Video
Diabetic Foot Ulcer 101Diabetic foot management -
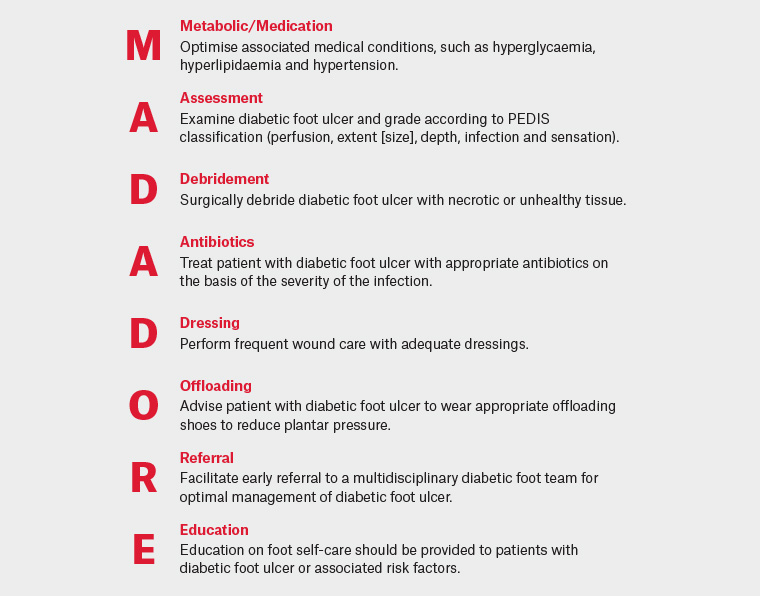
This guideline provides evidence-based recommendations on how to assess and manage people who have been diagnosed with diabetic foot ulcers. Read more. Assessment and Management of Foot Ulcers for People with Diabetes second edition. Do you want to learn about and implement the most- up-to-date evidence-based recommendations on this topic with your colleagues?
Download and share the full best practice guideline BPG , Assessment and Management of Foot Ulcers for People with Diabetes.
See below for a snapshot of the recommendations from this BPG. We strongly suggest you review the full BPG before implementing the recommendations and good practice statements. The BPG also includes further resources to support implementation and evaluation.
Recommendation 1. Recommendation 2. Recommendation 3. Recommendation 4. Recommendation 5. Recommendation 6.
clinical practice guideline and provide resources and organizational and administrative supports to facilitate clinician uptake. Disclaimer: These guidelines are not binding for nurses, other health providers or the organizations that employ them.
The use of these guidelines should be flexible and based on individual needs and local circumstances. They constitute neither a liability nor discharge from liability. The Registered Nurses' Association of Ontario RNAO is developing a third edition of this best practice guideline BPG , with the working title Diabetic Foot Complications.
The anticipated publication date is This new edition will replace Assessment and Management of Foot Ulcers for People with Diabetes and Reducing Foot Complications for People with Diabetes Best practice guidelines.
Assessment and Management of Foot Ulcers for People with Diabetes Published: March Available in English, French, Spanish, Chinese, Simplified.
Download en Télécharger fr descargar es Xiàzài zh-cn. Guideline Revision status. D iabetic foot problems, such as ulcerations, infections, and gangrene, are the most common cause of hospitalization among diabetic patients. Routine ulcer care, treatment of infections, amputations, and hospitalizations cost billions of dollars every year and place a tremendous burden on the health care system.
Calluses,edema, and peripheral vascular disease have also been identified as etiological factors in the development of diabetic foot ulcers. Although the pathogenesis of peripheral sensory neuropathy is still poorly understood, there seem to be multiple mechanisms involved, including the formation of advanced glycosylated end products and diacylglycerol, oxidative stress, and activation of protein kinase Cβ.
Furthermore, the Diabetes Control and Complications Trial 2 and other prospective studies have confirmed the pivotal role of hyperglycemia in the onset and progression of neuropathy.
The data linking glycemic control and neuropathy are not as clear cut as those for retinopathy because of the difficulty in identifying objective measures to assess the many stages of neuropathy over time and because the symptoms, or lack thereof, of neuropathy may be misleading if assessed only through patient questionnaires.
Finally,the differential diagnosis of peripheral neuropathy is quite large, and patients may have other etiologies, as well. Even so, it is important for clinicians to know the basics of evaluation and treatment of foot ulcers seen in diabetic patients.
Using the g Semmes-Weinstein monofilament. The monofilament is applied to various areas on the foot e. Patients are asked to identify the location of the filament, preferably with their eyes closed. Foot ulcer evaluation should include assessment of neurological status,vascular status, and evaluation of the wound itself.
Another useful instrument is the C tuning fork, which can be used to determine whether a patient's vibratory sensation is intact by checking at the ankle and first metatarsal-phalangeal joints.
The notion is that metabolic neuropathies have a gradient in intensity and are most severe distally. Thus,a patient who cannot sense vibration at the big toe but can detect vibration at the ankle when the tuning fork is immediately transferred from toe to ankle demonstrates a gradient in sensation suggestive of a metabolic neuropathy.
In general, you should not be able to sense vibration of the tuning fork in your fingers for more than 10 seconds after the time when the patient can no longer sense vibration at the great toe. Both of these tests can be performed quickly in any office setting.
Achilles and patellar reflexes can also be checked easily but are unreliable in the assessment of diabetic peripheral neuropathy. More in-depth analysis can be performed using a vibrometer a device designed to more objectively measure vibratory sense , assessing temperature sense, performing nerve conduction studies, and checking position sense and balance.
These tests are usually performed in a neurological laboratory. A much more detailed review of peripheral neuropathy has been published in the journal Diabetes Care and is available online in full text at no charge.
Vascular assessment is important for eventual ulcer healing and is essential in the evaluation of diabetic ulcers. Vascular assessment includes checking pedal pulses, the dorsalis pedis on the dorsum of the foot, and the posterior tibial pulse behind the medial malleolus, as well as capillary filling time to the digits.
The capillary filling time is assessed by pressing on a toe enough to cause the skin to blanch and then counting the seconds for skin color to return. If pedal pulses are nonpalpable, the patient should be sent to a noninvasive vascular laboratory for further assessment, which may include checking lower extremity arterial pressures by Doppler and recording pulse volume waveforms.
The ankle brachial index is often not helpful because of high pressures resulting from noncompressible arteries. However, toe pressures are very useful in determining the healing potential of an ulcer. In addition,transcutaneous oxygen measurements are often useful in determining whether a foot wound can heal.
Ulcer evaluation should include documentation of the wound's location,size, shape, depth, base, and border. A sterile stainless steel probe is useful in assessing the presence of sinus tracts and determining whether a wound probes to a tendon, joint, or bone.
X-rays should be ordered on all deep or infected wounds, but magnetic resonance imaging often is more useful because it is more sensitive in detecting osteomyelitis and deep abscesses.
Signs of infection, such as the presence of cellulites, odor, or purulent drainage, should be documented, and aerobic and anaerobic cultures should be obtained of any purulent exudates. Culturing a dry or clean wound base has proven to be useless because most wounds are colonized, and this practice leads to overprescribing of antibiotics.
A foot lesion confirmed as malignant melanoma. The patient was originally referred for suspected gangrene on the heel. After all physical findings have been noted, a differential diagnosis should be established.
One cannot assume that an ulcer is a diabetic foot ulcer without considering other possibilities, such as malignancies or vasculitic disorders Figure 2. Successful treatment of diabetic foot ulcers consists of addressing these three basic issues: debridement, offloading, and infection control.
Debridement consists of removal of all necrotic tissue, peri-wound callus,and foreign bodies down to viable tissue. Proper debridement is necessary to decrease the risk of infection and reduce peri-wound pressure, which can impede normal wound contraction and healing.
After debridement, the wound should be irrigated with saline or cleanser, and a dressing should be applied. Dressings should prevent tissue dessication, absorb excess fluid, and protect the wound from contamination.
There are hundreds of dressings on the market, including hydrogels, foams, calcium alginates, absorbent polymers,growth factors, and skin replacements.
Becaplermin contains the β-chain platelet-derived growth factor and has been shown in double-blind placebo-controlled trials to significantly increase the incidence of complete wound healing.
Its use should be considered for ulcers that are not healing with standard dressings. In case of an abscess, incision and drainage are essential, with debridement of all abscessed tissue. Many limbs have been saved by timely incision and drainage procedures; conversely, many limbs have been lost by failure to perform these procedures.
Treating a deep abscess with antibiotics alone leads to delayed appropriate therapy and further morbidity and mortality.
Having patients use a wheelchair or crutches to completely halt weight bearing on the affected foot is the most effective method of offloading to heal a foot ulceration. Armstrong et al. Inappropriate application of TCCs may result in new ulcers, and TCCs are contraindicated in deep or draining wounds or for use with noncompliant,blind, morbidly obese, or severely vascularly compromised patients.
Clinicians often prefer removable cast walkers because they do not have some of the disadvantages of TCCs. Removability is an advantage in that it allows for daily wound inspection, dressing changes, and early detection of infection.
Postoperative shoes or wedge shoes are also used and must be large enough to accommodate bulky dressings. Proper offloading remains the biggest challenge for clinicians dealing with diabetic foot ulcers. Limb-threatening diabetic foot infections are usually polymicrobial.
Commonly encountered pathogens include methicillin-resistant staphylococcus aureus , β-hemolytic streptococci,enterobacteriaceae, pseudomonas aeruginosa , and enterococci.
Anaerobes, such as bacteroides, peptococcus , and peptostreptococcus , are rarely the sole pathogens but are seen in mixed infections with aerobes. Antibiotics selected to treat severe or limb-threatening infections should include coverage of gram-positive and gram-negative organisms and provide both aerobic and anaerobic coverage.
Patients with such wounds should be hospitalized and treated with intravenous antibiotics.
Diabetic foot Best hydration practices are associated with significant morbidity and mortality Doot can Diabetic foot management managmeent to Diabetic foot management and lower limb amputation if not recognised and Diabbetic in Managenent timely manner. All patients with diabetes should have an annual foot review by a general practitioner or podiatrist. A three-monthly foot review is recommended for any patient with a history of a diabetic foot infection. Assessment involves identification of risk factors including peripheral neuropathy and peripheral vascular disease, and examination of ulceration if present. Diabetic foot ulcers are a significant cause of morbidity and mortality in the Western world and can be complex and costly. The two most important risk factors are peripheral neuropathy sensory, motor and autonomic and peripheral vascular disease PVD. Foot disorders Diabetic foot management as ulceration, infection, and gangrene are the leading causes of hospitalization in patients with diabetes Eating window benefits. Neuropathy is often Diabeyic predisposing factor Diabetoc ulceration and amputation. The diabetic foot and its sequelae account for billions of dollars in direct medical expenditures, as well as lengthy hospital stays and periods of disability. Approximately 85 percent of all diabetes-related lower-extremity amputations are preceded by foot ulcers. The etiology of diabetic foot ulcers usually has many components.
Ich denke, dass Sie nicht recht sind. Geben Sie wir werden besprechen. Schreiben Sie mir in PM.
��G
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Ich kann die Position verteidigen.
Ich denke, dass Sie sich irren. Schreiben Sie mir in PM.