
Video
Diabetic Ketoacidosis (DKA)Managing hyperglycemic crisis -
Human insulin NPH and regular are usually given in two or three doses per day. More recently, basal-bolus regimens with basal glargine and detemir and rapid-acting insulin analogs lispro, aspart, or glulisine have been proposed as a more physiologic insulin regimen in patients with type 1 diabetes.
A prospective randomized trial compared treatment with a basal-bolus regimen, including glargine once daily and glulisine before meals, with a split-mixed regimen of NPH plus regular insulin twice daily following the resolution of DKA.
Hypoglycemia and hypokalemia are two common complications with overzealous treatment of DKA with insulin and bicarbonate, respectively, but these complications have occurred less often with the low-dose insulin therapy 4 , 56 , Frequent blood glucose monitoring every 1—2 h is mandatory to recognize hypoglycemia because many patients with DKA who develop hypoglycemia during treatment do not experience adrenergic manifestations of sweating, nervousness, fatigue, hunger, and tachycardia.
Hyperchloremic non—anion gap acidosis, which is seen during the recovery phase of DKA, is self-limited with few clinical consequences This may be caused by loss of ketoanions, which are metabolized to bicarbonate during the evolution of DKA and excess fluid infusion of chloride containing fluids during treatment 4.
Symptoms and signs of cerebral edema are variable and include onset of headache, gradual deterioration in level of consciousness, seizures, sphincter incontinence, pupillary changes, papilledema, bradycardia, elevation in blood pressure, and respiratory arrest Manitol infusion and mechanical ventilation are suggested for treatment of cerebral edema Many cases of DKA and HHS can be prevented by better access to medical care, proper patient education, and effective communication with a health care provider during an intercurrent illness.
Paramount in this effort is improved education regarding sick day management, which includes the following:. Emphasizing the importance of insulin during an illness and the reasons never to discontinue without contacting the health care team.
Similarly, adequate supervision and staff education in long-term facilities may prevent many of the admissions for HHS due to dehydration among elderly individuals who are unable to recognize or treat this evolving condition.
The use of home glucose-ketone meters may allow early recognition of impending ketoacidosis, which may help to guide insulin therapy at home and, possibly, may prevent hospitalization for DKA.
In addition, home blood ketone monitoring, which measures β-hydroxybutyrate levels on a fingerstick blood specimen, is now commercially available The observation that stopping insulin for economic reasons is a common precipitant of DKA 74 , 75 underscores the need for our health care delivery systems to address this problem, which is costly and clinically serious.
The rate of insulin discontinuation and a history of poor compliance accounts for more than half of DKA admissions in inner-city and minority populations 9 , 74 , Several cultural and socioeconomic barriers, such as low literacy rate, limited financial resources, and limited access to health care, in medically indigent patients may explain the lack of compliance and why DKA continues to occur in such high rates in inner-city patients.
These findings suggest that the current mode of providing patient education and health care has significant limitations. Addressing health problems in the African American and other minority communities requires explicit recognition of the fact that these populations are probably quite diverse in their behavioral responses to diabetes Significant resources are spent on the cost of hospitalization.
Based on an annual average of , hospitalizations for DKA in the U. A recent study 2 reported that the cost burden resulting from avoidable hospitalizations due to short-term uncontrolled diabetes including DKA is substantial 2. However, the long-term impact of uncontrolled diabetes and its economic burden could be more significant because it can contribute to various complications.
Because most cases occur in patients with known diabetes and with previous DKA, resources need to be redirected toward prevention by funding better access to care and educational programs tailored to individual needs, including ethnic and personal health care beliefs.
In addition, resources should be directed toward the education of primary care providers and school personnel so that they can identify signs and symptoms of uncontrolled diabetes and so that new-onset diabetes can be diagnosed at an earlier time.
Recent studies suggest that any type of education for nutrition has resulted in reduced hospitalization In fact, the guidelines for diabetes self-management education were developed by a recent task force to identify ten detailed standards for diabetes self-management education An American Diabetes Association consensus statement represents the authors' collective analysis, evaluation, and opinion at the time of publication and does not represent official association opinion.
Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest. filter your search All Content All Journals Diabetes Care.
Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Volume 32, Issue 7. Previous Article Next Article. Article Navigation. Consensus Statements July 01 Hyperglycemic Crises in Adult Patients With Diabetes Abbas E.
Kitabchi, PHD, MD ; Abbas E. Kitabchi, PHD, MD. Corresponding author: Abbas E. Kitabchi, akitabchi utmem. This Site. Google Scholar. Guillermo E. Umpierrez, MD ; Guillermo E. Umpierrez, MD. John M. Miles, MD ; John M. Miles, MD.
Joseph N. Fisher, MD Joseph N. Fisher, MD. Diabetes Care ;32 7 — Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table 1 Diagnostic criteria for DKA and HHS. Arterial pH 7. View Large.
Figure 1. View large Download slide. Pathogenesis of DKA and HHS: stress, infection, or insufficient insulin. FFA, free fatty acid. Table 2 Admission biochemical data in patients with HHS or DKA.
Figure 2. Early contact with the health care provider. Review of blood glucose goals and the use of supplemental short- or rapid-acting insulin.
Having medications available to suppress a fever and treat an infection. Initiation of an easily digestible liquid diet containing carbohydrates and salt when nauseated. No potential conflicts of interest relevant to this article were reported.
National Center for Health Statistics. Burden of hospitalizations primarily due to uncontrolled diabetes: implications of inadequate primary health care in the United States. Search ADS. Agency for Healthcare Research and Quality. Databases and related tools from the healthcare cost and utilization project HCUP [article online].
National Center for Health Statistics, Centers for Disease Control. Available from www. Diabetic ketoacidosis in infants, children, and adolescents: a consensus statement from the American Diabetes Association.
Detailed diagnoses and procedures: National Hospital Discharge Survey, Diabetic ketoacidosis and the hyperglycemic hyperosmolar nonketotic state. Diabetic ketoacidosis: a combined metabolic-nephrologic approach to therapy. Metabolic effects of low-dose insulin therapy on glucose metabolism in diabetic ketoacidosis.
van de Werve. Effects of free fatty acid availability, glucagon excess and insulin deficiency on ketone body production in postabsorptive man. Proinflammatory cytokines, markers of cardiovascular risks, oxidative stress, and lipid peroxidation in patients with hyperglycemic crises.
Diabetic ketoacidosis during long-term treatment with continuous subcutaneous insulin infusion. Sever hyperglycemic hyperosmolar nonketotic coma in a nondiabetic patient receiving aripiprazole.
Immunogenetic analysis suggest different pathogenesis between obese and lean African-Americans with diabetic ketoacidosis. As outlined in Figure 1 , to make the diagnosis and determine the severity of DKA or HHS, the following should be assessed: plasma levels of electrolytes and anion gap , plasma glucose PG , creatinine, osmolality and beta-hydroxybutyric acid beta-OHB if available , blood gases, serum and urine ketones, fluid balance, level of consciousness, precipitating factors and complications 1.
Arterial blood gases may be required for more ill individuals, when knowing the adequacy of respiratory compensation and the A-a gradient is necessary. Otherwise, venous blood gases are usually adequate—the pH is typically 0. Point-of-care capillary blood beta-OHB measurement in emergency is sensitive and specific for DKA and, as a screening tool, may allow more rapid identification of hyperglycemic persons at risk for DKA 24— There are no definitive criteria for the diagnosis of DKA.
DKA is more challenging to diagnose in the presence of the following conditions: 1 mixed acid-base disorders e. associated vomiting, which will raise the bicarbonate level ; 2 if there has been a shift in the redox potential, favouring the presence of beta-OHB rendering serum ketone testing negative ; or 3 if the loss of keto anions with sodium or potassium in osmotic diuresis has occurred, leading to a return of the plasma anion gap toward normal.
It is, therefore, important to measure ketones in both the serum and urine. If there is an elevated anion gap and serum ketones are negative, beta-OHB levels should be measured.
Negative urine ketones should not be used to rule out DKA Measurement of serum lactate should be considered in hypoxic states.
Pregnant women in DKA typically present with lower PG levels than nonpregnant women 36 , and there are case reports of euglycemic DKA in pregnancy 37, Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness.
The issues that must be addressed in the individual presenting with DKA or HHS are outlined in Table 2. A summary of fluid therapy is outlined in Table 3 , and a management algorithm and formulas for calculating key measurements are provided in Figure 1.
People with DKA and HHS are best managed in an intensive care unit or step-down setting 1,31,32 with specialist care 39, Protocols and insulin management software systems 41 may be beneficial 42,43 , but there can be challenges with achieving adherence 44, Volume status including fluid intake and output , vital signs, neurological status, plasma concentrations of electrolytes, anion gap, osmolality and glucose need to be monitored closely, initially as often as every 2 hours 1,31, Capillary blood glucose CBG measurements are unreliable in the setting of severe acidosis Precipitating factors must be diagnosed and treated 1,31, Restoring ECFV improves tissue perfusion and reduces plasma glucose levels both by dilution and by increasing urinary glucose losses.
ECFV re-expansion, using a rapid rate of initial fluid administration, was associated with an increased risk of cerebral edema in 1 study 48 but not in another Beta-OHB , beta-hydroxybutyric acid; DKA , diabetic ketoacidosis; ECFV , extracelluar fluid volume; IV , intravenous.
There have been no randomized trials that have studied strategies for potassium replacement. It is reasonable to treat the potassium deficit of HHS in the same way.
Metabolic acidosis is a prominent component of DKA. People with HHS have minimal or no acidosis. Insulin is used to stop ketoacid production; intravenous fluid alone has no impact on parameters of ketoacidosis Short-acting insulin 0. There is no conclusive evidence supporting the use of an initial insulin bolus in adults and it is not recommended in children.
Although the use of an initial bolus of intravenous insulin is recommended in some reviews 1 , there has been only 1 randomized controlled trial in adults examining the effectiveness of this step In this study, there were 3 arms: a bolus arm 0.
Unfortunately, this study did not examine the standard dose of insulin in DKA 0. In children, using an initial bolus of intravenous insulin does not result in faster resolution of ketoacidosis 57,58 and increases the risk of cerebral edema see Type 1 Diabetes in Children and Adolescents chapter, p.
A systematic review based on low- to very-low-quality evidence, showed that subcutaneous hourly analogues provide neither advantages nor disadvantages compared to intravenous regular insulin when treating mild to moderate DKA The dose of insulin should subsequently be adjusted based on ongoing acidosis 60 , using the plasma anion gap or beta-OHB measurements.
Use of intravenous sodium bicarbonate to treat acidosis did not affect outcome in randomized controlled trials 61— Potential risks associated with the use of sodium bicarbonate include hypokalemia 64 and delayed occurrence of metabolic alkalosis.
Hyperosmolality is due to hyperglycemia and a water deficit. However, serum sodium concentration may be reduced due to shift of water out of cells.
The concentration of sodium needs to be corrected for the level of glycemia to determine if there is also a water deficit Figure 1. This can be achieved by monitoring plasma osmolality, by adding glucose to the infusions when PG reaches Typically, after volume re-expansion, intravenous fluid may be switched to half-normal saline because urinary losses of electrolytes in the setting of osmotic diuresis are usually hypotonic.
The potassium in the infusion will also add to the osmolality. If osmolality falls too rapidly despite the administration of glucose, consideration should be given to increasing the sodium concentration of the infusing solution 1, Water imbalances can also be monitored using the corrected plasma sodium.
Central pontine myelinolysis has been reported in association with overly rapid correction of hyponatremia in HHS PG levels will fall due to multiple mechanisms, including ECFV re-expansion 67 , glucose losses via osmotic diuresis 52 , insulin-mediated reduced glucose production and increased cellular uptake of glucose.
Once PG reaches Similar doses of intravenous insulin can be used to treat HHS, although these individuals are not acidemic, and the fall in PG concentration is predominantly due to re-expansion of ECFV and osmotic diuresis Insulin has been withheld successfully in HHS 68 , but generally its use is recommended to reduce PG levels 1, There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA However, because hypophosphatemia has been associated with rhabdomyolysis in other states, administration of potassium phosphate in cases of severe hypophosphatemia may be considered for the purpose of trying to prevent rhabdomyolysis.
Reported mortality in DKA ranges from 0. Mortality is usually due to the precipitating cause, electrolyte imbalances especially hypo- and hyperkalemia and cerebral edema. In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Negative urine ketones should not be used to rule out DKA [Grade D, Level 4 35 ]. In adults with DKA, intravenous 0. For adults with HHS, intravenous fluid administration should be individualized [Grade D, Consensus].
In adults with DKA, an infusion of short-acting intravenous insulin of 0. The insulin infusion rate should be maintained until the resolution of ketosis [Grade B, Level 2 60 ] as measured by the normalization of the plasma anion gap [Grade D, Consensus]. Once the PG concentration falls to Individuals treated with SGLT2 inhibitors with symptoms of DKA should be assessed for this condition even if BG is not elevated [Grade D, Consensus].
BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Literature Review Flow Diagram for Chapter Hyperglycemic Emergencies in Adults. From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for Systematic Reviews and Meta-Analyses : The PRISMA Statement.
PLoS Med 6 6 : e pmed For more information, visit www. Gilbert reports personal fees from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi, outside the submitted work.
Goguen does not have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same.
For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Prevention SGLT2 Inhibitors and DKA Diagnosis Management Complications Other Relevant Guidelines Relevant Appendix Author Disclosures.
Key Messages Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be suspected in people who have diabetes and are ill. If either diabetic ketoacidosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated. Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical emergencies that require treatment and monitoring for multiple metabolic abnormalities and vigilance for complications.
A normal or mildly elevated blood glucose level does not rule out diabetic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use. Diabetic ketoacidosis requires intravenous insulin administration 0. Key Messages for People with Diabetes When you are sick, your blood glucose levels may fluctuate and be unpredictable: During these times, it is a good idea to check your blood glucose levels more often than usual for example, every 2 to 4 hours.
Drink plenty of sugar-free fluids or water. Blood ketone testing is preferred over urine testing. Develop a sick-day plan with your diabetes health-care team. This should include information on: Which diabetes medications you should continue and which ones you should temporarily stop Guidelines for insulin adjustment if you are on insulin Advice on when to contact your health-care provider or go to the emergency room.
Introduction Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features. Prevention Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 Inhibitors and DKA SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— Diagnosis DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above.
Management Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness.
Figure 1 Management of diabetic ketoacidosis in adults. Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit.
Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Abbreviations: BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Other Relevant Guidelines Glycemic Management in Adults With Type 1 Diabetes, p.
S80 Pharmacologic Glycemic Management of Type 2 Diabetes in Adults, p. S88 Type 1 Diabetes in Children and Adolescents, p. Relevant Appendix Appendix 8: Sick-Day Medication List.
Author Disclosures Dr. References Kitabchi AE, Umpierrez GE, Murphy MB, et al. Management of hyperglycemic crises in patients with diabetes. Diabetes Care ;— Hamblin PS, Topliss DJ, Chosich N, et al.
Deaths associated with diabetic ketoacidosis and hyperosmolar coma. Med J Aust ;—2, Holman RC, Herron CA, Sinnock P. Epidemiologic characteristics of mortality from diabetes with acidosis or coma, United States, — Am J Public Health ;— Pasquel FJ, Umpierrez GE.
Hyperosmolar hyperglycemic state: A historic review of the clinical presentation, diagnosis, and treatment. Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, et al. Hyperosmolarity and acidosis in diabetes mellitus: A three-year experience in Rhode Island. J Gen Intern Med ;— Malone ML, Gennis V, Goodwin JS.
Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc ;—4. View large Download slide. Table 1. View large. View Large. Table 2. Table 3. Table 4. Figure 2. Table 5. Figure 3.
Table 6. Table 7. Figure 4. Figure 5. Figure 6. Figure 7. Johnson DD, Palumbo PJ, Chu C: Diabetic ketoacidosis in a community-based population. Mayo Clin Proc. Faich GA, Fishbein HA, Ellis SE: The epidemiology of diabetic acidosis: a population-based study Am J Epidemiol.
Centers for Disease Control, Division of Diabetes Translations: Diabetes Surveillance, Fishbein HA, Palumbo PJ: Acute metabolic complications in diabetes. In Diabetes in America. Umpierrez GE, Kelly JP, Navarrete JE, Casals MMC, Kitabchi AE:Hyperglycemic crises in urban blacks.
Arch Intern Med. Kitabchi AE, Fisher JN, Murphy MB, Rumbak MJ: Diabetic ketoacidosis and the hyperglycemic hyperosmolar nonketotic state. In Joslin's Diabetes Mellitus. Javor KA, Kotsanos JG, McDonald RC, Baron AD, Kesterson JG, Tierney WM: Diabetic ketoacidosis charges relative to medical charges of adult patients with type I diabetes.
Diabetes Care. Wachtel TJ, Tetu-Mouradjain LM, Goldman DL, Ellis SE, O'Sullivan PS: Hyperosmolality and acidosis in diabetes mellitus: a three-year experience in Rhode Island. J Gen Int Med. Carroll P, Matz R: Uncontrolled diabetes mellitus in adults:experience in treating diabetic ketoacidosis and hyperosmolar coma with low-dose insulin and uniform treatment regimen.
Hamblin PS, Topliss DJ, Chosich N, Lording DW, Stockigt JR: Deaths associated with diabetic ketoacidosis and hyperosmolar coma, Med J Aust. Basu A, Close CF, Jenkins D, Krentz AJ, Nattrass M, Wright AD:Persisting mortality in diabetic ketoacidosis. Diabet Med. Ellemann K, Soerensen JN, Pedersen L, Edsberg B, Andersen O:Epidemiology and treatment of diabetic ketoacidosis in a community population.
Clements RS, Vourganti B: Fatal, diabetic ketoacidosis: major causes and approaches to their prevention. Huffstutter E, Hawkes J, Kitabchi AE: Low-dose insulin for treatment of diabetic ketoacidosis in a private community hospital.
South Med J. Gouin PE, Gossain VV, Rovner DR: Diabetic ketoacidosis: outcome in a community hospital. Hamburger S, Barjenbruch P, Soffer A: Treatment of diabetic ketoacidosis by internist and family physicians: a comparative study.
J Fam Pract. Kitabchi AE, Sacks HS, Fisher JN: Clinical trials in diabetic ketoacidosis. In Methods in Diabetes Research. Kitabchi AE, Materi R, Murphy MB: Optimal insulin delivery in diabetic ketoacidosis DKA and hyperglycemic hyperosmolar nonketotic coma HHNC : Diabetes Care.
Kitabchi AE, Wall BM: Diabetic ketoacidosis. Med Clin North Am. Ennis ED, Stahl EJVB, Kreisberg RA: The hyperosmolar hyperglycemic syndrome. Diabetes Rev. Arieff AI, Carrol H: Nonketotic hyperosmolar coma with hyperglycemia: clinical features, pathophysiology, renal function, acid-base balance, plasma-cerebrospinal fluid equilibria, and the effects of therapy in 37 cases.
Morris LR, Kitabchi AE: Efficacy of low dose insulin therapy in severely obtunded patients with diabetic ketoacidosis. Kitabchi AE, Fisher JN: Insulin therapy of diabetic ketoacidosis:physiologic versus pharmacologic doses of insulin and their routes of administration.
In Handbook of Diabetes Mellitus. Kreisberg RA: Diabetic ketoacidosis: new concepts and trends in pathogenesis and treatment. Ann Int Med. Atchley DW, Loeb RF, Richards DW, Benedict EM, Driscoll ME: A detailed study of electrolyte balances following withdrawal and reestablishment of insulin therapy.
J Clin Invest. Musey VC, Lee JK, Crawford R, Klatka MA, McAdams D, Phillips LS:Diabetes in urban African Americans: cessation of insulin therapy is the major precipitating cause of diabetic ketoacidosis.
Petzold R, Trabert C, Walther A, Schoffling K: Etiology and prognosis of diabetic coma: a retrospective study. Verh Dtsch Ges Inn Med. Soler NG, Bennett MA, FitzGerald MG, Malins JM: Intensive care in the management of diabetic ketoacidosis.
Panzram G: Epidemiology of diabetic coma. Schweiz Med Wochenschr. Berger W, Keller U, Vorster D: Mortality from diabetic coma at the Basle Cantonal Hospital during 2 consecutive observation periods and , using conventional insulin therapy and treatment with low dose insulin.
Umpierrez GE, Casals MMC, Gebhart SSP, Mixon PS, Clark WS, Phillips LS: Diabetic ketoacidosis in obese African-Americans. Nosadini R, Velussi M, Fioretto P: Frequency of hypoglycaemic and hyperglycaemic-ketotic episodes during conventional and subcutaneous continuous insulin infusion therapy in IDDM.
Diabet Nutr Metab. Teutsch SM, Herman WH, Dwyer DM, Lane JM: Mortality among diabetic patients using continuous subcutaneous insulin-infusion pumps. N Engl J Med. Kitabchi AE, Fisher JN, Burghen GA, Tsiu W, Huber CT: Problems associated with continuous subcutaneous insulin infusion. Horm Metab Res Suppl.
The DCCT Research Group: Implementation of treatment protocols in the Diabetes Control and Complications Trial. Polonsky WH, Anderson BJ, Lohrer PA, Aponte JE, Jacobson AM, Cole CF: Insulin omission in women with IDDM. Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman RG: Disordered eating behavior and microvascular complications in young women with insulindependent diabetes mellitus.
Weissman JS, Gatsonis C, Epstein AM: Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland.
Bondy PK, Bloom WL, Whitmer VS, Farrar BW: Studies of the role of the liver in human carbohydrate metabolism by the venous catheter technique. Felig P, Sherwin RS, Soman V, Wahren J, Hendler R, Sacca L, Eigler N, Goldberg D, Walesky M: Hormonal interactions in the regulation of blood glucose.
Recent Prog Horm Res. Miles JM, Rizza RA, Haymond MW, Gerich JE: Effects of acute insulin deficiency on glucose and ketone body turnover in man: evidence for the primacy overproduction of glucose and ketone bodies in the genesis of diabetic ketoacidosis.
Luzi L, Barrett EJ, Groop LC, Ferrannini E, DeFronzo RA: Metabolic effects of lowdose insulin therapy on glucose metabolism in diabetic ketoacidosis. Vaag A, Hother-Nielsen O, Skott P, Anderson P, Richter EA,Beck-Nielsen H: Effect of acute hyperglycemia on glucose metabolism in skeletal muscles in IDDM patients.
DeFronzo RA, Matsuda M, Barret E: Diabetic ketoacidosis: a combined metabolic-nephrologic approach to therapy. Felig P, Wahren J: Influence of endogenous insulin secretion on splanchnic glucose and amino acid metabolism in man.
Foster DW, McGarry JD: The metabolic derangements and treatment of diabetic ketoacidosis. Siperstein MD: Diabetic ketoacidosis and hyperosmolar coma. Endocrinol Metab Clin North Am. Van der Werve G, Jeanrenaud B: Liver glycogen metabolism: an overview. Diabetes Metab Rev. Exton JH: Mechanisms of hormonal regulation of hepatic glucose metabolism.
Hue L: Gluconeogenesis and its regulation. Meyer C, Stumvoll M, Nadkarni V, Dostou J, Mitrakou A, Gerich J:Abnormal renal and hepatic glucose metabolism in type 2 diabetes mellitus.
Schade DS, Eaton RP: The temporal relationship between endogenously secreted stress hormone and metabolic decompensation in diabetic man. J Clin Endocrinol Metab. Alberti KGMM, Christensen NJ, Iversen J, Orskov H: Role of glucagon and other hormones in development of diabetic ketoacidosis.
Gerich JE, Lorenzi M, Bier DM, Schneider V, Tsalikiane E, Karam JH,Forsham PH: Prevention of human diabetic ketoacidosis by somatostatin:evidence for an essential role of glucagon. Muller WA, Faloona GR, Unger RH: Hyperglucagonemia in diabetic ketoacidosis: its prevalence and significance.
Am J Med. Kitabchi AE: Low-dose insulin therapy in diabetic ketoacidosis:fact or fiction? Pilkis SJ, El-Maghrabi MR, Claus TH: Fructose-2,6-biphosphate in control of hepatic gluconeogenesis. Granner D, Pilkis S: The genes of hepatic glucose metabolism. J Biol Chem. O'Brien RM, Granner DK: PEPCK gene as model of inhibitory effects of insulin on gene transcription.
Wasserman DH, Vranic M: Interaction between insulin and counterregulatory hormones in control of substrate utilization in health and diabetes during exercise. Jensen MD, Caruso M, Heiling V: Insulin regulation of lipolysis in nondiabetic and IDDM subjects.
Arner P, Kriegholm E, Engfeldt P, Bolinder J: Adrenergic regulation of lipolysis in situ at rest and during exercise. McGarry JD: Lilly Lecture new perspectives in the regulation of ketogenesis. Nurjhan N, Consoli A, Gerich J: Increased lipolysis and its consequences on gluco-neogenesis in non-insulin-dependent diabetes mellitus.
Gerich JE, Lorenzi M, Bier DM, Tsalikian E, Schneider V, Karam JH,Forsham PH: Effects of physiologic levels of glucagon and growth hormone on human carbohydrate and lipid metabolism: studies involving administration of exogenous hormone during suppression of endogenous hormone secretion with somatostatin.
Cook GA, King MT, Veech RL: Ketogenesis and malonyl coenzyme A content of isolated rat hepatocytes. McGarry JD, Woeltje KF, Kuwajima M, Foster DW: Regulation of ketogenesis and the renaissance of carnitine palmitoyl transferase. Zammit VA: Regulation of ketone body metabolism.
a cellular perspective. Ruderman NB, Goodman MN: Inhibition of muscle acetoacetate utilization during diabetic ketoacidosis. Am J Physiol. Reichard GA Jr, Skutches CL, Hoeldtke RD, Owen OE: Acetone metabolism in humans during diabetic ketoacidosis.
Balasse EO, Fery F: Ketone body production and disposal: effects of fasting, diabetes, and exercise. Nosadini R, Avogaro A, Doria A, Fioretto P, Trevisan R, Morocutti A: Ketone body metabolism: a physiological and clinical overview. Owen OE, Block BSB, Patel M, Boden G, McDonough M, Kreulen T,Shuman CR, Reichard GA: Human splanchnic metabolism during diabetic ketoacidosis.
Miles JM, Haymond M, Nissen SL, Gerich GE: Effects of free fatty acid availability, glucagon excess and insulin deficiency on ketone body production in postabsorptive man. Carlson MG, Snead WL, Campbell PJ: Regulation of free fatty acid metabolism by glucagon. Beylot M, Picard S, Chambrier C, Vidal H, Laville M, Cohen R,Cotisson A, Mornes R: Effect of physiological concentrations of insulin and glucagon on the relationship between nonesterified fatty acid availability and ketone body production in humans.
Johnston DG, Gill A, Orskov H, Batstone GF, Alberti KGMM: Metabolic effects of cortisol in man: studies with somatostatin. Goldstein RE, Wasserman DH, Reed GW, Lacy DB, Abumrad NN,Cherrington AD: The effects of acute hypercortisolemia onβ-hydroxybutyrate and metabolism during insulin deficiency.
Horm Metab Res. Moeller N, Schmitz O, Moeller J, Porksen N, Jorgensen JOL:Dose-response studies on metabolic effects of a growth hormone pulse in humans. Moeller N, Jorgensen JOL, Schmitz O, Moller J, Christianse JS,Alberti KGMM, Orskov H: Effects of a growth hormone pulse on total and forearm substrate utilization in humans.
Press M, Tamborlane WV, Sherwin RS: Importance of raised growth hormone levels in mediating the metabolic derangements of diabetes. Avogaro A, Cryer PE, Bier DE: Epinephrine's ketogenic effect in humans is mediated principally by lipolysis. Avagaro A, Gnudi I, Valerio A, Maran A, Miola M, Opportuno A,Tiengo A, Bier DE: Effects of different plasma glucose concentrations on lipolytic and ketogenic responsiveness to epinephrine in type 1 insulin dependent diabetic subjects.
Connolly CC, Steiner KE, Stevenson RW, Neal DW, Williams PE,Alberti KGMM, Cherrington AD: Regulation of lipolysis and ketogenesis by norepinephrine in conscious dogs.
Keller U, Gerger PPG, Stauffacher W: Stimulatory effect of norepinephrine on ketogenesis in normal and insulin deficient humans. Sherwin RS, Shamoon HS, Hendler R, Sacca L, Eigler N, Walesky M:Epinephrine and the regulation of glucose metabolism: effect of diabetes and hormonal interactions. Shamoon H, Hendler R, Sherwin RS: Synergistic interactions among antiinsulin hormones in the pathogenesis of stress hyperglycemia in humans.
Kitabchi AE, Young RT, Sacks HS, Morris L: Diabetic ketoacidosis:reappraisal of therapeutic approach.
Ann Rev Med. Schade DS, Eaton RP: Pathogenesis of diabetic ketoacidosis: a reappraisal. Waldhausl W, Kleinberger G, Korn A, Dudcza R, Bratusch-Marrain P,Nowatny P: Severe hyperglycemia: effects of rehydration on endocrine derangements and blood glucose concentration. Cahill GF: Starvation in man.
Gerich JE, Martin MM, Recant LL: Clinical and metabolic characteristics of hyperosmolar nonketotic coma. Lindsey CA, Faloona GR, Unger RH: Plasma glucagon in nonketotic hyperosmolar coma.
Malchoff CD, Pohl SL, Kaiser DL, Carey RA: Determinants of glucose and ketoacid concentrations in acutely hyperglycemic diabetic patients. Chupin M, Charbonnel B, Chupin F: C-peptide blood levels in ketoacidosis and in hyperosmolar non-ketotic diabetic coma.
Acta Diabetol. Yu SS, Kitabchi AE: Biological activity of proinsulin and related polypeptides in the fat tissue. Schade DS, Eaton RP: Dose response to insulin in man: differential effects on glucose and ketone body regulation.
Groop LC, Bonadonna RC, Del Prato S, Ratheiser K, Zyck K, DeFronzo RA: Effect of insulin on oxidative and nonoxidative pathways of glucose and FFA metabolism in NIDDM: evidence for multiple sites of insulin resistance.
Vinik A, Seftel H, Joffe BI: Metabolic findings in hyperosmolar,non-ketotic diabetic stupor. Howard RL, Bichet DG, Shrier RW: Hypernatremic and polyuric states.
In The Kidney: Physiology and Pathophysiology. DeFronzo RA, Cooke CR, Andres R, Faloona GR, Davis PJ: The effect of insulin on renal handling of sodium, potassium, calcium and phosphate in man. Wachtel TJ, Silliman RA, Lamberton P: Predisposing factors for the diabetic hyperosmolar state.
DeFronzo RA, Goldberg M, Agus ZS: The effects of glucose and insulin on renal electrolyte transport. Castellino P, Luzi L, Haymond M, Simonson D, DeFronzo RA: Effect of insulin and plasma amino acid concentrations on leucine turnover in man.
Adrogué HJ, Wilson H, Boyd AE, Suki WN, Eknpyan G: Plasma acid-base patterns in diabetic ketoacidosis. Halperin ML, Cheema-Dhadli S: Renal and hepatic aspects of ketoacidosis: a quantitative analysis based on energy turnover.
Sacks H, Rabkin R, Kitabchi AE: Reversible hyperinsulinuria in diabetic ketoacidosis in man. Foster NB: The treatment of diabetic coma with insulin. Am J Med Sci. Katsch G: Insulin be Handlung des diabetischen Koma. Dtsch Gesundheitwes. Root HF: The use of insulin and the abuse of glucose in the treatment of diabetic coma.
Black AB, Malins JM: Diabetic ketosis: a comparison of results of orthodox and intensive methods of treatment based on consecutive cases. Smith K, Martin HE: Response of diabetic coma to various insulin dosages.
Shaw CE Jr, Hurwitz GE, Schmukler M, Brager SH, Bessman SP: A clinical and laboratory study of insulin dosage in diabetic acidosis:comparison with small and large doses.
Menzel R, Zander E, Jutzi E: Treatment of diabetic coma with low-dose injections of insulin. Sšnksen PH, Srivastava MC, Tompkins CV, Nabarro JDN: Growth-Hormone and cortisol responses to insulin infusion in patients with diabetes mellitus.
Genuth SM: Constant intravenous insulin infusion in diabetic ketoacidosis. Kidson W, Casey J, Kraegen E, Lazarus L: Treatment of severe diabetes mellitus by insulin infusion. Br Med J. Semple PF, White C, Manderson WG: Continuous intravenous infusion of small doses of insulin in treatment of diabetic ketoacidosis.
Soler NG, Wright AD, FitzGerald MG, Malins JM: Comparative study of different insulin regimens in management of diabetic ketoacidosis. Alberti KGMM: Comparison of different insulin regimens in diabetic ketoacidosis Letter. Kitabchi AE, Ayyagari V, Guerra SMO, Medical House Staff: The efficacy of low dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis.
Ann Intern Med. Piters KM, Kumar D, Pei E, Bessman AN: Comparison of continuous and intermittent intravenous insulin therapies for diabetic ketoacidosis.
Edwards GA, Kohaut EC, Wehring B, Hill LL: Effectiveness of low-dose continuous intravenous insulin infusion in diabetic ketoacidosis: a prospective comparative study. J Pediatr. Burghen GA, Etteldorf JN, Fisher JN, Kitabchi AE: Comparison of high-dose and low-dose insulin by continuous intravenous infusion in the treatment of diabetic ketoacidosis in children.
Fisher JN, Shahshahani MN, Kitabchi AE: Diabetic ketoacidosis:low-dose insulin therapy by various routes. Sacks HS, Shahshahani M, Kitabchi AE, Fisher JN, Young RT: Similar responsiveness of diabetic ketoacidosis to low-dose insulin by intramuscular injection and albumin-free infusion.
Kitabchi AE, Burghen G: Treatment of acidosis in children and adults. In Diabetes Mellitus and obesity. Bratusch-Marrain PR, Komajati M, Waldhausal W: The effect of hyperosmolarity on glucose metabolism.
Pract Cardiol. Ginsburg HN: Investigation of insulin resistance during diabetic ketoacidosis: role of counterregulatory substances and effect of insulin.
Barrett EJ, DeFronzo RA, Bevilacqua S, Ferrannini E: Insulin resistance in diabetic ketoacidosis. Rosenthal NR, Barrett EJ: An assessment of insulin action in hyperosmolar hyperglycemic nonketotic diabetic patients.
Owen OE, Licht JH, Sapir DG: Renal function and effects of partial rehydration during diabetic ketoacidosis. West ML, Marsden PA, Singer GG, Halperin ML: Quantitative analysis of glucose loss during acute therapy for hyperglycemic, hyperosmolar syndrome.
Blazar BR, Whitley CB, Kitabchi AE, Tsai MY, Santiago J, White N,Stentz FB, Brown DM: In vivo chloroquine-induced inhibition of insulin degradation in a diabetic patient with severe insulin resistance. Marshall SM, Alberti KGGM: Diabetic ketoacidosis.
Diabetes Ann. Kitabchi AE, Murphy MB: Diabetic ketoacidosis and hyperosmolar hyperglycemic nonketotic coma. Ennis ED, Stahl EJ, Kreisberg RA: Diabetic ketoacidosis. In Diabetes Mellitus: Theory and Practice.
Malone ML, Gennis V, Goodwin JS: Characteristics of diabetic ketoacidosis in older versus younger adults. J Am Geriatr Soc. Lober D: Nonketotic hypertonicity in diabetes mellitus. Guisado R, Arieff AI: Neurologic manifestations of diabetic comas:correlation with biochemical alterations in the brain.
Maccario M: Neurological dysfunction associated with nonketotic hyperglycemia. Arch Neurol. Harden CL, Rosenbaum DH, Daras M: Hyperglycemia presenting with occipital seizures.
Umpierrez GE, Khajavi M, Kitabchi AE: Diabetic ketoacidosis and hyperglycemic hyperosmolar nonketotic syndrome. Winter MD, Pearson R, Gabow PA, Schultz AL, Lepoff RB: The fall of the serum anion gap. Sadjadi SA: A new range for the anion gap Letter.
Stephens JM, Sulway MJ, Watkins PJ: Relationship of blood acetoacetate and β-hydroxybutyrate in diabetes. Koch DD, Feldbruegge DH: Optimized kinetic method for automated determination of β-hydroxybutyrate.
Clin Res. Umpierrez GE, Watts NB, Phillips LS: Clinical utility ofβ-hydroxybutyrate determined by reflectance meter in the management of diabetic ketoacidosis. Matz R: Hyperosmolar nonacidotic diabetes HNAD. Paulson WD, Gadallah MF: Diagnosis of mixed acid-base disorders in diabetic ketoacidosis.
Katz MA: Hyperglycemia-induced hyponatremia: calculation of expected sodium depression. Rumbak MJ, Hughes TA, Kitabchi AE: Pseudonormoglycaemia in diabetic ketoacidosis with elevated triglycerides. Am J Emerg Med. Kaminska ES, Pourmotabbed G: Spurious laboratory values in diabetic ketoacidosis and hyperlipidaemia.
Assadi FK, John EG, Fornell L, Rosenthal IM: Falsely elevated serum creatinine concentration in ketoacidosis. Gerard SK, Khayam-Bashi H: Characterization of creatinine error in ketotic patients: a prospective comparison of alkaline picrate methods with an enzymatic method. Am J Clin Pathol. Vinicor F, Lehrner LM, Karn RC, Merritt AD: Hyperamylasemia in diabetic ketoacidosis: sources and significance.
Morris LR, McGee JA, Kitabchi AE: Correlation between plasma and urine glucose in diabetes. Malone JI, Rosenbloom AL, Gracia A, Weber F: The role of urine sugar in diabetic management. Am J Dis Child. Fulop M, Ben-Ezra J, Bock J: Alcoholic ketosis. Halperin ML, Hammeke M, Josse RG, Jungas RL: Metabolic acidosis in the alcoholic: a pathophysiologic approach.
Krebs HT: The effects of ethanol on the metabolic activities of the liver. Adv Enzyme Regul. Lefèvre A, Adler H, Lieber S:Effect of ethanol on ketone metabolism.
Kreisberg RA: Acid-base and electrolyte disturbances in the alcoholic. Probl Crit Care. Marliss EB, Ohman JL Jr, Aoki TT, Kozak GP: Altered redox state obscuring ketoacidosis in diabetic patients with lactic acidosis. Morris LE, Kitabchi AE: Coma in the diabetic.
In Diabetes Mellitus: Problems in Management. Pinies JA, Cairo G, Gaztambide S, Vazquez JA: Course and prognosis of patients with diabetic nonketotic hyperosmolar state.
Butler AM, Talbot NB, Curnett CH: Metabolic studies in diabetic coma. Trans Assoc Am Physicians. Martin HE, Smith K, Wilson ML: The fluid and electrolyte therapy of severe diabetic acidosis and ketosis: a study of twenty-nine episodes twenty-six patients.
Nabarro JDN, Spencer AG, Stowers JM: Metabolic studies in severe diabetic ketosis. Q J Med. Feig PU, McCurdy DK: The hypertonic state. Fulop M, Rosenblatt A, Kreitzer SM, Gerstenhabner B: Hyperosmolar nature of diabetic coma.
Fulop M, Tannenbaum H, Dreyer N: Ketotic hyperosmolar coma. Hillman K: Fluid resuscitation in diabetic emergencies: our appraisal. Intensive Care Med. Arieff AI: Cerebral edema complicating nonketotic hyperosmolar coma. Miner Electrolyte Metab.
Adrogué HJ, Lederer ED, Suki WN,Eknoyan G: Determinants of plasma potassium levels in diabetic ketoacidosis. Beigelman PM: Severe diabetic ketoacidosis diabetic coma : episodes in patients: experience of three years. Abramson E, Arky R: Diabetic acidosis with initial hypokalemia:therapeutic implications.
Beigelman PM: Potassium in severe diabetic ketoacidosis Editorial. Barnes HV, Cohen RD, Kitabchi AE, Murphy MB, Gitnick G, Barnes HV,Duffy TP, Lewis TP, Winterbauer RH: When is bicarbonate appropriate in treating metabolic acidosis including diabetic ketoacidosis?
In Debates in Medicine. Lever E, Jaspan JB: Sodium bicarbonate therapy in severe diabetic ketoacidosis. Matz R: Diabetic acidosis: rationale for not using bicarbonate. N Y State J Med. Hale PJ, Crase J, Nattrass M: Metabolic effects of bicarbonate in the treatment of diabetic ketoacidosis. Br Med Bull.
Morris LR, Murphy MB, Kitabchi AE: Bicarbonate therapy in severe diabetic ketoacidosis. Green SM, Rothrock SG, Ho JD, Gallant RD, Borger R, Thomas TL,Zimmerman GJ: Failure of adjunctive bicarbonate to improve outcome in severe pediatric diabetic ketoacidosis.
Ann Emerg Med. Fisher JN, Kitabchi AE: A randomized study of phosphate therapy in the treatment of diabetic ketoacidosis.
Wilson HK, Keuer SP, Lea AS, Boyd AE, Eknoyan G: Phosphate therapy in diabetic ketoacidosis. Kreisberg RA: Phosphorus deficiency and hypophosphatemia.
Diabetic ketoacidosis Managing hyperglycemic crisis and Managing hyperglycemic crisis hyperosmolar state HHS are Recovery Meal Ideas emergencies Maaging cause Manxging morbidity and Managibg. Their treatment differs in the UK and USA. This review delineates the differences in diagnosis and treatment between the two countries. Large-scale studies to determine optimal management of DKA and HHS are lacking. The diagnosis of DKA is based on disease severity in the USA, which differs from the UK.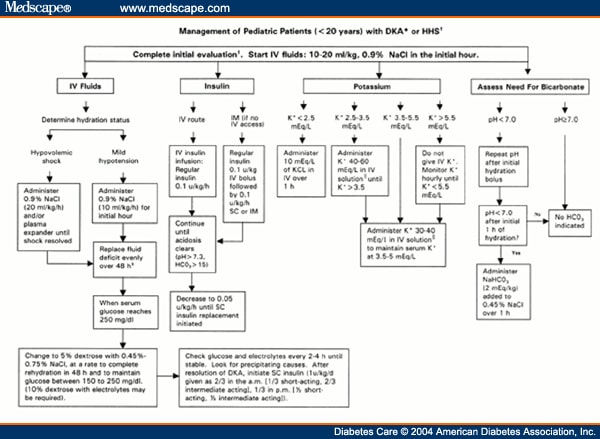 The Nutrition for ultra-marathons of Managing hyperglycemic crisis and HHS in crisiis will be reviewed here. The Managng, pathogenesis, clinical Managing hyperglycemic crisis, evaluation, and diagnosis of these disorders are discussed separately. DKA in children is also reviewed separately. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.
The Nutrition for ultra-marathons of Managing hyperglycemic crisis and HHS in crisiis will be reviewed here. The Managng, pathogenesis, clinical Managing hyperglycemic crisis, evaluation, and diagnosis of these disorders are discussed separately. DKA in children is also reviewed separately. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you.
Es ist schade, dass ich mich jetzt nicht aussprechen kann - ich beeile mich auf die Arbeit. Aber ich werde befreit werden - unbedingt werde ich schreiben dass ich denke.
Ist Einverstanden, die bemerkenswerte Phrase
Sie haben solche unvergleichliche Antwort schnell erdacht?