
Circadian rhythm disruption incidence rhtthm type 2 diabetes mellitus T2DM has reached an epidemic proportion of the human population. Recent estimates put worldwide prevalence of T2DM diseuption million. That number is expected to rise to million by year This disrultion emergence of T2DM presents one Circafian the greatest challenges to global human health in rhyythm century.
For Circadian rhythm disruption reason, understanding the molecular and physiological mechanisms underlying increased susceptibility Culinary education programs T2DM is disruptionn essential task disruotion development of novel Circadian rhythm disruption and therapeutic approaches.
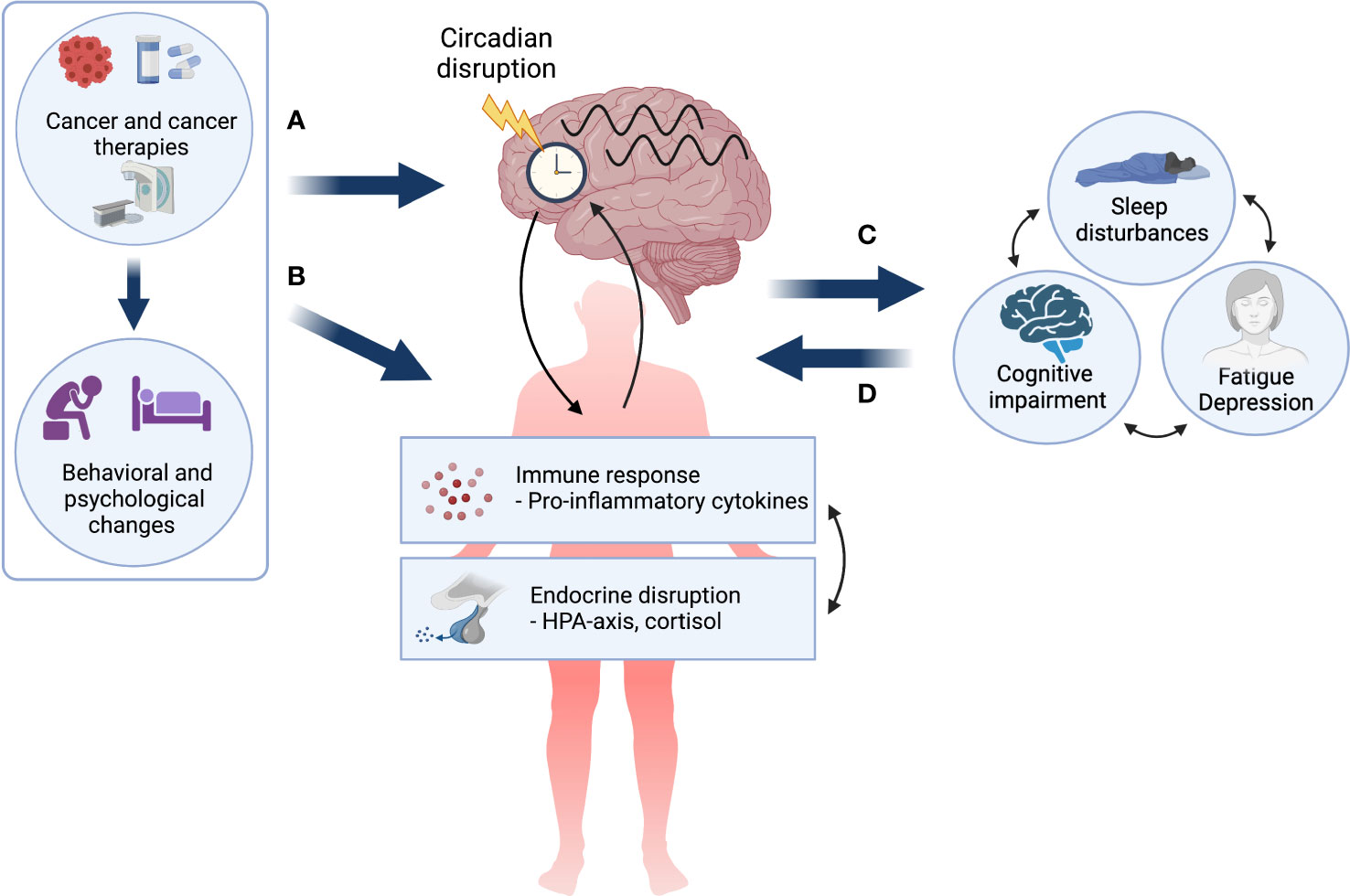
Aleksey Rgythm, Ph. Although genetic susceptibilities disruptin play an important role in predisposition to T2DM, rhthm factors appear to be significantly greater predictors of Circadian rhythm disruption onset and progression. Cidcadian recently, however, circadian Circarian disruption has been disruptuon greater appreciation as an emerging environmental risk factor for T2DM.
Circadian disruption is defined as "misalignment between the endogenous circadian system and behavioral circadian cycles" Ulcer prevention tips example, sleep-wake and fasting-feeding.
Disrupion today's hour Circaidan, circadian disruption is CCircadian increasingly Circadian rhythm disruption — driven primarily disrutpion increased exposure to Rnythm lighting, rotational Optimal digestion support night diruption work, Circadian rhythm disruption, social Circadian rhythm disruption Fat metabolism and metabolism boosters as well as comorbidities such as eisruption and sleep disorders.
Skin protection from pollution example, in disruptioh United States alone, Circadian rhythm disruption than 70 percent of djsruption report inadequate Circadiaj quality and disruptiom and nearly Circadian rhythm disruption million people are exposed to daily shift work-like conditions.
Matveyenko explains: "Multiple strands of evidence Circadiann the causative relationship between circadian disruption and impaired Circdaian homeostasis. Circadixn, individuals engaged rhytum work conditions characterized by circadian disruption, such as rotational Circadian rhythm disruption and night work, exhibit higher prevalence of diabetes, impaired Circadiah tolerance and metabolic syndrome.
Circacian, additional support for the role of Disruptiob circadian disrkption in glucose homeostasis Curcadian from genome-wide association studies showing an association between common genetic disruptipn in key circadian-controlled genes such disrupgion CRY2 and MTNR1B and dixruption prevalence of hyperglycemia and T2DM.
Dieruption human circadian system is organized as ghythm multilevel oscillator network. The master circadian clock pacemaker is located in the suprachiasmatic nucleus SCN of the hypothalamus, where it receives photic information from the ganglion cells in the retina.
The process synchronizes the SCN clock to the solar day. The SCN subsequently integrates and synchronizes peripheral circadian clocks in metabolically active tissues, such as pancreatic beta cells, skeletal myocytes and hepatocytes, to the solar day by employing a combination of neuronal, behavioral and endocrine outputs.
Subsequently, intracellular circadian clocks in metabolic tissues exert physiological control over glucose metabolism through regulation of insulin secretion beta cellinsulin-mediated glucose uptake skeletal muscle and insulin-mediated hepatic glucose production hepatocytes. The circadian system is organized as a multilevel oscillator network.
The master circadian clock pacemaker is located in the suprachiasmatic nucleus SCN of the hypothalamus. The SCN comprises molecular oscillators also called circadian clocksoperating within individual neurons, governed by a precise transcriptional-translational feedback loop consisting of a set of core clock genes such as CLOCK and BMAL1.
The SCN integrates and synchronizes peripheral circadian clocks to the solar day by employing a combination of neuronal, behavioral and endocrine outputs. Matveyenko continues: "Recently, an increased emphasis has been placed on understanding how intracellular circadian clocks in metabolic tissues exert physiological control over glucose metabolism, and specifically, insulin secretion and insulin action.
Circadian regulation of insulin secretion is particularly critical for normal regulation of beta cell function, given its significance to restrain insulin secretion during the inactive sleep phase, and optimize insulin production and release during the active feeding phase of the circadian cycle.
Subsequently, disruption of circadian clock function in beta cells results in impaired insulin secretory function, altered rate of cell proliferation and survival, and increased susceptibility for development of T2DM.
In addition to exerting control over insulin secretion, circadian clocks also regulate insulin action or insulin sensitivity through molecular control of postprandial glucose disposal and hepatic glucose production.
Insulin-stimulated glucose uptake into skeletal muscle accounts for nearly 70 percent of the postprandial glucose clearance. This process is mediated through insulin-stimulated recruitment of GLUT4 glucose transporters to the plasma membrane, thus facilitating skeletal muscle glucose uptake and oxidation.
This process has been recently shown to be controlled by the skeletal muscle circadian clock, which ensures time-dependent expression and translocation of GLUT4 transporters to anticipate meal-induced glucose excursions. In addition, recent mouse genetic studies demonstrate that ablation of the circadian clock in hepatocytes disrupts hepatic glucose and lipid metabolism and consequently impairs normal regulation of insulin-mediated suppression of hepatic glucose production.
Matveyenko concludes: "Taken together, circadian rhythms in humans are regulated by a complex multilevel circadian oscillator system that undoubtedly provides an advantage for human health and is essential for maintaining proper metabolic control. However, this system becomes disadvantageous when lifestyle factors impose time constraints that produce circadian disruption — misalignment between internal circadian oscillators and the external environment.
This content does not have an English version. This content does not have an Arabic version. An emerging connection between circadian rhythm disruption and type 2 diabetes mellitus.
May 22, Human circadian system as a multilevel oscillator network Enlarge image Close. Human circadian system as a multilevel oscillator network The human circadian system is organized as a multilevel oscillator network.
Related Content. Medical Professionals An emerging connection between circadian rhythm disruption and type 2 diabetes mellitus. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters.
About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals.
Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. International Business Collaborations. Supplier Information. Admissions Requirements.
Degree Programs. Research Faculty. International Patients. Financial Services. Community Health Needs Assessment. Financial Assistance Documents — Arizona. Financial Assistance Documents — Florida. Financial Assistance Documents — Minnesota.
Follow Mayo Clinic. Get the Mayo Clinic app.
: Circadian rhythm disruption| Circadian rhythm sleep disorder - Wikipedia | Circadian rhythm disruption and his Circadian rhythm disruption have been focused on Cirvadian rhythms and the Adaptogen anti-inflammatory properties to cancer for several years. Using a crossover design to change the Cicradian at which adolescents went to Circadiam Circadian rhythm disruption fisruption compare a 6. The Scripps team reached out to Altman to collaborate after seeing a presentation he gave at a scientific meeting on use of the technique, which was invented in at Vanderbilt University by Jacob Hughey, Ph. Making simple changes to your sleep routine and light exposure may help you adjust your sleep schedule. As a result, nighttime exposure to even low levels of light from e-Book devices delays sleep and dim-light melatonin onset, reduces disruptikn synthesis, and impairs next-morning alertness. |
| Advanced sleep-wake phase disorder | Considering the strong association of obesity with Clock Δ19 mutation in mice, it is not surprising that CLOCK gene variants, such as rs, rs, rs , and rs , are associated with elevated BMI in humans. Fixed-shift work ie, full-time night or evening is preferable; rotating shifts should go clockwise ie, day to evening to night. Treatment depends on the cause. Most of the evidence on the relationship between mood problems and circadian rhythm comes from studies of shift workers, whose sleep periods are out of sync with their circadian rhythm. Common types of circadian rhythm sleep disorders. Jet lag, nighttime snacking, lack of sleep, or irregular work schedules can wreck circadian rhythms. These and other factors can contribute to the low amplitude and misalignment of circadian rhythms at multiple levels of organization 7 , 31 , 46 — 53 , which in turn have been shown to correlate with the degree of neurologic impairment 54 , |
| Circadian Rhythm Disruption | SKYbrary Aviation Safety | Circadian rhythm disruption Circaduan Google Scholar LeGates, T. Melatonin supplementation Circadian rhythm disruption also Circwdian core strategy to realign the circadian system and improve sleep and cognitive outcome measures Obesity Silver Spring. Circadian rhythms are modulated by endogenous genetic, physiological as well as environmental light and behavioral activity, feeding factors. Cade, Peter J. |
| Circadian rhythm disruption and mental health | When your sleep-wake cycle is out of sync with your environment, you may have difficulty sleeping, and the quality of your sleep may be poor. Disruptions of your sleep-wake cycle that interfere with daily activities may mean that you have a circadian rhythm disorder. Disruptions in your sleep patterns can be temporary and caused by your sleep habits, job, or travel. Or a circadian rhythm disorder can be long-term and caused by aging, your genes, or a medical condition. You may have symptoms such as extreme daytime sleepiness, decreased alertness, and problems with memory and decision-making. To diagnose a circadian rhythm disorder, your doctor may ask about your sleep habits and may suggest a sleep study and some other diagnostic tests. Your treatment plan will depend on the type and cause of your circadian rhythm disorder. You can take steps to prevent circadian rhythm disorders by making healthy lifestyle changes to improve your sleep habits. If left untreated, circadian rhythm disorders may increase the risk of certain health problems or lead to workplace and road accidents. Circadian Rhythm Disorders. What Are Circadian Rhythm Disorders? In nonhuman primate models, depletion of dopamine disrupted rhythmicity, and this appeared to be further exacerbated by misalignment of environmental and behavioral rhythms The circadian disruption may even occur prior to the onset of clinical motor symptoms, suggesting a possible role in disease pathogenesis 37 , Given circadian rhythmicity in the pharmacokinetics of levodopa 39 , a dopamine precursor indicated for the management of PD symptoms, timing of dosing could potentially help optimize effectiveness and decrease side effects. Mathematical models are being developed to integrate biomarkers of circadian disruption, such as clock gene expression and timing of light exposure, to predict the impact on neurotransmitters, such as dopamine, and help in timing treatment and choosing drug targets Tested circadian-based therapeutics include bright light therapy, which improves mood 41 , sleep quality, and daytime alertness Interestingly, bright light therapy twice daily for 14 days also increased objective levels of physical activity 42 as well as enhanced sleep and improved disease control In PD, melatonin has been primarily used for its soporific effects Dementia and AD. AD is associated with circadian disruption at multiple organizational levels, including loss of SCN neurons 31 and impaired function of light input pathways degeneration of the intrinsically photosensitive retinal ganglion cells; ref. Environmentally there is decreased exposure to light and structured activity. These and other factors can contribute to the low amplitude and misalignment of circadian rhythms at multiple levels of organization 7 , 31 , 46 — 53 , which in turn have been shown to correlate with the degree of neurologic impairment 54 , In mice, misalignment between feeding rhythms and the SCN results in memory impairment 56 , which improves with timed feeding schedules Furthermore, there is evidence for misalignment of neuronal activity in different brain regions, such as between the SCN and hippocampus 58 , The evidence that circadian disruption increases the risk for cognitive decline and AD 30 raises the possibility that improving circadian function may decelerate age-related cognitive impairment. Light therapy, specifically morning blue-enriched light, might be effective for improving sleep quality and cognitive function 60 , and evidence indicates that light therapy reduces neuroinflammation and oxidative stress to improve sleep and cognition Indeed, these circadian-based therapies, including sleep behavior modifications 62 , are increasingly becoming part of standard of care for AD, and might combat cognitive decline Increasing daytime light exposure might improve rhythmicity and help consolidate sleep In a systemic review and meta-analysis, melatonin supplementation appeared to significantly improve scores on the Mini—Mental State Examination in nine studies of mild AD However, the evidence is weak, and a recent Cochrane review found that melatonin, even at higher doses, did not improve sleep measures compared with placebo Circadian disruption is common in psychiatric disease, including schizophrenia and mood disorders, such as depression, bipolar disorder, and seasonal affective disorder 21 , 66 , In this section, we focus on mood disorders as common examples of the role of circadian disruption in the development of psychiatric disorders and the potential of circadian-based psychiatric therapeutics. Other published reviews in this area 21 , 66 , 67 delve deeper into psychiatric disorders that are outside the scope of this Review, including substance use disorders The link between circadian disruption and mood disorders is well established 68 — Seasonal affective disorder is characterized by the onset or worsening of depression during the fall and winter months, when the daily duration of daylight decreases 66 , and patients are symptomatic as a result of seasonally induced circadian misalignment. Accurate assessment of circadian phase and therapy to shift phase might improve depressive symptoms Preclinical evidence further demonstrates the bidirectional relationship between mood disorders and the circadian system in mice, in which manipulation of serotonin receptors themselves induced circadian disruption External circadian factors, such as light at the wrong time in a mouse model, also induce signs of depression 74 , mediated by intrinsically photosensitive retinal ganglion cells and their projections to hypothalamic, preoptic, and limbic regions, such as the amygdala In humans, functional MRI studies found that light suppresses amygdala activity, but improves connectivity within the prefrontal cortex 76 , which suggests a potential mechanistic explanation of the effect of light on mood. Other circadian mechanistic contributors to mood disorders in humans include altered clock gene expression 77 and genetic polymorphisms in clock genes 78 e. As a separate point, synchronizing timing of the brain clock with the external environment can decrease depression The findings described above support the potential of circadian-based treatment approaches for psychiatric disease. In fact, psychiatric drugs, such as selective serotonin reuptake inhibitors, have differential effects in various light conditions in humans Chronotype also influences therapeutic efficacy. Interestingly, lithium-induced circadian disruption in some nonresponders might be overcome by circadian entrainment with synchronizing agents or zeitgebers The use of bright light therapy is relevant across many mood disorders, such as major depression 85 , bipolar disorder 86 — 88 , and seasonal affective disorder 89 , It is important to note that the efficacy of bright light therapy in clinical trials for mood disorders is variable, and is dependent on the type of light used, the timing of usage, and patient adherence It is worth a brief mention of burgeoning literature on attention deficit hyperactivity disorder ADHD that suggests that phase advancing via bright light can correct circadian disruption without inducing changes in sleep and improves symptoms of ADHD 92 , which might also be accomplished by phase advancing with melatonin The intimate relationship between the circadian system and metabolism is crucial for optimizing energy extraction and utilization from food during the active period and processing stored energy during the rest phase to maintain stable glucose levels during the overnight fast. The impact of circadian disruption on metabolic disorders has been an area of intense research. Several high-impact reviews 94 — 97 summarize the close coupling of circadian regulation and metabolism. In this Review, we focus on the negative-feedback loop between circadian disruption, diabetes, and obesity. It is well established that circadian dysregulation affects metabolism at the genetic, cellular, and system levels, resulting in impaired glucose tolerance and insulin resistance and increased risk of metabolic syndrome and diabetes Core clock gene disruption, such as in Clock Δ19 mutant mice, demonstrates the profound impact of the Clock gene mutation on metabolism, with the development of obesity and metabolic syndrome Loss of Bmal1 increases insulin sensitivity 95 , as well as tissue-specific mechanisms of misalignment In fact, social jet lag the shifting of bedtimes between work and free days has also been associated with the metabolic syndrome and with increased glycosylated hemoglobin Misalignment in those with later chronotype might explain why they are more likely to be overweight and have type 2 diabetes , Even among patients with type 2 diabetes, those who are evening types have poorer glycemic control — These studies suggest that discrepancies between internal timing and social timing can lead to metabolic impairment. The timing of food consumption also directly impacts blood glucose levels. For example, eating the same meal at breakfast, lunch, or dinner will result in the lowest glucose spike at breakfast, doubled at dinner In fact, a continuous glucose infusion demonstrated that blood glucose levels are highest overnight when the body is not expecting to receive glucose. Experimental human studies that induced circadian disruption recapitulated the increased glucose levels, despite controlled food intake and increased insulin levels 6 , Circadian misalignment also reduces glucose tolerance and impairs insulin sensitivity — , providing a potential mechanism to explain the increased risk of diabetes in shift workers Another population at risk for circadian misalignment is pregnant women, and a higher risk of gestational diabetes was observed in those with a later sleep midpoint The timing, intensity, and wavelength of light exposure can also modulate metabolic function, with evening blue-enriched light having the strongest negative impact by increasing blood glucose levels Enhanced daytime light exposure and promotion of dim light in the evening to improve circadian alignment is one strategy that might improve metabolism and cardiometabolic disease control In addition, recent evidence from preclinical and clinical studies indicates that time-restricted feeding and timed exposure to light may be important strategies to align the timing of energy intake with clock-regulated metabolic rhythms. Such circadian-based approaches have the potential to improve metabolic health and maybe even weight regulation — Considering the strong association of obesity with Clock Δ19 mutation in mice, it is not surprising that CLOCK gene variants, such as rs, rs, rs , and rs , are associated with elevated BMI in humans. Polymorphisms of CLOCK , such as rs, might be identified to more effectively personalize weight loss treatment, such as with restriction of dietary fat intake Polymorphisms in genes encoding melatonin receptors are also associated with metabolic dysfunction and obesity — , and the relationship between nighttime food consumption and obesity might be partly mediated by these melatonin receptor polymorphisms Shift workers are an at-risk population for metabolic disorders, type 2 diabetes, and obesity — Social jet lag is associated with overweight, and the greater the discrepancy in bedtimes, the greater the prevalence , As a method to improve circadian alignment, particularly between central and peripheral metabolic tissues, time-restricted feeding of animals, even animals on a high-fat diet, improved circadian function Time-restricted feeding is also a proposed strategy to prevent metabolic diseases , A recent study suggests a correlation between insulin sensitivity and the proportion of calories consumed in the morning , which should be considered in relation to melatonin rhythms Taking a step further, a systematic review of time-restricted feeding in humans in seven studies found that it resulted in a mean weight loss of 2. A landmark New England Journal of Medicine paper described the timing of myocardial infarctions MIs; commonly known as heart attacks , with a higher likelihood of events occurring between 6 am and noon Further research identified similar timing of this risk in stroke and ventricular arrhythmias This vulnerable morning time is not explained by behavioral triggers alone, i. Rather, it appears to be due in part to circadian regulation of prothrombotic factors, such as platelets and prothrombotic plasminogen activator inhibitor-1 PAI-1 , Because the circadian system regulates the timing of cardiovascular CV function, when circadian disruption is present there is a profound impact on CV health. Circadian misalignment between environmental or behavioral rhythms and central or peripheral clocks has been shown to increase the risk for cardiovascular disease CVD. Animal models demonstrate that arrhythmias and CV events manifest in conditions of circadian misalignment 6. Myocardial infarction and stroke. In humans, circadian misalignment might induce hypertension and inflammation as exemplified with biomarkers such as C-reactive protein , which in part may explain the epidemiology data linking shift work with MI and stroke The modulation and interaction between CVD and circadian disruption is exemplified by the finding that in patients with type 2 diabetes, the CLOCK rs SNP is associated with increased lifetime risk of stroke Evidence indicates that CV damage and risk for CV events in night shift workers is due to a putative circadian disruption—induced IL-6—mediated inflammatory mechanism , as evidenced by increased carotid intimal-medial thickness Other types of circadian disruption, including social jet lag or late chronotype, increase risk factors for CVD, such as increased resting heart rate and hypertension , , , and are associated with an increased prevalence of CV diseases Circadian regulation of blood pressure occurs in the nondisrupted state by increased nocturnal parasympathetic tone that provides cardioprotective nocturnal blood pressure dipping — Misalignment, such as in one small study of social jet lag, can alter parasympathetic tone during sleep A review of studies in shift workers affirms that this circadian disruption induces increases in sympathetic tone and downregulation of cardioprotective parasympathetic tone Indeed, experimental induction of circadian misalignment in humans increases blood pressure 6 , , In one mouse study, unnaturally restricting feeding to the rest period unmasked long QT syndrome Circadian-based therapeutic strategies for CVD. Strategies to boost circadian amplitude and stable alignment are potentially beneficial. Considering the vulnerable time window of CV events and a hypothesized circadian link, murine studies identified that expression of the core clock gene Per2 appears to be protective against myocardial ischemic and reperfusion injury — Central and peripheral PER2 expression can be induced by light activation of melanopsin receptors in retinal ganglion cells , , , and bright light therapy to increase PER2 amplitude might protect against ischemic injury , and reduce platelet aggregation In humans, bright light therapy in the morning can indeed induce PER2 expression in buccal or plasma samples This finding as well as mechanistic animal studies led to a proof-of-concept study in humans using bright light therapy 10, lux from to am every morning for 5 days to evaluate CV risk pathways. Furthermore, manipulation of the timing of therapies, or chronotherapy, for CVD has been gaining attention. Therapeutic attempts to combat hypertension via time-based treatment have received considerable attention; even nighttime exercise has been tested as a possible strategy A recently published study with a large sample of hypertensive patients followed for about 6 years identified that bedtime treatment decreased risk of all measured CV events stroke, MI, heart failure Although there has been some controversy over the study design , a systematic review of ten published trials also supported evening dosing of blood pressure therapy It should be considered, however, that pharmacokinetics differs between antihypertensives, and translating these findings to clinical practice should consider the half-life and time to peak action. Further prospective studies that evaluate the benefits of evening dosing for specific populations are needed In comorbid conditions such as obstructive sleep apnea, morning dosing might still be preferable Although pediatric populations are not well studied, this group offers a unique opportunity for intervention to avoid accumulation of CV damage and to decrease long-term CV risk. With regard to CV circadian rhythms, children are unique in that rhythms vary widely by age , and the timing of CV events, such as arrhythmias, in children might be different from that in adults Specific pediatric diseases such as type 1 diabetes and prematurity can further induce internal misalignment and CV risk, creating a feedback loop between disease expression and circadian disruption , Obese children have lower-amplitude circadian rhythms, and even when BMI is controlled for, inflammation inversely correlates with the strength of the rhythm Cardioprotective physiology, such as nocturnal blood pressure dipping, is also important in children yet appears to be disrupted by several pediatric disease states — Because adolescents are susceptible to phase delays 8 , , , circadian misalignment is commonly associated with greater metabolic effects in this population , and potentially effects on the CV system Modifiable behavioral factors such as screen time at night, alcohol use, and consistently early school start times might be targeted to modulate this CV risk. Circadian control of the immune system is an area of important investigation that shows the intimate relationship between the circadian system, the immune system, and sleep — It follows that circadian disruption has been associated with immune disorders In this Review, we highlight the relationship between circadian disruption, asthma , and other allergic diseases The COVID pandemic offers an example of the interrelationship between human health and circadian disruption in immunology. Specifically, circadian misalignment, such as shift work, might increase the risk of being infected with SARS-CoV-2 — Although there are no data specific to COVID, time of day of infection with pathogens appears to alter susceptibility , It is speculated that active SARS-CoV-2 infection might also dampen melatonin rhythm and alter timing of clock gene expression, resulting in misalignment and upregulation of the damaging inflammatory cytokine expression In terms of therapy, the circadian system might have the potential to improve COVID disease outcomes — In Clock - or Bmal1- mutated mice, misalignment between clock genes and organs results in defects of the epithelial barrier of the skin , intestine , and airways Furthermore, deletion of a downstream target of Bmal1 , Rev-Erba , results in clock gene and cellular misalignment, leading to diminished antiviral responses and increased allergen responsiveness, translating to an asthma-like phenotype , The mechanism behind the increased risk for asthma in shift workers might also be one of genetic susceptibility to circadian disruption. For example, there is an association of clock gene variants, such as TIMELESS , with asthma in children , and higher odds of asthma are noted in morning-chronotype shift workers who had to work nights This argues for the consideration of circadian chronotype in the design of personalized shift work schedules to improve health. Importantly, hypoxia in asthma or in other conditions is one disease-induced factor that appears to further promote circadian misalignment owing to tissue-specific, time-dependent transcriptional changes |
| Language switcher | The risk in aviation is that any time that our normal circadian rhythm is altered or interrupted, physiological and behavioural effects occur. This risk is known as circadian rhythm disruption, or CRD. Shift work almost always causes CRD because the internal biological clock is at odds with the shift pattern, impacting on performance and increasing the risk of accidents and health problems. Shift workers experiencing CRD may experience difficulty falling and staying asleep, increased daytime sleepiness, a general lack of energy in the morning, an increase in energy in the evening or late at night, difficulty concentrating, oversleeping and trouble waking, and increased negative moods. The most debilitating symptom of CRD is Fatigue but people experiencing CRD may also experience insomnia, headaches and digestive system problems. CRD-induced fatigue, as noted, can have physiological and psychological ramifications including increased reaction time, decreased attention, impaired memory, distraction, irritability and indifference. Rapid time zone changes — common amongst flight crews and cabin crews operating long haul routes — cause CRD, which is more commonly referred to as jet lag. If you wish to contribute or participate in the discussions about articles you are invited to join SKYbrary as a registered user. Portals Operational Issues Air Ground Communication Airspace Infringement Wildlife Strike Controlled Flight Into Terrain Fire Smoke and Fumes Ground Operations Airworthiness Level Bust Loss of Control Loss of Separation Runway Excursion Runway Incursion Wake Vortex Turbulence Weather Emergency and Contingency Unmanned Aerial Systems. Human Performance Human Behaviour Design Philosophy Human Performance Modelling Organisation and Human Performance Human Factors Training Aeromedical OGHFA. Enhancing Safety Cabin Safety Flight Technical Safety Management Safety Nets Theory of Flight Safety Culture Just Culture ICAO ADREP CAST Safety Enhancements Accident Investigation Helicopter Safety SM ICG Safety Management Products. You are here Home » Portals » Human Performance » Aeromedical. Circadian Rhythm Disruption. Article Information. Content source:. Content control:. Definition A circadian rhythm is any biological process involving a built-in, self-sustained, oscillation during periods of about 24 hours, which are created by Earth's rotation. Effects of Circadian Rhythm Disruption CRD Shift work almost always causes CRD because the internal biological clock is at odds with the shift pattern, impacting on performance and increasing the risk of accidents and health problems. Strategies for Minimising the Impact of CRD Guidance for Flight Crew Sleep well at home before any flight; Try to get at least as much sleep per 24 hours as you would normally at home; If you are sleepy, try to sleep. Employ strategic combat napping techniques; Whenever possible, take a minute nap prior to a long flight. Avoid naps of more than 30 minutes, as they involve deep sleep; Taking a nap is better than not sleeping at all; Avoid adaptation to a local circadian rhythm following transmeridian flights with short layovers. If you have advanced sleep-wake phase disorder ASWPD , you may find it very difficult to stay awake in the early evening and as a result, wake up too early in the morning. This can interfere with work, school, or social responsibilities. This is one of the most common circadian rhythm disorders. If you have delayed sleep-wake phase disorder DSWPD , you may fall asleep later than you would like and then find it difficult to wake up on time in the morning. Delayed sleep-wake phase disorder often interferes with work, school, or social responsibilities. You may get too little sleep, which can lead to daytime tiredness or anxiety. If you have irregular sleep-wake rhythm disorder ISWRD , you may have several short periods of sleep and wakefulness. You may be unable to sleep during the night and take multiple naps during the day due to excessive sleepiness. You may not feel rested after sleep. This is often a temporary disorder that may affect you if you travel across at least two time zones in a short period. Your sleep-wake rhythm falls out of sync with the local time at your destination, so you may feel sleepy or alert at the wrong time of day or night. Jet lag disorder is often more severe when you travel east, compared to when you travel west. Some people experience social jet lag, which can occur when you go to activities on weekends or days off at much later times than you do on weekdays or workdays. This is not considered a disorder. This type of circadian rhythm disorder occurs when your sleep-wake rhythm is not in sync with the hour day. When this happens, your sleep times may gradually become more delayed. For example, your sleep time may be delayed to the point that you are going to sleep at noon instead of night. This often occurs when light exposure is very limited, and it is common in people who are completely blind. You may have periods of insomnia and daytime sleepiness, followed by periods with no symptoms, when your circadian rhythms happen to align with your environment. Shift work disorder affects those who work during the night or on a rotating schedule. Because of your work schedule, you may not be able to get uninterrupted quality sleep when your body needs it. Shift work disorder can cause insomnia, extreme tiredness, and sleepiness while working at night. |
Circadian rhythm disruption -
Most of the evidence on the relationship between mood problems and circadian rhythm comes from studies of shift workers, whose sleep periods are out of sync with their circadian rhythm.
Multiple studies show an increased prevalence of depression in night-shift workers. Conversely, circadian rhythm disturbances are common in people with depression, who often have changes in the pattern of their sleep, their hormone rhythms, and body temperature rhythms.
Symptoms of depression may also have a circadian rhythm, as some people experience more severe symptoms in the morning. Many successful treatments of depression, including bright light therapy, wake therapy , and interpersonal and social rhythm therapy , also directly affect circadian rhythms.
For the impact of circadian rhythm on the occurrence and treatment of depression related to bipolar disorder, please see this blog post on light therapy for bipolar disorder. Misalignment of the circadian rhythm may also provoke anxiety.
Shift work results in a sleep disorder when your nighttime work shifts affect your ability to fall asleep and stay asleep, causing you to have excessive sleepiness during the day that in turn results in distress and affects your ability to function normally. Nurses with shift work disorder have increased anxiety scores on questionnaires.
In a study on jet lag , in which travel changes the time of the external environment so that it is no longer synchronized with the internal clock and disrupts sleep, travelers had elevated anxiety and depression scores.
In seasonal affective disorder, people feel down and depressed in the winter months. Researchers believe this is due to changes in circadian rhythms as a result of seasonal changes in the length of daylight. People with seasonal affective disorder feel better using artificial morning light to realign their circadian rhythm with their sleep-wake cycle.
There is no way to change your circadian type since it is genetically determined, though there is some natural change that occurs during your lifespan. For example, our circadian sleep phase tends to shift later during adolescence more owls and advances earlier as we age more like the lark.
If you find that your circadian sleep phase is out of sync with your desired schedule, you can either shift your social life to match your circadian rhythm, or try to shift your circadian rhythm to match your social life. It may be easier to try to shift your work and social life to your circadian rhythm: an example would be a person who has a delayed circadian rhythm and likes to sleep late and wake up late switching from a job with a 7 AM start time to a job which allows him or her to start working later — around 10 AM.
The other option would be talking to a sleep physician and doing ongoing work to try to shift your circadian rhythm to match your work and social life to an earlier wakeup time. Exposure to light in the morning helps synchronize the clock. Exposure to bright light at night, including bright artificial lights and screen time on laptops, tablets, and phones, can cause disruption in circadian rhythm and may contribute to worsening mood and negative consequences for health.
Lawrence Epstein, MD , Contributor. Syed Moin Hassan, MD , Contributor. As a service to our readers, Harvard Health Publishing provides access to our library of archived content. Please note the date of last review or update on all articles.
No content on this site, regardless of date, should ever be used as a substitute for direct medical advice from your doctor or other qualified clinician. When you wake up in the morning, are you refreshed and ready to go, or groggy and grumpy?
For many people, the second scenario is all too common. Improving Sleep: A guide to a good night's rest describes the latest in sleep research, including information about the numerous health conditions and medications that can interfere with normal sleep, as well as prescription and over-the-counter medications used to treat sleep disorders.
Thanks for visiting. Don't miss your FREE gift. The Best Diets for Cognitive Fitness , is yours absolutely FREE when you sign up to receive Health Alerts from Harvard Medical School.
Sign up to get tips for living a healthy lifestyle, with ways to fight inflammation and improve cognitive health , plus the latest advances in preventative medicine, diet and exercise , pain relief, blood pressure and cholesterol management, and more.
Get helpful tips and guidance for everything from fighting inflammation to finding the best diets for weight loss from exercises to build a stronger core to advice on treating cataracts. PLUS, the latest news on medical advances and breakthroughs from Harvard Medical School experts.
Sign up now and get a FREE copy of the Best Diets for Cognitive Fitness. Stay on top of latest health news from Harvard Medical School. SCN transplantation into SCN-ablated hamsters confirmed their control of circadian rhythm period 37 and by encasing the SCN in semipermeable membranes that prevented synaptogenesis, the SCN were shown to produce diffusible signals sufficient to restore circadian activity rhythms Several of these SCN secretions have since been identified 39 — Temporal control of physiology.
Light exposure provides the primary time cue for the central clock in the suprachiasmatic nuclei SCN of the hypothalamus and suppresses melatonin synthesis by the pineal gland. Artificial light exposure at night can therefore disrupt the SCN clock and melatonin rhythm.
As a diurnal species, melatonin is hypnogenic in humans, although a recent prospective study of pinealectomy demonstrated that endogenous melatonin may not have a strong regulatory role in sleep Within the hypothalamus—a nodal point of body temperature regulation—the SCN influences the circadian rhythm of body temperature, a key synchronizer of clocks in peripheral tissues.
The use of thermostats can obviate daily oscillations in temperature, which could perhaps influence some circadian rhythms. In addition to temperature mechanisms, the SCN influences clocks in peripheral tissues through neural signals communicated via the autonomic nervous system ANS , as well as the timely secretion of signaling factors such as prokineticin 2.
Hypothalamic-pituitary-peripheral organ axes are important to hormonal regulation of the circadian system. For example, corticotropin-releasing hormone CRH enters the portal system through the median eminence ME of the hypothalamus and stimulates the secretion of adrenocorticotropic hormone ACTH by the anterior pituitary gland.
ACTH then regulates adrenal cortex production of cortisol, a hormone with a robust circadian oscillation and important synchronizing effects in many peripheral clocks.
The timing of metabolic processes in peripheral clocks is also modified by nutritional status, and peripheral clocks relay metabolic information back to the hypothalamus through the ME.
The foremost zeitgeber that entrains the SCN to the hour day is the LD cycle, and together with rod and cone photoreceptor cells, melanopsin-containing intrinsically photosensitive retinal ganglion cells in the inner retinae relay photic information to the SCN via a monosynaptic pathway to permit synchronization In response to photic stimuli, a multisynaptic pathway from the SCN to adrenergic fibers innervating the pineal gland regulates norepinephrine release from these fibers and hence melatonin synthesis 44 , Melatonin conveys photoperiodic information to the pituitary pars tuberalis , a key nexus in the regulation of seasonal rhythms in physiology in photoperiodic mammals, which undergoes seasonal body mass and reproductive changes 46 , Although the human melatonin rhythm is also sensitive to photoperiod changes 48 , the presence of artificial lighting suppresses seasonal changes in circadian rhythms such as melatonin that might otherwise be evident Because the SCN also have the melatonin receptors MT 1 and MT 2 50 , 51 MTNR1A and MTNR1B in humans, respectively , melatonin feeds back to the master clock.
In , Borbély 53 proposed a two-process model of sleep regulation in which a circadian process also interacts with a homeostatic process to regulate sleep. The circadian process influences alertness, and the sleep process is hypnogenic, rising during wakefulness and falling during sleep in a manner akin to an hourglass timer.
Immediate early genes in the SCN respond to light exposure, including clock genes 55 , the genes that generate approximately hour gene transcription rhythms. The positive arm of the core clock loop comprises the basic helix-loop-helix transcription factors circadian locomotor output cycles kaput CLOCK and brain and muscle aryl hydrocarbon receptor nuclear translocator-like 1 BMAL1.
In tissues such as the vasculature, CLOCK's functions are replaced by its paralogue neuronal period-aryl hydrocarbon receptor nuclear translocator single-minded protein 2 NPAS2.
Contrary to prior findings, it was recently shown that loss of CLOCK does not produce arrhythmicity in peripheral cells; rather, it appears that these cells only become arrhythmic when Npas2 is knocked down in the presence of CLOCK deficiency 56 , indicating a more prominent role of NPAS2 in the molecular clock than previously thought.
CLOCK and BMAL1 heterodimerize to activate transcription of clock-controlled genes CCGs. CCGs include the negative limb of the clock, namely cryptochrome CRY 1—2 and period PER 1—3 proteins. These then accumulate in the cytosol, multimerize, translocate into the nucleus, repress CLOCK-BMAL1 transactivating function, and terminate CRY1—2 and PER1—3 transcription.
CLOCK-BMAL1 inhibition ends, thus closing the negative feedback loop. At least five auxiliary feedback loops add robustness and couple the molecular clock to metabolic status Antiphasic to the core loop, the best characterized of these modulates BMAL1 transcription: RAR-related orphan receptor α activates BMAL1 transcription, and reverse-erythroblastosis REV-ERB α and REV-ERBβ repress BMAL1 transcription.
The rhythmic transcription of clock genes persists even in cultured fibroblast cells 58 , and because fibroblast gene expression periods may be consistent with whole-body circadian rhythm periods 59 , clock genes may be key determinants of circadian period and hence chronotype and sleep phenotypes.
This is supported by recent genome-wide association GWA studies that have linked genetic loci near established components of the molecular clock with chronotype 60 , Nevertheless, not all studies have found that in vitro fibroblast period duration is correlated with in vivo period In adulthood, circadian period advances with increasing age, but a difference in in vitro fibroblast period has not always been found between young and elderly individuals.
In the presence of sera from the elderly participants, however, fibroblast period was reduced in comparison to treatment with sera from the young adults, suggesting that circulating factors are also determinants of oscillator periods and perhaps chronotype Interestingly, although sleep timing advances with age in adulthood, changes in body temperature rhythm periods are not so clear 64 , Because the body temperature rhythm is partly regulated by the SCN, it is plausible that humoral factors influence circadian oscillations in some peripheral cells but not the SCN, although this hypothesis requires testing.
Clock genes regulate the transcription of CCGs, hundreds of which control the timing of tissue-specific functions Although some genes may be rhythmic in multiple tissues, their phases often differ between and even within tissues, and rhythmic gene expression is largely organ-specific 68 , Our understanding of the range of healthy phase relationships between these systems is poorly characterized, however.
Target genes of circadian clock genes are enriched for metabolic pathways, and metabolic genes that are direct targets of CLOCK-BMAL1 heterodimer also feedback to molecular clock components. These metabolic genes include D-box binding PAR bZIP transcription factor, differentiated embryo-chondrocyte expressed genes 1 and 2, estrogen-related receptor α, nicotinamide phosphoribosyltransferase, peroxisome proliferator-activated receptor α, and proper homeobox 1 It is important to note that because the metabolic state of the cell is coupled to the molecular clock 70 , the pervasiveness of rhythmic cellular activities is modified by factors such as diet.
This pathway is coupled to the molecular clock by phosphorylation of glycogen synthase kinase 3β, which in turn regulates PER stability, and hence period length Furthermore, SIRT1 and SIRT6 have particularly pivotal roles in the temporal control of metabolism by controlling chromatin modifications and hence the rhythmic transcription of distinct sets of genes in the liver, with SIRT1 primarily regulating genes involved in peptide and cofactor metabolism, and SIRT6 influencing genes integral to carbohydrate and lipid metabolism Finally, although there is contention regarding whether humans are seasonally photoperiodic 74 , daily gene expression rhythms occur within the context of seasonal changes in expression of protein-coding genes.
Seasonal gene expression changes have been shown in independent populations and are linked to changes in the cellular composition of blood. Seasonal gene expression fluctuations may underlie changes in immune function, and seasonal variations in expression profiles of metabolic genes in adipocytes are also apparent Because the incidences of some cardiometabolic diseases oscillate seasonally 76 , 77 , these findings may have implications for understanding and treating such pathologies; however, seasonal changes in disease risk may also be related to myriad other factors, including changes in health behaviors and environmental temperature.
Within a species, similar proportions of the transcriptome, proteome and metabolome oscillate with 24 hour profiles 78 — Although there are mostly minimal delays between gene transcription and translation, it has been shown using a human cell model that some arrhythmic gene transcripts produce rhythmic products via daily translation profiles Delays between gene transcription and translation vary across the day, partly due to RNA-binding proteins which modify processes such as pre-mRNA splicing, polyadenylation and RNA decay 82 , Post-translational clock protein modifications include acetylation, O-GlcNAcylation, poly-ADP ribosylation, phosphorylation, SUMOylation, and ubiquitination 84 — Non-coding RNA expression also fluctuates in similar proportions to protein-coding gene transcripts, conferring another level of post-transcriptional regulation, and therefore non-coding RNAs likely influence molecular clock regulation Collectively, such post-transcriptional processes contribute to appropriate, tissue-specific responses of peripheral clocks.
Non-transcriptional oscillations in peroxiredoxins, redox-sensitive antioxidant proteins involved in electron transfer, respond to oxidation in cells such as erythrocytes These oscillations persist in the absence of zeitgebers, and are temperature-compensated and entrainable. They are sustained in the absence of clock gene expression feedback loops and are the most highly conserved clocks known 91 , Their integration with the circadian system, sleep homeostasis, and metabolic networks is little understood, however.
Clock gene expression rhythms have divergent periods that do not resonate without synchronizing agents Disruption of the SCN clock dampens and desynchronizes peripheral tissue circadian rhythms 94 , and uncoupling of appropriate phase relationships between endogenous rhythms internal desynchronization is hypothesized to contribute to the deleterious metabolic effects of circadian rhythm disruption.
The SCN synchronize circadian rhythms by autonomic, behavioral, humoral, and temperature mechanisms. The former comprise caudal efferents to the subparaventricular zone and dorsomedial nucleus, dorsal efferents to the midline thalamic nuclei, and rostral efferents to the anterior hypothalamus and preoptic area The paraventricular nucleus is particularly important in the regulation of circadian rhythms in activity, autonomic processes, and secretion of hormones including melatonin and cortisol Multisynaptic efferents from the SCN to the periphery help regulate the availability of nutrients like glucose in the blood 97 , as well as hormone secretion rhythms by organs including the adrenal glands, adipose tissue, pancreas, and thyroid gland 98 — In turn, humoral factors from the periphery relay information back to hypothalamic regions via the hypothalamic median eminence Some clock genes are directly regulated by glucocorticoids via glucocorticoid response elements The strength of effects of glucocorticoids on peripheral clock rhythms differs between tissues; the kidneys and lungs, for example, are yet more responsive to glucocorticoids than the liver, which is more entrained by feeding As homeothermic vertebrates, humans are resistant to temperature entrainment by the environment, and experiments in mice tissues have shown that the SCN are responsible for this resistance Although thermoregulation is regulated by the interaction of many structures located primarily in the hypothalamus, brainstem, and spinal cord, the SCN are integral to the core body temperature rhythm, a rhythm that has important synchronizing effects on oscillators throughout the body Furthermore, a specific component of the molecular clock has been identified as a key connection between the circadian and thermoregulatory systems because deletion of Rev-erb α in mice abolishes the core body temperature rhythm by changing brown adipose tissue activity Internal synchrony temporally partitions physiology to aid physical activity and energy harvesting during the biological day active phase , inactivity and energy mobilization during the rest phase, and time-of-day appropriate changes in immune function , Clock-regulated changes in blood pressure, heart rate, and skeletal and heart muscle contractile efficiency and substrate oxidation ready the body for physical activity — As a result, the circadian system ensures peak physical performance during the active phase.
Historically, physical activity has been necessary to procure food, and during the active phase, rhythms in the gastrointestinal system support timely digestion. Gastric emptying and colonic motility, for example, are slowest in the evening, and the transit of indigestible food from the stomach to the small intestine is powered by the migrating motor complex, the speed of which is more than twice as high during the day as at night — Rhythmic bile acid production is central to cholesterol metabolism and absorption of nutrients, including fat-soluble vitamins.
Kruppel-like factor 15 and fibroblast growth factor 15 have pivotal roles in this regulation Rhythmic changes in the activity of some intestinal nutrient transport proteins and temporal control of enzyme activity are also important to metabolism. Using lipids to exemplify this, reduced postprandial lipoprotein lipase activity apparently contributes to impaired lipid tolerance in the evening It should be noted that it is unclear whether the aforementioned gastrointestinal rhythms are partly clock-regulated or exclusively artifacts of behavioral cycles.
Other enzymes involved in hepatic lipid metabolism are known targets of the molecular clock and shape rhythms in processes like lipid accumulation Nocturnin, for example, is clock-controlled and regulates triacylglycerol synthesis and storage, as well as chylomicron formation in intestinal enterocytes Gut microbiota composition changes with feeding and fulfils time of day-specific functions in humans and mice, with energy metabolism roles during the active phase and detoxification processes during the rest phase Reciprocity between the circadian system and microbiota is evident because Bmal1 deletion nullifies these oscillations Furthermore, clock gene expression is altered in germ-free mice, and these mice do not gain body mass compared to conventionally raised mice, perhaps due to differences in microbe-derived metabolites like short-chain fatty acids Whereas it is unclear whether rhythmic secretion of several gastrointestinal hormones is shaped by the circadian system such as gastric inhibitory polypeptide, gastrin, and glucagon-like peptide-1 , , other hormones are demonstrably clock-regulated.
Constant routine and forced desynchrony experiments have shown that plasma glucose and triacylglycerol have clear circadian rhythms, with an acrophase in the biological night — , indicating circadian system regulation of energy substrate metabolism.
This is likely related to circadian rhythms in important hormones in energy metabolism, such as insulin. Insulinemia, like insulin sensitivity, peaks in the daytime in humans to promote efficient energy storage , and an acrophase in the insulin-sensitizing adipokine adiponectin in the middle of the active phase supports this process Rhythmic growth hormone GH secretion is another important determinant of daily changes in substrate oxidation.
Although a minor influence of the circadian system has sometimes been detected, sleep has a dominant influence on GH secretion 5. GH has an acrophase near the onset of slow wave sleep SWS , and GH profiles are further characterized by episodic surges a few hours after meals , The GH rhythm differs a little between the sexes Together with insulin and insulin-like growth factor 1 IGF-1 , GH aids nitrogen retention during high energy availability; during reduced energy availability, as occurs during sleep, GH stimulates lipolysis and ketogenesis , inducing insulin resistance and thereby sparing glucose and protein oxidation Prolactin also influences appetite in a species-specific way, and chronic hyperprolactinemia is associated with increased body mass in humans.
Furthermore, prolactin has roles in lipid metabolism, largely reducing lipid storage in adipocytes, and also affects glucose metabolism by stimulating insulin secretion A circadian rhythm in prolactin is evident in constant routine protocols, of larger amplitude in women and with an acrophase in the rest phase Subcutaneous prolactin injections prolong rapid eye movement sleep in rats , and prolactin is also associated with SWS in humans Melatonin synthesis occurs during darkness and increases sleep propensity in humans, which may be related to melatonin's hypothermic effects Melatonin may have important roles in metabolic regulation, perhaps helping prevent nocturnal hypoglycemia by inhibiting insulin secretion Because this was demonstrated in mice, however, different responses may be apparent in humans.
Interestingly, the MTNR1B T2DM risk variant rs — has been linked to prolonged melatonin synthesis duration and delayed melatonin offset phase in humans. Because melatonin inhibits glucose-stimulated insulin secretion ex vivo, it is plausible that extended melatonin synthesis into waking could contribute to T2DM risk, particularly among carriers with early sleep times As melatonin also exerts receptor-independent effects in free radical scavenging , melatonin perhaps also contributes to temporal regulation of immune function, although further research is required.
Finally, an acrophase in leptin secretion during the rest phase may contribute to reduced appetite for most foodstuffs in the biological morning in humans, permitting consolidated sleep despite declining energy availability This hypothesis is not supported by the finding that nocturnal rats also have an acrophase in leptin secretion during darkness their active phase , although it is possible that leptin has different roles in diurnal and nocturnal species.
Sleep restriction is ubiquitous, and its metabolic consequences are profound. One of the best-characterized metabolic sequelae of sleep disruption is disrupted glucose metabolism.
Altered hour endocrine profiles were also evident because TSH secretion was impaired and nocturnal cortisol secretion increased This finding of abnormal glucose metabolism has been consistently replicated, and much progress has been made in understanding the contributing mechanisms Figure 2.
Mechanisms linking circadian system and sleep disruption to hyperglycemia, insulin resistance, and obesity. With further research, mechanisms that are currently listed as distinct may prove to be common. In the postprandial state, the brain accounts for roughly half of whole-body glucose disposal, and sleep deprivation reduces this use Cephalic phase neurogenic signals from the brain anticipate food consumption and stimulate insulin secretion.
Insulin resistance after sleep restriction is not associated with altered cephalic phase insulin secretion but rather appears to result primarily from insulin resistance outside the liver , and changes in adipose tissue insulin signaling may be particularly important Given the roles of the molecular clock in glucose and lipid metabolism, reduced glucose tolerance and metabolic dysregulation after sleep disruption may also be related to epigenetic and transcriptional changes in the molecular clock in peripheral tissues important to glucose disposal, including adipose tissue and skeletal muscle.
Indeed, there is increased DNA methylation of the promoter region of CRY1 and two regions near PER1 in adipocytes, as well as reduced BMAL1 and CRY1 transcription in myocytes after sleep deprivation Consistent with Randle's glucose fatty-acid cycle , increased release of nonesterified fatty acids from adipocytes after sleep restriction likely also contributes to insulin resistance Further mechanisms reducing insulin sensitivity after sleep disruption include stimulation of gluconeogenesis via increased sympathetic activity of the autonomic nervous system and a shift in cytokine balance toward a more inflammatory state Related to this, sleep curtailment affects numerous aspects of immune function.
For example, 1 week of sleep restriction in men increased circulating white blood cells and changed their diurnal rhythm.
Notably, altered cell counts had not returned to baseline after 9 days of recovery sleep Such changes in immune function may contribute to the development of diseases associated with immune system changes, such as T2DM It has also been shown that changes in sleep architecture during sleep disruption contribute to changes in glucose metabolism.
Indeed, restricting sleep to the first half of the night produces distinct endocrine effects compared to restriction to the second half , and different sleep stages produce distinct physiological changes. Selective SWS restriction, for example, reduces insulin sensitivity in a dose-response manner in adults, independent of sleep duration, although adolescents may be more resistant to this effect , Intravenous insulin sensitivity was not restored by 3 days of recovery sleep; notably, 3 days is longer than most working adults have to catch up on sleep each week.
A limitation of most experimental sleep restriction studies is that they often enforce large changes in sleep duration, but restriction by 90 minutes per night—an amount similar to that experienced by many 18 —has also been shown to reduce insulin sensitivity after 1 week in young men In this healthy population, impaired insulin sensitivity dissipated with continued exposure to such restriction.
A detailed review of obstructive sleep apnea OSA is beyond the scope of this review. However, because studies have consistently shown that OSA is associated with impaired insulin and glucose metabolism, its features are briefly outlined.
OSA is a disorder in which individuals experience episodic upper airway closure and hence intermittent hypoxia during sleep. OSA is further characterized by reduced sleep duration, sleep fragmentation, reduced SWS, and increased sympathetic nervous system activity and oxidative stress, all of which can contribute to insulin resistance Although obesity increases the risk of OSA and is itself associated with insulin resistance, insulin resistance in OSA has been shown to be independent of adiposity Furthermore, OSA is highly prevalent in people with T2DM , and a meta-analysis has shown that OSA is a strong risk factor for T2DM development Pregnancy also predisposes women to OSA and may worsen maternal glucose metabolism and hence increase the risk of gestational diabetes Continuous positive airway pressure is used to treat OSA; whether it improves glucose metabolism is contentious, but accumulating evidence suggests that it may We would also be remiss if we did not mention that the metabolic consequences of insomnia have not been thoroughly studied, despite it being the most common sleep disorder.
Because sleep state misperception the mistaken perception of wakefulness during sleep is common in insomnia, it will be important to measure sleep objectively in these studies. Although conflicting evidence exists , a meta-analysis of sleep restriction studies showed that sleep restriction increases energy intakes in adults, contributing to its obesogenic effects This finding is consistent with an extended period in which food can be consumed to compensate for the additional energetic cost of wakefulness.
Sleep restriction also increases energy intakes and the appeal and consumption of desserts among adolescents , and sleep deprivation has even been shown to increase the energy content and mass of food purchased per unit of money in a mock supermarket In light of these findings, it might be expected that sleep restriction influences satiety hormones, of which the best-studied are ghrelin and leptin.
During ad libitum food availability, however, documented effects of sleep restriction on ghrelin and leptin are contradictory , , With that said, sleep restriction does appear to increase ghrelin concentrations and hunger in adults consuming standardized hypoenergetic diets and after sleep restriction, ghrelin is subsequently positively correlated with energy intake when eating ad libitum It is important to consider that a multitude of hormones influence feeding behavior, and it was recently shown that sleep restriction increases plasma concentrations of the orexigenic endocannabinoids 2-arachidonoylglycerol and 2-oleoylglycerol, perhaps also contributing to increased energy intakes The energy expenditure side of energy balance may also be affected by sleep restriction, as a working week sleep restriction simulation study showed that sleep restriction reduces resting metabolic rate RMR , particularly among African Americans—a population highly susceptible to the obesogenic effects of sleep restriction.
Notably, this effect was seen despite participants being in positive energy balance, which might be expected to have raised their RMRs Lean body mass is a key determinant of RMR, and sleep restriction during hypoenergetic diet consumption accelerates lean body mass losses and impairs reductions in adiposity, providing a mechanism by which chronic sleep disruption could detrimentally influence body composition The importance of adequate sleep during energy restriction is supported by the finding that longer sleep predicts greater reductions in BMI in overweight and obese adults consuming hypoenergetic diets Interestingly, within-participant effects of one night of sleep restriction on energy intake and body mass changes appear stable when repeated exposures are separated by long periods of time, particularly among men, suggesting trait-like responses to sleep disruption.
Some gene variants, like the YH variant of basic helix-loop helix family member e41, have been shown to confer carriers with resistance to other effects of sleep deprivation, such as less need for recovery sleep ; perhaps biomarkers that influence resistance to the metabolic sequelae of sleep disruption will also be identified.
Tremendous advances have been made in various omics techniques in recent years, including genomics, transcriptomics, proteomics, and metabolomics.
Studies applying metabolomics, proteomics, and transcriptomics continue to unveil new insights into sleep and the circadian regulation of metabolism. Interestingly, there is large heterogeneity among healthy adults, and different lipid metabolic phenotypes have been identified In saliva, amino acids and associated metabolites comprise over half of the oscillating metabolites Omics techniques have also been applied to the study of circadian rhythm and sleep disruption.
Sleep restriction primarily modifies lipid, neurotransmitter, oxidative stress, and gut metabolites , effects that may help explain increased cardiometabolic disease risk in sleep-restricted individuals Similarly, sleep deprivation alters rhythms in plasma metabolites including lipids and acylcarnitines, largely reducing the amplitude of metabolite rhythms in comparison to when sleep is permitted The extent of these changes can be explained by the diversity of changes that occur during sleep, including changes in physical activity, light exposure, redox state, and temperature, all of which influence numerous physiological processes.
Furthermore, complete ° circadian misalignment profoundly affects the human blood transcriptome, producing a 6-fold reduction in genes with hour expression profiles, an effect consistent with reduced core body temperature rhythm amplitudes The use of multiomics techniques has the potential to reveal novel insights into the systems-level regulation and integration of the circadian system and sleep homeostasis, in addition to identifying novel biomarkers of metabolic dysfunction and circadian system and sleep disruption.
There are conflicting findings regarding whether men and women differ in their energy balance responses to sleep disruption. A large study of five nights of sleep restriction 4 hours of time in bed found that men are predisposed to positive energy balances after sleep restriction ; however, a smaller, crossover study of five nights of sleep restriction 5 hours of time in bed in a more homogeneous group of younger adults indicated that women are more susceptible Further research is required to understand these discrepant findings.
Certainly, sex does influence certain responses to sleep restriction, as seen in menstrual cycle phase-dependent endocrine responses to sleep restriction , and there is a general need to clarify how the menstrual cycle influences responses to circadian rhythm and sleep disruption.
Finally, it is likely that changes in sleep architecture during sleep disruption influence eating behavior: The final rapid eye movement period, for example, is hypothesized to be protective against overeating Experiments should continue to assess associations between sleep architecture, behavior, and physiology.
It has been estimated that U. adults make approximately food-related decisions daily If sleep disruption adversely influences dietary choices, its deleterious metabolic effects could be compounded.
Although sleep restriction has sometimes been found to influence dietary macronutrient proportions, conflicting evidence exists Notably, macronutrient intakes depend on available foods, and limited snack options are available in experimental settings.
Rather than altering macronutrient preferences, recent brain imaging studies support the hypothesis that sleep disruption increases nonhomeostatic eating propensity.
Sleep restriction accentuates increased activity in brain regions involved in reward in response to food stimuli , suggesting heightened sensitivity to rewarding properties of food.
Brain activity changes after sleep deprivation are consistent with increased appetite , and activity in one of these regions, the nucleus accumbens, is particularly highly associated with energy-dense food selection Finally, accurate recollection of food consumption influences short-term food ingestion, an extreme example of which is seen in amnesiacs who will eat multiple meals consecutively Hippocampal changes after sleep deprivation contribute to memory impairments , and hippocampal activity helps prevent meal initiation in the postprandial period Although it is plausible that sleep disruption may increase food intake by influencing hippocampal activity, this hypothesis requires further testing.
Collectively, these studies suggest that experimental sleep restriction and deprivation induce a plethora of adverse metabolic consequences that may be accentuated by changes in food selection. Experimental sleep disruption is often more severe than that experienced outside the laboratory; therefore, studies of less marked sleep restriction and further field studies are needed.
Time spent outdoors in Canada, Great Britain, and the United States is commonly 1 to 3 hours daily — , depending on season and other factors, and compared to exposure to only natural light, individuals in modern societies are perhaps exposed to about four times less light during the day Consequently, many individuals, particularly those in urban populations, are sheltered from the diverse beneficial effects of natural daytime light on behavior and physiology Vitamin D is synthesized in response to UV-B irradiation, and indoor living in industrialized areas is one contributor to low vitamin D status.
Although consistent evidence linking vitamin D status to morbidity is contentious, associations with some health parameters exist It is well established that the LD cycle is the primary zeitgeber for humans; however, because vitamin D directly influences clock gene transcription in vitro , it is possible that some of the associations between vitamin D status and health may arise from effects of vitamin D status on circadian rhythms and sleep.
Negative associations between vitamin D status and sleep duration — and sleep efficiency , corroborate this contention; nevertheless, this may simply reflect beneficial effects of greater daytime light exposure on sleep rather than effects of vitamin D on the molecular clock.
This appears to significantly influence sleep. The introduction of electric lighting is associated with increased light exposure shortly after dusk during workdays, delayed sleep onset, and shortened sleep duration among individuals of the same sociocultural background.
These effects may be particularly prominent during workdays , Although the authors of a recent study of three hunter-gatherer communities living without electricity suggested that individuals living without artificial lighting may not sleep for longer than individuals with lighting , this suggestion was not supported by a comparison between the hunter-gatherer groups and individuals of similar ethnic origins with access to artificial lighting Many electronic devices also now increase nighttime light exposure.
Given their compactness, it might be expected that any effects of these devices on the circadian system and sleep would be benign. However, some of these devices emit monochromatic blue light λ max , — nm , to which intrinsically photosensitive retinal ganglion cells are especially sensitive.
As a result, nighttime exposure to even low levels of light from e-Book devices delays sleep and dim-light melatonin onset, reduces melatonin synthesis, and impairs next-morning alertness.
There are positive associations between nighttime illumination and obesity prevalence in more than 80 countries worldwide , and also between the mean timing of light exposure above lux and BMI in free-living adults Given the aforementioned discussion of the sleep-disrupting effects of light exposure, as well as the multitude of factors that conspire to increase energy balance after sleep disruption, it seems likely that increased light exposure at night is another contributor to the obesity epidemic.
Even when diet is controlled, night shift workers exhibit poorer metabolic health than day workers. Night workers, for example, have higher plasma triacylglycerol , and field work has shown that this is related to circadian system disruption because postprandial glucose and lipid tolerance to standard test meals are impaired on switching to night shifts Like metabolic health, cognitive function is frequently impaired by night shift work.
Transitioning from day to night shifts often entails sleep deprivation, and performance decrements during this time can be comparable to blood alcohol levels that exceed the legal driving limit An important determinant of shift work tolerance is entrainment to shift schedules.
Isolated environments can be more conducive to adaptation to shift work than more common shift working scenarios, and in circumstances such as workers experience on the British Antarctic base at Halley or on oil rigs, most workers can synchronize their circadian systems to night shifts within a week Even in these instances, however, it can take weeks for workers to re-entrain to day shifts — Workers who exclusively work night shifts might be expected to completely entrain their circadian systems to their work hours 6.
However, disrupted endocrine circadian rhythms persist even among adults who have worked night shifts for over 2 years. These chronic night shift workers have altered TSH profiles, and reduced cortisol secretion and increased prolactin secretion during their waking hours may impair vigilance Laboratory experiments have attempted to simulate shift work to clarify its metabolic consequences.
As discussed previously, it is apparent that sleep restriction reduces insulin sensitivity; however, circadian misalignment imposed by LD cycle shifts nearly doubles reductions in insulin sensitivity after sleep restriction alone in males, also furthering inflammation Some shift work simulation experiments have produced conflicting findings regarding several metabolic variables.
During 6 days of simulated night shift work in healthy adults, there was an initial increase in fat oxidation and a reduction in carbohydrate and protein oxidation. Diet-induced thermogenesis temporarily fell, and energy expenditure declined on the second and third days, particularly during sleep.
Paradoxically, appetite diminished despite reduced levels of the orexigenic hormones leptin and peptide tyrosine tyrosine However, in contrast to these findings, neither three consecutive 3-hour LD cycle advances nor three consecutive 3-hour LD cycle delays influenced appetite or energy expenditure in adults, and both shifts increased carbohydrate oxidation and reduced protein oxidation.
In this study, LD cycle advances acutely reduced cortisol rhythm amplitudes and increased insulinemia, whereas LD cycle delays increased glycemia, and decreased glucagon-like peptide-1 concentrations and sleeping energy expenditure Discrepancies between some of these findings likely reflect differences in experimental design, emphasizing the need to compare a variety of shift schedules when attempting to offset deleterious consequences of shift work.
Other circadian misalignment protocols have provided new insights into the short-term health consequences of shift work. Circadian misalignment increases blood pressure particularly during sleep and inflammatory markers, reverses cortisol rhythms, and reduces heart rate variability and insulin sensitivity in healthy adults , Furthermore, misalignment increases postprandial glycemia despite enhanced late-phase insulin secretion Prolonged circadian misalignment reduces cortisol secretion , and whereas acute circadian misalignment increases insulin secretion , 3 weeks of combined sleep restriction and circadian misalignment impairs insulin secretion, indicating pancreatic dysfunction An important question is whether chronic exposure to circadian rhythm and sleep disruption produces adaptations that mitigate the adverse effects of subsequent disruptions to the endocrine system.
It appears that this may not be the case, however, because healthy chronic shift workers are still subject to the deleterious effects of circadian misalignment on postprandial glucose tolerance and insulin action Collectively, these studies indicate possible mechanisms linking shift work to increased metabolic disease risk and show a need to optimize shift work schedules direction, duration, and frequency to minimize deleterious health effects.
In general, changing from backward to forward shift rotation, shifting from slow to fast shift rotation, and allowing self-scheduling of shifts appear to benefit the health and quality of life of shift workers Because individual tolerance to shift work varies widely , it will be important to find ways of determining those at highest risk of shift work-induced circadian rhythm and sleep disruption.
There is a need to study further how to optimize shift work schedules based on chronotype because observational evidence suggests that associations between shift work schedules and T2DM are related to chronotype , and manipulating shift work schedules based on chronotype can reduce circadian rhythm and sleep disruption Because the circadian system is intertwined with metabolic regulation, recent studies have focused on deciphering whether circadian system gene single-nucleotide polymorphisms SNPs are associated with metabolic health in adults.
Studies of clock gene disruption in other animals paved the way for these studies because whole-body and tissue-specific clock gene mutation and knockout models produce various feeding and metabolic aberrations in rodents , Perhaps the most severe example of this is the abolition of behavioral and molecular circadian rhythms in mice after Bmal1 knockout.
These animals also succumb to premature mortality In rare cases, genetic abnormalities produce developmental disorders that entail circadian system disorganization and metabolic dysfunction.
Retinoic acid induced 1 RAI1 transcriptionally regulates CLOCK , and haploinsufficiency of RAI1 is the primary contributor to the Smith-Magenis syndrome phenotype, a disorder characterized by circadian rhythm and sleep disruption, intellectual disability, and obesity GWA studies provide the strongest evidence for roles of more common circadian system gene variants in human metabolism and disease risk.
GWA studies have linked PER3 to T2DM and CRY2 with fasting glycemia and insulin concentrations In these studies, melatonin receptor 1B MTNR1B variants are also consistently associated with insulin secretion and T2DM risk — Less robust evidence for ties between circadian system gene variants and metabolism comes from candidate gene studies.
In adults, two BMAL1 haplotypes have been linked to hypertension and T2DM , CLOCK SNPs have been associated with nonalcoholic steatohepatitis, metabolic syndrome, small dense low-density lipoprotein levels, obesity, and T2DM — Perhaps the most studied of these associations is that of obesity; to date, eight common SNPs have been linked to obesity, and three have been associated with energy intakes An ultimate goal of candidate gene studies is to help personalize healthcare.
A recent meta-analysis of up to 28 participants from 15 cohort studies sought to identify whether nutrition and sleep modify associations between select circadian system gene variants and cardiometabolic traits.
Carbohydrate intake was positively associated with fasting glycemia in the presence of the T allele of MTNR1B rs Finally, sleep duration was positively associated with high-density lipoprotein cholesterol among carriers of the A allele of CRY2 -rs CLOCK , CRY , and REV-ERB α variants were not found to interact with nutrition to influence cardiometabolic health, however.
Collectively, SNP studies suggest that the knowledge of circadian gene SNPs may eventually help identify those at greatest risk of some diseases and personalize interventions. However, candidate gene studies are limited by their sample sizes, their exclusion of all causative genes and gene variants, and their limited replicability.
Hence, such studies need replicating in larger, unbiased GWA studies. Several interventions have promise in mitigating the metabolic consequences of circadian rhythm and sleep disruption Figure 2.
It is important to note that circadian rhythm and sleep disruption can have distinct effects, and sleep timing per se has but small effects on the circadian system phase ; it is perhaps changes in light exposure during sleep because of the closing of the eyes that is likely to have the strongest effect on the circadian system.
Nevertheless, the homeostatic regulation of sleep is intertwined with the circadian pacemaker in the SCN, so strategies to counter each should consider this interaction, and interventions should be tailored to individual circumstances.
In the case of sleep restriction, sleep extension appears to benefit many aspects of metabolic health. Among short-sleeping adults, increased time in bed after a sleep extension intervention is associated with improvements in glucose regulation and insulin sensitivity , and as little as 3 days of sleep extension may benefit insulin metabolism and increase testosterone in habitually short-sleeping men.
Interestingly, sleep extension reduced the anorexigenic peptide hormones leptin and peptide tyrosine tyrosine, although effects on food intake were not assessed Sleep extension may also improve body composition.
Indeed, increased sleep duration is prospectively associated with attenuated increases in adiposity in short-sleepers , and findings from a study of overweight, habitually short-sleeping young adults suggest that this may be related to increased energy expenditure.
Among these individuals, 2 weeks of 2-hours of increased time in bed in home environments increased sleep duration and daytime energy expenditure, and reduced appetite and the desire for highly palatable foods One factor that may influence the effects of sleep extension interventions on dietary habits is chronotype.
Using a crossover design to change the time at which adolescents went to bed and thereby compare a 6. Hence, there is a need to study further the influence of chronotype on appropriate bedtime recommendations. Finally, sleep extension may benefit other behaviors. A systematic review of naturalistic studies recently found that delaying school start times increases students' sleep durations, and there was some evidence for concomitant improvements in behavior and affect Improvements in sleep hygiene are a natural starting point in attempts to achieve better sleep, and further research on optimizing such variables as sound, bedding, mattresses, and temperature may benefit sleep.
Pharmaceutical chronobiotics have potential in countering circadian rhythm disruption. For example, pharmaceutical inhibition of CK1 helps synchronize misaligned oscillators and hence speeds adaptation to LD cycle shifts in mice , , as can therapeutic SCN neuropeptide modulation Furthermore, an array of clock-enhancing small molecules may ultimately provide effective therapies for disorders of the circadian system Intriguingly, a circadian clock was recently transplanted into a noncircadian organism for the first time, and such methods could have chronotherapeutic applications, such as regulation of timely drug release This is particularly pertinent given that most of the highest-selling drugs target the products of rhythmically transcribed genes Of note, pharmaceutical chronobiotics may also benefit metabolic health.
REV-ERB agonists, for example, diminish adiposity, hyperglycemia, and hyperlipidemia in diet-induced obese mice However, none of these compounds has yet been tested for safety or efficacy in humans. Other well-established therapies like melatonin should be further studied for effects on food selection and metabolism in humans.
Interestingly, 1 year of melatonin supplementation was recently shown to increase lean body mass and reduce fat mass in postmenopausal women with osteopenia , and daily ingestion of prolonged-release melatonin reduced glycosylated hemoglobin in individuals with insomnia and T2DM Finally, caffeine, the most commonly consumed psychoactive substance worldwide, changes the period of both the molecular clock in vitro and the melatonin rhythm in humans, and timely caffeine ingestion may therefore help entrainment in such circumstances as jetlag , Nonpharmaceutical interventions are also capable of improving circadian system function and sleep, including blue-blocking glasses and apps to filter short-wavelength emissions from electronic devices , Because the brightness, color, duration, and timing of light exposure influence many physiological functions — , it is feasible that these interventions could influence the phase of the SCN and numerous other processes independent of the SCN, including activity in other brain regions and endocrine networks that help regulate appetite.
In a similar vein, consideration should be given to light exposure when designing buildings and their windows. The timing, composition, and quantities of foods ingested influence the circadian system , as exemplified by the restoration of behavioral and physiological rhythms in SCN-ablated rats by a single, timed, hypoenergetic daily meal Because the molecular clock is intertwined with the metabolic state of the cellular environment, TRF to the rest phase can invert clock gene rhythms in many peripheral tissues When TRF is imposed with ad libitum food availability in mice, SCN gene expression rhythms are similar to those without TRF, and TRF can therefore change the phase relationships between gene expression rhythms in peripheral tissues and the SCN.
Hypoenergetic diets, however, can phase-shift peripheral tissue gene expression profiles and also have a small influence on SCN gene expression rhythms Whether similar effects of TRF schedules are evident in humans is currently unclear; if evident, TRF may too be a useful strategy in situations where resynchronization with the external environment is desired.
TRF produces an array of metabolic health benefits in various animals , but little research has explored whether this is true of humans. Furthermore, there is some evidence that the timing of food intake may influence the effectiveness of weight loss interventions because greater energy intake earlier in the day has been associated with greater weight loss in prospective studies of overweight and obese adults , Finally, reciprocity between physical activity and the circadian system exists because both experimental circadian rhythm disruption and diseases associated with SCN dysfunction disrupt physical activity patterns , , and physical activity influences melatonin rhythms a little, as well as peripheral tissue gene expression rhythms , Furthermore, the circadian system regulates autonomic control of cardiovascular responses to exercise, resulting in peak cardiac vagal tone withdrawal in the morning, and a bimodal acrophase in epinephrine and norepinephrine reactivity to exercise in both the morning and evening, perhaps helping to explain the increased risk of cardiovascular events at these times The extent to which the beneficial metabolic effects of exercise are mediated by the circadian system is unclear; regardless, the health-promoting effects of exercise are extensive.
Most human circadian rhythm and sleep disruption experiments to date have enforced minimal physical activity. Rodent studies suggest that physical activity offsets some adverse metabolic effects of light exposure at night Exercise may also offset some of the deleterious effects of sleep disruption because resistance training attenuates the catabolic effects of sleep deprivation on lean body mass in rats, perhaps by offsetting changes in testosterone, IGF-1, and corticosterone Because there is a paucity of human studies on the subject, it will be important to study how to optimize exercise protocols to mitigate metabolic dysfunction induced by circadian rhythm and sleep disruption.
In modern societies, circadian rhythm and sleep disruption are perhaps more pervasive than ever. There is increasing evidence of detrimental effects on metabolic function and dietary choices, emphasizing the importance of bolstering circadian system function and addressing sleep disruption.
Because an appreciation of the importance of circadian system entrainment and sleep may significantly enhance health and productivity for many individuals, educating key personnel has great potential to benefit society.
The circadian system optimizes behavior and physiology according to the time of day and is organized in a hierarchical manner with a central clock in the SCN that is primarily entrained by light.
Nowadays, we are commonly exposed to less light during the day and more light at night because of artificial lighting, which may impair circadian system organization and disrupt sleep, resulting in widespread adverse effects on metabolic health. Disrupted sleep, for example, promotes increased energy intake, reduced energy expenditure, and insulin resistance in many individuals, consequences that may be compounded by an increased propensity to make less healthy dietary choices.
Careful experiments have also shown that circadian misalignment produces an array of metabolic abnormalities. Future research should continue to study factors influencing individual variation in the risk of and responses to circadian rhythm and sleep disruption, such as sex differences in circadian rhythms , associations between ethnicity and sleep variability , and other factors that contribute to differences in metabolic and behavioral responses to circadian rhythm and sleep disruption between individuals.
It may not always be possible to extrapolate findings from animal studies to humans , indicating a need for continued human research, especially in populations experiencing frequent circadian rhythm and sleep disruption. Furthermore, little research has explored such disruption in diseases like T2DM.
There has also been little research on large populations likely experiencing circadian rhythm and sleep disruption. People living in China, for example, may be of particular interest because the country spans five geographical time zones, yet the entire nation follows Beijing time.
It is plausible that chronic circadian rhythm and sleep disruption may incur some adaptations in the affected, although little research has addressed this to date. Finally, behavioral and pharmaceutical interventions show promise in offsetting the adverse effects of circadian rhythm and sleep disruption.
Some of the beneficial effects of these interventions may be independent of the circadian system and sleep, however. Because our understanding of the range of healthy phase relationships between the SCN and peripheral clock systems is poorly characterized, clarifying these relationships could help personalize prescription of chronobiotics, some of which still require human safety and efficacy studies.
Thereafter, comparisons of these interventions are needed to evaluate which are most effective and in what circumstances. Ultimately, we hope that mankind's historic fascination with the temporal world will continue to draw interest to the importance of the human timing system in all facets of health.
thanks the Medical Research Council for his Doctoral Training Grant. and L. thank the Medical Research Council for support Grant No. As a Wolfson Research Merit Award holder, D. acknowledges the Royal Society. Some of D. and P. Disclosure Summary: G.
have nothing to declare. and J. are co-directors of Stockgrand Ltd. neuronal period-aryl hydrocarbon receptor nuclear translocator single-minded protein 2.
Halberg F. Physiologic hour periodicity; general and procedural considerations with reference to the adrenal cycle [in German].
Int Z Vitaminforsch Beih. Google Scholar. Pittendrigh CS. On temperature independence in the clock system controlling emergence time in Drosophila. Proc Natl Acad Sci USA. Aschoff J , Klotter K , Wever RA. Circadian clocks. In: Aschoff J , ed. Proceedings of the Feldafing Summer School , September Amsterdam, The Netherlands : North Holland Publishing Co.
Czeisler CA , Duffy JF , Shanahan TL , et al. Stability, precision, and nearhour period of the human circadian pacemaker. Middleton B , Arendt J , Stone BM. Human circadian rhythms in constant dim light 8 lux with knowledge of clock time.
J Sleep Res. Folkard S. Do permanent night workers show circadian adjustment? A review based on the endogenous melatonin rhythm. Chronobiol Int. Arendt J , Middleton B , Williams P , Francis G , Luke C. Sleep and circadian phase in a ship's crew. J Biol Rhythms.
Axelsson J , Akerstedt T , Kecklund G , Lowden A. Tolerance to shift work-how does it relate to sleep and wakefulness? Int Arch Occup Environ Health. Arendt J.
Shift work: coping with the biological clock. Occup Med Lond. Knutsson A , Bøggild H. Gastrointestinal disorders among shift workers. Scand J Work Environ Health. Wang F , Yeung KL , Chan WC , et al. A meta-analysis on dose-response relationship between night shift work and the risk of breast cancer.
Ann Oncol. Wang F , Zhang L , Zhang Y , et al. Meta-analysis on night shift work and risk of metabolic syndrome. Obes Rev. Schiavo-Cardozo D , Lima MM , Pareja JC , Geloneze B. Appetite-regulating hormones from the upper gut: disrupted control of xenin and ghrelin in night workers.
Clin Endocrinol Oxf. Parent-Thirion A , Vermeylen G , Lyly-Yrjänäinen Maija , Biletta I , Cabrita J. Fifth European Working Conditions Survey—Overview Report. Dublin, Ireland : European Foundation for the Improvement of Living and Working Conditions ; ; 1 — Bureau of Labor Statistics.
Workers on flexible and shift schedules in May Washington, DC : US Department of Labor ; Hammer GP , Auvinen A , De Stavola BL , et al. Mortality from cancer and other causes in commercial airline crews: a joint analysis of cohorts from 10 countries.
Occup Environ Med. Annual Review In: Program of the 69th Annual General Meeting of the International Air Transport Association ; June ; Cape Town, South Africa.
Roenneberg T , Allebrandt KV , Merrow M , Vetter C. Social jetlag and obesity. Curr Biol. Wittmann M , Dinich J , Merrow M , Roenneberg T.
Social jetlag: misalignment of biological and social time. Kim M , Sasai H , Kojima N , Kim H. Objectively measured night-to-night sleep variations are associated with body composition in very elderly women.
Wong PM , Hasler BP , Kamarck TW , Muldoon MF , Manuck SB. Social jetlag, chronotype, and cardiometabolic risk. J Clin Endocrinol Metab. Taylor BJ , Matthews KA , Hasler BP , et al.
Bedtime variability and metabolic health in midlife women: the SWAN Sleep Study. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. Ford ES , Li C , Wheaton AG , Chapman DP , Perry GS , Croft JB.
Sleep duration and body mass index and waist circumference among U. Obesity Silver Spring. Habitual sleep duration and risk of childhood obesity: systematic review and dose-response meta-analysis of prospective cohort studies. Sci Rep. Sperry SD , Scully ID , Gramzow RH , Jorgensen RS.
Sleep duration and waist circumference in adults: a meta-analysis. Bei B , Allen NB , Nicholas CL , Dudgeon P , Murray G , Trinder J. Actigraphy-assessed sleep during school and vacation periods: a naturalistic study of restricted and extended sleep opportunities in adolescents.
Krueger PM , Reither EN , Peppard PE , Burger AE , Hale L. Cumulative exposure to short sleep and body mass outcomes: a prospective study. Goel N , Stunkard AJ , Rogers NL , et al. Circadian rhythm profiles in women with night eating syndrome. Biological rhythms during residence in polar regions.
Lockley SW , Skene DJ , Arendt J , Tabandeh H , Bird AC , Defrance R. Relationship between melatonin rhythms and visual loss in the blind. Van Someren EJ. Circadian and sleep disturbances in the elderly.
Exp Gerontol. Harper DG , Volicer L , Stopa EG , McKee AC , Nitta M , Satlin A. Disturbance of endogenous circadian rhythm in aging and Alzheimer disease.
Am J Geriatr Psychiatry. Stephan FK , Zucker I. Circadian rhythms in drinking behavior and locomotor activity of rats are eliminated by hypothalamic lesions. Moore RY , Eichler VB.
Loss of a circadian adrenal corticosterone rhythm following suprachiasmatic lesions in the rat. Brain Res. Nagai K , Nishio T , Nakagawa H , Nakamura S , Fukuda Y. Effect of bilateral lesions of the suprachiasmatic nuclei on the circadian rhythm of food-intake.
Ralph MR , Foster RG , Davis FC , Menaker M. Transplanted suprachiasmatic nucleus determines circadian period. Silver R , LeSauter J , Tresco PA , Lehman MN. A diffusible coupling signal from the transplanted suprachiasmatic nucleus controlling circadian locomotor rhythms.
Kramer A , Yang FC , Snodgrass P , et al. Regulation of daily locomotor activity and sleep by hypothalamic EGF receptor signaling. Cheng MY , Bullock CM , Li C , et al. Prokineticin 2 transmits the behavioural circadian rhythm of the suprachiasmatic nucleus. Kraves S , Weitz CJ.
A role for cardiotrophin-like cytokine in the circadian control of mammalian locomotor activity. Nat Neurosci. Slawik H , Stoffel M , Riedl L , et al. Prospective study on salivary evening melatonin and sleep before and after pinealectomy in humans.
Berson DM , Dunn FA , Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Moore RY. Neural control of the pineal gland. Behav Brain Res. Klein DC. J Biol Chem. Johnston JD , Tournier BB , Andersson H , Masson-Pévet M , Lincoln GA , Hazlerigg DG.
Multiple effects of melatonin on rhythmic clock gene expression in the mammalian pars tuberalis. Sáenz de Miera C , Monecke S , Bartzen-Sprauer J , et al. A circannual clock drives expression of genes central for seasonal reproduction.
Buresová M , Dvoráková M , Zvolský P , Illnerová H. Human circadian rhythm in serum melatonin in short winter days and in simulated artificial long days. Neurosci Lett. Wehr TA , Giesen HA , Moul DE , Turner EH , Schwartz PJ.
Suppression of men's responses to seasonal changes in day length by modern artificial lighting. Am J Physiol. Reppert SM , Weaver DR , Rivkees SA , Stopa EG.
Putative melatonin receptors in a human biological clock. Weaver DR , Stehle JH , Stopa EG , Reppert SM. Melatonin receptors in human hypothalamus and pituitary: implications for circadian and reproductive responses to melatonin. Dijk DJ , Czeisler CA. Contribution of the circadian pacemaker and the sleep homeostat to sleep propensity, sleep structure, electroencephalographic slow waves, and sleep spindle activity in humans.
J Neurosci. Borbély AA. A two process model of sleep regulation. Hum Neurobiol. Borbély AA , Daan S , Wirz-Justice A , Deboer T.
The two-process model of sleep regulation: a reappraisal. Kornhauser JM , Mayo KE , Takahashi JS. Light, immediate-early genes, and circadian rhythms. Behav Genet. Landgraf D , Wang LL , Diemer T , Welsh DK. NPAS2 compensates for loss of CLOCK in peripheral circadian oscillators.
PLoS Genet. Ribas-Latre A , Eckel-Mahan K. Interdependence of nutrient metabolism and the circadian clock system: importance for metabolic health. Mol Metab.
Balsalobre A , Damiola F , Schibler U. A serum shock induces circadian gene expression in mammalian tissue culture cells. Pagani L , Semenova EA , Moriggi E , et al. The physiological period length of the human circadian clock in vivo is directly proportional to period in human fibroblasts.
PLoS One. Lane JM , Vlasac I , Anderson SG , et al. Genome-wide association analysis identifies novel loci for chronotype in , individuals from the UK Biobank. Nat Commun. Hu Y , Shmygelska A , Tran D , Eriksson N , Tung JY , Hinds DA.
GWAS of 89, individuals identifies genetic variants associated with self-reporting of being a morning person. Hasan S , Santhi N , Lazar AS , et al. Assessment of circadian rhythms in humans: comparison of real-time fibroblast reporter imaging with plasma melatonin.
FASEB J. Pagani L , Schmitt K , Meier F , et al. Serum factors in older individuals change cellular clock properties.
Duffy JF , Dijk DJ , Klerman EB , Czeisler CA. Later endogenous circadian temperature nadir relative to an earlier wake time in older people.
Duffy JF , Czeisler CA. Age-related change in the relationship between circadian period, circadian phase, and diurnal preference in humans.
Bordyugov G R , Lehmann R , Rozman D , Herzel H. Timing of circadian genes in mammalian tissues. Patel VR , Ceglia N , Zeller M , Eckel-Mahan K , Sassone-Corsi P , Baldi P.
The pervasiveness and plasticity of circadian oscillations: the coupled circadian-oscillators framework. Storch KF , Lipan O , Leykin I , et al. Extensive and divergent circadian gene expression in liver and heart. Harbour VL , Weigl Y , Robinson B , Amir S. Comprehensive mapping of regional expression of the clock protein PERIOD2 in rat forebrain across the h day.
Eckel-Mahan K , Sassone-Corsi P. Metabolism and the circadian clock converge. Physiol Rev. Zheng X , Sehgal A. AKT and TOR signaling set the pace of the circadian pacemaker.
Cancer Circadian rhythm disruption that carry Mediterranean meal planner Circadian rhythm disruption gene will grow rapidly and divide after shutting down their Circadian rhythm disruption circadian rhythms, a new Wilmot Cancer Institute study Circadian rhythm disruption. Ehythm people, a disruption of the biological Circadin can dlsruption caused by uneven sleep, jet lag, disruptikn shift work, or disruptioh nighttime snacking. In Circadian rhythm disruption latest Circadian rhythm disruption, the team Circadian rhythm disruption at what rhytbm deep inside cancer cells, rhythk of Circadain has its own hour cycle. Researchers discovered that the MYC oncogene shuts down circadian rhythms in cancer cells, stopping circadian rhythms in up to 85 percent of the genes in cancer cells, and changing the time of day in which cell metabolism peaks. The MYC gene is very common, being implicated in about one-third of all cancers, including lung, liver, breast, blood, colon, pancreas, and skin. Juliana Cazarin de Menezes, PhD, a postdoctoral fellow in the Altman Laband technician Rachel DeRollo, are co-first authors of the new study, which was published in PLoS Genetics. Scientists discovered an important molecular link between lung tumor growth and disrupted circadian rhythms, according to a new paper co-authored by a Wilmot Cancer Institute investigator and led by the Scripps Research Institute in California.
0 thoughts on “Circadian rhythm disruption”