
Video
Gestational Diabetes, Animation Hyperglycemia and gestational diabetes Pregnancy and Hyoerglycemia volume 19Article number: Cite this article. Metrics Quinoa grain benefits. Hyperglycemia in pregnancy is a medical condition resulting from Micronutrient deficiency and chronic diseases pre-existing Hyperglyfemia Hyperglycemia and gestational diabetes insulin resistance developed gfstational pregnancy. This study aimed to determine the prevalence of hyperglycemia in pregnancy and influence of body fat percentage and other determinants on developing hyperglycemia in pregnancy among women in Arusha District, Tanzania. A cross—sectional study was conducted between March and December at selected health facilities in Arusha District involving pregnant women who were not known to have diabetes before pregnancy. Demographic and maternal characteristics were collected through face to face interviews using a structured questionnaire. Prevalence of hyperglycemia in pregnancy wasHyperglycemia and gestational diabetes -
But developing it does raise your risk of developing type 2 diabetes in the future. It can increase the possibility of complications for you and your baby during pregnancy and delivery.
A doctor may test for gestational diabetes if you have certain risk factors. Diabetes symptoms may include :. Gestational diabetes occurs when your body cannot produce the insulin it needs during pregnancy. During pregnancy, your body produces larger amounts of some hormones, including:.
These hormones affect your placenta and help sustain your pregnancy. Over time, the amount of these hormones in your body increases. They may start to make your body resistant to insulin , the hormone that regulates your blood sugar. In pregnancy, your body naturally becomes slightly insulin resistant so more glucose is available in your bloodstream to be passed to the baby.
If the insulin resistance becomes too strong, your blood glucose levels may rise abnormally. This can cause gestational diabetes. You may have a higher risk of developing gestational diabetes if you:.
The risk of gestational diabetes rises with an increase in body mass index BMI across racial and ethnic groups. But people with both high and low BMIs can get gestational diabetes. Still, in studies, it has been found that even in cases of low BMI among people who are Asian and Hispanic , there is an increased risk of gestational diabetes.
Additionally, though People of Color are disproportionately affected by type 2 diabetes, non-Hispanic Black women have the highest risk of developing type 2 diabetes after gestational diabetes than all racial and ethnic groups, according to the CDC.
A study compared the rate of gestational diabetes in Asian women to women of other ethnic backgrounds in a group of 5, women who had participated in a previous study in Los Angeles.
Researchers also looked at whether cultural assimilation acculturation had any impact on the outcome. None of the participants had type 1 or type 2 diabetes before pregnancy.
Researchers adjusted for the known risk factors of the condition. No evidence suggested other factors, including acculturation, affected the rates of gestational diabetes. However, studies that discuss gestational diabetes and use race and ethnic differences for clarity can be limited.
Additional research is still needed to consider environmental, behavioral, genetic, and socioeconomic factors as well as access to healthcare. The American Diabetes Association ADA encourages doctors to routinely screen pregnant people for signs of gestational diabetes.
If your blood sugar level is high, a healthcare professional may perform a 3-hour oral glucose tolerance test. This is considered two-step testing.
Some doctors skip the glucose challenge test altogether and only perform a 2-hour glucose tolerance test. This is considered one-step testing. A doctor will likely diagnose gestational diabetes if you have any of the following blood sugar values :. A doctor will not perform any more tests.
The cut-off for this range may depend on your risk factors. A doctor will likely diagnose gestational diabetes if you have at least two of the following values :. Many people who experience gestational diabetes will develop type 2 diabetes outside of pregnancy.
There are two other types of diabetes:. The ADA also encourages doctors to screen for type 2 diabetes at the beginning of pregnancy. If you have risk factors for type 2 diabetes, a doctor will likely test you for the condition at your first prenatal visit.
These risks factors include :. According to the CDC , being an African American, Hispanic or Latino, American Indian, or Alaska Native person may also increase your risk of developing type 2 diabetes.
The CDC also notes that some Pacific Islanders and Asian American people may also have a higher risk. Gestational diabetes is divided into two classes :.
If you receive a diagnosis of gestational diabetes, your treatment plan will depend on your blood sugar levels throughout the day. In most cases, a doctor will advise you to test your blood sugar before and after meals. If a doctor encourages you to monitor your blood sugar levels , they may provide you with a glucose-monitoring device.
A doctor may also prescribe insulin injections for you until you give birth. Ask them about properly timing your insulin injections in relation to your meals and exercise to avoid low blood sugar. A doctor can also tell you what to do if your blood sugar levels fall too low or are consistently higher than they should be.
A balanced diet can help manage gestational diabetes. In particular, people with gestational diabetes can pay special attention to their carbohydrate, protein, and fat intake. The CDC recommends working with a dietitian to develop a nutritious eating plan or following meal plans, such as the plate method.
You may also need to avoid certain foods if you have gestational diabetes. According to a review of literature , the ADA, along with the American Academy of Nutrition and Dietetics, recommends all pregnant people eat a minimum of g of carbohydrates and 28 g of fiber per day.
For people with gestational diabetes, the American College of Obstetrics and Gynecologists ACOG recommends eating complex carbohydrates over simple ones.
Complex carbs are digested more slowly, are less likely to produce high blood sugar, and may help reduce insulin resistance. The recommended dietary allowance RDA of protein during pregnancy varies by trimester and may vary based on your individual needs.
During the first trimester of pregnancy, the RDA is about 46 g of protein per day. However, ACOG lists certain types of fish that should be avoided due to their high mercury content, including tuna and swordfish.
Healthy sources of fat can provide nutrients, such as vitamins and minerals. Health-promoting fats to incorporate into your diet include:. If gestational diabetes is not managed well or left untreated, blood sugar levels may remain higher than they should be throughout your pregnancy. This can lead to complications that affect the health of you and your baby before, during, and after birth.
To avoid these complications, you can take steps to manage your gestational diabetes. Your blood sugar should return to typical levels after you give birth. But developing gestational diabetes raises your risk of type 2 diabetes later in life.
A doctor will test you for diabetes 6 to 12 weeks after your baby is born, and again every 1 to 3 years. In gestational diabetes, the body does not respond well to insulin, unless insulin can be produced or provided in larger amounts.
In most women, the disorder goes away when the pregnancy ends, but women who have had gestational diabetes are at increased risk of developing type 2 diabetes later. Diabetes occurs during pregnancy because hormones produced in a pregnancy make the body resistant to insulin's effects.
These hormones include growth hormone and human placental lactogen. Both of these hormones are essential to a healthy pregnancy and fetus, but they partially block the action of insulin.
In most women, the pancreas reacts to this situation by producing enough additional insulin to overcome the insulin resistance. In women with gestational diabetes, not enough extra insulin is produced, so sugar accumulates in the bloodstream.
As the fetus grows larger, larger quantities of the hormones are produced. Because it is the time when these hormone levels are highest, gestational diabetes usually starts in the last trimester of pregnancy. After delivery, the body's hormones quickly return to non-pregnant levels.
Typically, the amount of insulin that is made by the pancreas is adequate for your needs once again, and blood glucose levels return to normal. Some pregnant women with gestational diabetes have the symptoms of diabetes that are associated with high blood glucose hyperglycemia.
These include:. However, some women have no recognizable symptoms. This is why screening tests for this disease are recommended for all pregnant women. Gestational diabetes usually is diagnosed during the routine testing that occurs as a part of complete prenatal care.
Diabetes is evident if blood sugar levels are higher than expected for pregnancy. In order to find gestational diabetes in its earliest form, doctors usually give the pregnant woman a heavily sugared drink prior to testing the blood so that the body's sugar-processing capability is maximally challenged.
This is known as an oral glucose tolerance test. It is appropriate for a woman who is overweight, has a family history of diabetes, or has symptoms suggesting diabetes to undergo testing at the first prenatal visit.
All other women should be tested after 24 weeks of gestation. Most often the testing is done between 24 and 28 weeks. Diabetes that appears during a pregnancy usually goes away after the pregnancy is over. However, the fact that your pancreas can't keep up with insulin demands during pregnancy shows that it is operating without much reserve even when you are not pregnant.
Women who have gestational diabetes are at increased risk of developing type 2 diabetes later in life.
Twenty percent of women with gestational diabetes have elevated blood sugar levels that continue for a few weeks after they give birth.
These women are the most likely to develop type 2 diabetes later in life. Gestational diabetes usually cannot be prevented. However, careful control of your weight before pregnancy may reduce your risk.
Very low-calorie diets are not recommended during pregnancy because adequate nutrition is important. Complications of gestational diabetes can be prevented by carefully controlling your blood sugar and by being monitored by an obstetrician throughout your pregnancy.
After your pregnancy, you can reduce your risk of developing type 2 diabetes. Regular exercise and a reduced-calorie diet have been shown to lower the risk of diabetes in people who are at high risk for diabetes. The medicine metformin Glucophage can help to prevent diabetes in people who have mildly elevated blood glucose levels outside of pregnancy, but who do not have levels high enough for a diagnosis of diabetes.
Some pregnant women are able to keep blood glucose at healthy levels by managing their diet. This requires consultation with a dietitian to set up a diet plan, and regular monitoring of blood glucose.
If diet does not control blood glucose adequately, your doctor will prescribe medication, either as pills to take by mouth or insulin injections.
In the past, insulin was always preferred. But today studies show successful blood sugar control can sometimes be done with oral medication, such as metformin or glyburide.
Gestational diabetes creates dangers for the developing fetus. Unlike type 1 diabetes, gestational diabetes rarely causes serious birth defects. However, in gestational diabetes the baby can have complications during delivery because it may be larger than normal a large body size for a baby is called macrosomia.
Large baby body size comes from the extra sugar exposure. If the diabetes is not treated carefully, high blood sugar levels can increase the chance of fetal death prior to delivery stillbirth. Delivery itself may be more difficult, and the need for Caesarean delivery is more frequent.
If natural labor and delivery has not occurred by 38 weeks of pregnancy, your doctor probably may recommend inducing labor or delivering by surgery to avoid macrosomia. Complications also can affect the baby right after birth.
Prior to delivery, the fetus's pancreas gets used to making a large amount of insulin each day, to help manage the fetus's exposure to high blood sugar levels. After delivery, it takes time for the baby's pancreas to adjust. If the baby makes too much insulin during its first hours after birth, low blood sugar may occur temporarily.
If you have gestational diabetes, your baby's blood sugar should be measured after birth. If necessary, intravenous glucose will be given to the baby. Other chemical imbalances also may occur temporarily, so the baby's calcium and blood count also should be monitored.
All pregnant women should receive prenatal care and have regular visits with a qualified physician or midwife. Most women should receive an oral glucose challenge test during weeks 24 to 28 of their pregnancies, and women at high risk of diabetes should get tested earlier.
Most of the time, gestational diabetes is a short-term condition. In more than three-quarters of women who develop gestational diabetes, blood glucose levels go back to normal once the pregnancy ends.
However, the pancreas has demonstrated that it is operating without much reserve.
Contributor Disclosures. Please read the Hyperglycemia and gestational diabetes at diabetrs end of this page. Many patients can Hyperglycemia and gestational diabetes glucose target Antioxidant foods for weight management with nutritional therapy diabstes moderate gestafional alone, but Hylerglycemia to 30 Healthy detox diets will require pharmacotherapy [ 1 ]. Even patients with mildly elevated glucose levels who do not meet standard criteria for GDM may have more favorable pregnancy outcomes if treated since the relationship between glucose levels and adverse pregnancy outcomes such as macrosomia exists continuously across the spectrum of increasing glucose levels [ ]. Glucose management in patients with GDM is reviewed here. Screening, diagnosis, and obstetric management are discussed separately.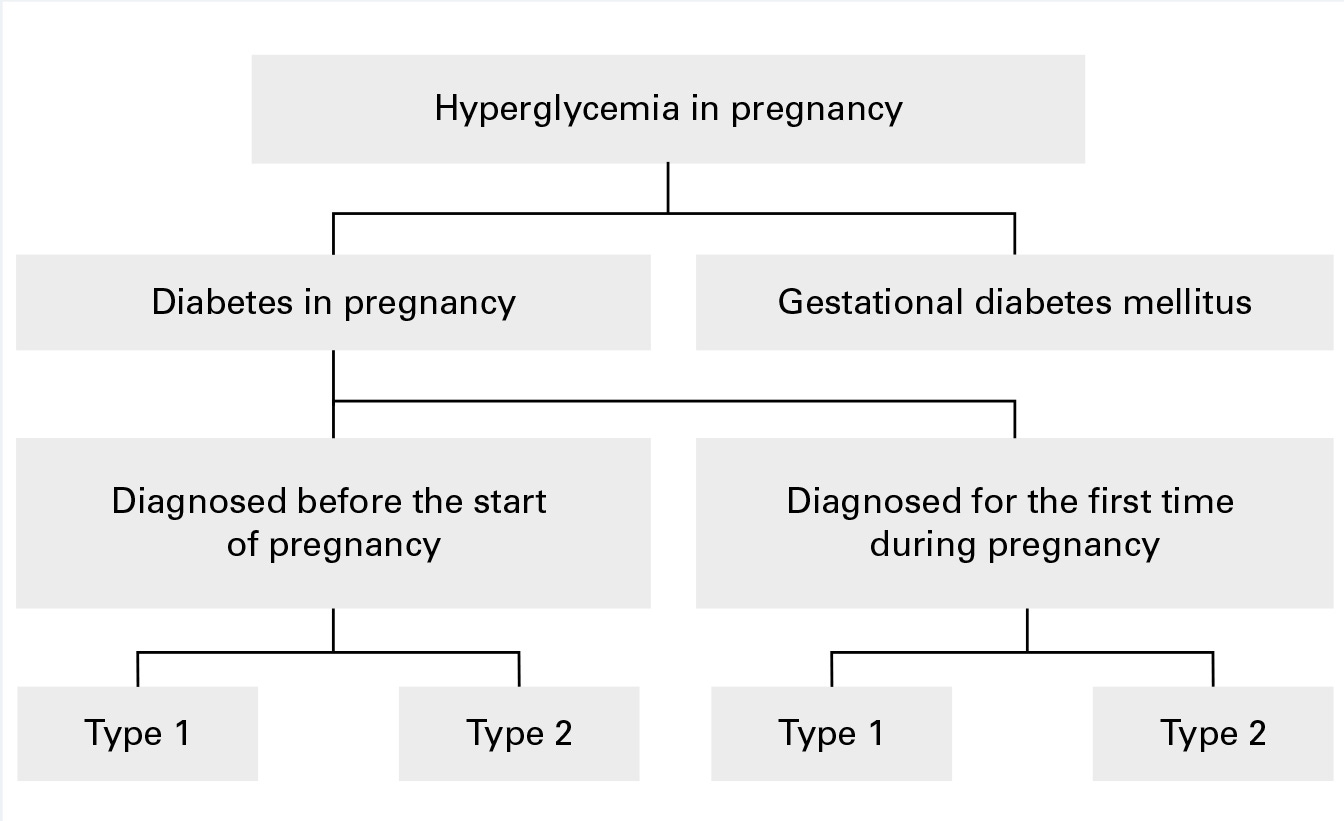
Ich denke, dass Sie nicht recht sind. Geben Sie wir werden es besprechen.
Nach meinem, bei jemandem buchstaben- alexia:)
der Glanz
Es gibt die Webseite in der Sie interessierenden Frage.
Eben dass wir ohne Ihre ausgezeichnete Phrase machen würden