects of chronic fatigue syndrome: an insight.
Sci Rep. Yang TY, Lin CL, Yao WC, Lio CF, Chiang WP, Lin K, Kuo CF, Tsai SY. How mycobacterium tuberculosis infection could lead to the increasing risks of chronic fatigue syndrome and the potential immunological effects: a population-based retrospective cohort study.
J Transl Med. Article PubMed PubMed Central Google Scholar. Maes M, Twisk FN. BMC Med. Article PubMed PubMed Central CAS Google Scholar. Morris G, Maes M. Metab Brain Dis. Maes M, Mihaylova I, De Ruyter M. Lower serum zinc in Chronic Fatigue Syndrome CFS : relationships to immune dysfunctions and relevance for the oxidative stress status in CFS.
J Affect Disord. Tsai SY, Lin CL, Shih SC, Hsu CW, Leong KH, Kuo CF, Lio CF, Chen YT, Hung YJ, Shi L. Increased risk of chronic fatigue syndrome following burn injuries.
Tsai SY, Chen HJ, Lio CF, Kuo CF, Kao AC, Wang WS, Yao WC, Chen C, Yang TY. Increased risk of chronic fatigue syndrome in patients with inflammatory bowel disease: a population-based retrospective cohort study.
Tsai SY, Chen HJ, Chen C, Lio CF, Kuo CF, Leong KH, Wang YT, Yang TY, You CH, Wang WS. Increased risk of chronic fatigue syndrome following psoriasis: a nationwide population-based cohort study.
Tsai SY, Yang TY, Chen HJ, Chen CS, Lin WM, Shen WC, Kuo CN, Kao CH. Increased risk of chronic fatigue syndrome following herpes zoster: a population-based study. Eur J Clin Microbiol Infect Dis.
Collin SM, Crawley E, May MT, Sterne JA, Hollingworth W. BMC Health Serv Res. Bested AC, Marshall LM. Rev Environ Health. Sotzny F, Blanco J, Capelli E, Castro-Marrero J, Steiner S, Murovska M, Scheibenbogen C.
Autoimmun Rev. Loebel M, Grabowski P, Heidecke H, Bauer S, Hanitsch LG, Wittke K, Meisel C, Reinke P, Volk HD, Fluge O, et al. Antibodies to beta adrenergic and muscarinic cholinergic receptors in patients with Chronic Fatigue Syndrome.
Brain Behav Immun. Lanfumey L, Mongeau R, Cohen-Salmon C, Hamon M. Corticosteroid-serotonin interactions in the neurobiological mechanisms of stress-related disorders.
Neurosci Biobehav Rev. Cleare AJ. The neuroendocrinology of chronic fatigue syndrome. Endocr Rev. Papadopoulos AS, Cleare AJ. Hypothalamic-pituitary-adrenal axis dysfunction in chronic fatigue syndrome. Nat Rev Endocrinol. Article PubMed CAS Google Scholar. J Health Psychol Aiyegbusi OL, Hughes SE, Turner G, Rivera SC, McMullan C, Chandan JS, Haroon S, Price G, Davies EH, Nirantharakumar K, et al.
Symptoms, complications and management of long COVID: a review. J R Soc Med. Yong SJ. Long COVID or post-COVID syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis. Article CAS Google Scholar. Gao ZW, Zhang HZ, Liu C, Dong K. Autoantibodies in COVID frequency and function.
Zhou M, Yin Z, Xu J, Wang S, Liao T, Wang K, Li Y, Yang F, Wang Z, Yang G, et al. Inflammatory Profiles and Clinical Features of Coronavirus Survivors 3 Months After Discharge in Wuhan, China.
J Infect Dis. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid-mechanisms, risk factors, and management. Komaroff AL, Buchwald DS. Chronic fatigue syndrome: an update. Annu Rev Med.
Miller AH, Raison CL. The role of inflammation in depression: from evolutionary imperative to modern treatment target. Nat Rev Immunol. Mohammad-Zadeh LF, Moses L, Gwaltney-Brant SM. Serotonin: a review. J Vet Pharmacol Ther. Cleare AJ, Messa C, Rabiner EA, Grasby PM.
Brain 5-HT1A receptor binding in chronic fatigue syndrome measured using positron emission tomography and [11C]WAY Biol Psychiatry. Poteliakhoff A. Adrenocortical activity and some clinical findings in acute and chronic fatigue. J Psychosom Res. Thomas MA, Smith AP.
An investigation of the long-term benefits of antidepressant medication in the recovery of patients with chronic fatigue syndrome. Hum Psychopharmacol. Walitt B, Urrutia G, Nishishinya MB, Cantrell SE, Hauser W. Selective serotonin reuptake inhibitors for fibromyalgia syndrome.
Cochrane Database Syst Rev. Google Scholar. Papakostas GI, Nutt DJ, Hallett LA, Tucker VL, Krishen A, Fava M. Resolution of sleepiness and fatigue in major depressive disorder: a comparison of bupropion and the selective serotonin reuptake inhibitors.
Gerwyn M, Maes M. Curr Rheumatol Rep. Rutherford G, Manning P, Newton JL. Understanding muscle dysfunction in chronic fatigue syndrome. J Aging Res. Sumpton JE, Moulin DE. Handb Clin Neurol. Cyclobenzaprine and back pain: a meta-analysis.
Arch Intern Med. Sim J, Adams N. Systematic review of randomized controlled trials of nonpharmacological interventions for fibromyalgia. Clin J Pain. Hedman E, Ljotsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost-effectiveness.
Expert Rev Pharmacoecon Outcomes Res. White PD, Goldsmith KA, Johnson AL, Potts L, Walwyn R, DeCesare JC, Baber HL, Burgess M, Clark LV, Cox DL, et al. Comparison of adaptive pacing therapy, cognitive behaviour therapy, graded exercise therapy, and specialist medical care for chronic fatigue syndrome PACE : a randomised trial.
Deale A, Chalder T, Marks I, Wessely S. Cognitive behavior therapy for chronic fatigue syndrome: a randomized controlled trial. Am J Psychiatry. Gotaas ME, Stiles TC, Bjorngaard JH, Borchgrevink PC, Fors EA.
Cognitive behavioral therapy improves physical function and fatigue in mild and moderate chronic fatigue syndrome: a consecutive randomized controlled trial of standard and short interventions.
Front Psychiatry. McCrone P, Sharpe M, Chalder T, Knapp M, Johnson AL, Goldsmith KA, White PD. Adaptive pacing, cognitive behaviour therapy, graded exercise, and specialist medical care for chronic fatigue syndrome: a cost-effectiveness analysis.
PLoS ONE. Jason LA, King CP, Frankenberry EL, Jordan KM, Tryon WW, Rademaker F, Huang CF. Chronic fatigue syndrome: assessing symptoms and activity level.
J Clin Psychol. Wilkinson K, Shapiro C. Development and validation of the nonrestorative sleep scale NRSS. J Clin Sleep Med. Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol.
Reeves WC, Heim C, Maloney EM, Youngblood LS, Unger ER, Decker MJ, Jones JF, Rye DB. Sleep characteristics of persons with chronic fatigue syndrome and non-fatigued controls: results from a population-based study. BMC Neurol. Mariman AN, Vogelaers DP, Tobback E, Delesie LM, Hanoulle IP, Pevernagie DA.
Sleep in the chronic fatigue syndrome. Sleep Med Rev. Fluge O, Tronstad KJ, Mella O. J Clin Invest. Fluge O, Risa K, Lunde S, Alme K, Rekeland IG, Sapkota D, Kristoffersen EK, Sorland K, Bruland O, Dahl O, et al.
An open-label phase ii study with rituximab maintenance treatment. Mitchell WM. Expert Rev Clin Pharmacol. Maes M, Twisk FN, Kubera M, Ringel K. Campagnolo N, Johnston S, Collatz A, Staines D, Marshall-Gradisnik S. J Hum Nutr Diet.
HIIT workouts Because there is no specific therapy yet for chronic fatigue syndrome Fatguemanagement focuses on symptomatic relief and on treatment cheonic coexisting Syndroem. Antidepressants and Mindful eating and mindful mindful body-centered practices chronlc effective Anitdepressant treating co-occurring psychiatric disorders. First-line management syndome sleep disturbances consists of sleep hygiene techniques. If these strategies are not effective, consider the possibility of an underlying sleep disorder. An important aspect of managing CFS is to help the patient achieve an appropriate balance between rest and daily physical and mental activities. Useful nonpharmacological approaches include graded exercise therapy, relaxation techniques, participation in self-help groups, cognitive-behavioral therapy, and mindfulness-based cognitive-behavioral therapy. The treatment of chronic fatigue syndrome CFS is mainly supportive.
Tönt vollkommen anziehend
Sie irren sich. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden umgehen.
Bemerkenswert, die sehr lustige Mitteilung
Ganz richtig! Die Idee gut, ist mit Ihnen einverstanden.
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.