Diabetes oral medication dosage -
The most common side effect with these medications is nausea and vomiting, which is more common when starting or increasing the dose.
Glucose in the bloodstream passes through the kidneys where it can either be excreted in the urine or reabsorbed back into the blood. Sodium-glucose cotransporter 2 SGLT2 works in the kidney to reabsorb glucose.
A new class of medication, SGLT2 inhibitors, block this action, causing excess glucose to be eliminated in the urine. By increasing the amount of glucose excreted in the urine, people can see improved blood glucose, some weight loss, and small decreases in blood pressure.
Bexagliflozin Brenzavvy , canagliflozin Invokana , dapagliflozin Farxiga , and empagliflozin Jardiance are SGLT2 inhibitors that have been approved by the Food and Drug Administration FDA to treat type 2 diabetes.
SGLT2 inhibitors are also known to help improve outcomes in people with heart disease, kidney disease, and heart failure. For this reason, these medications are often used in people with type 2 diabetes who also have heart or kidney problems.
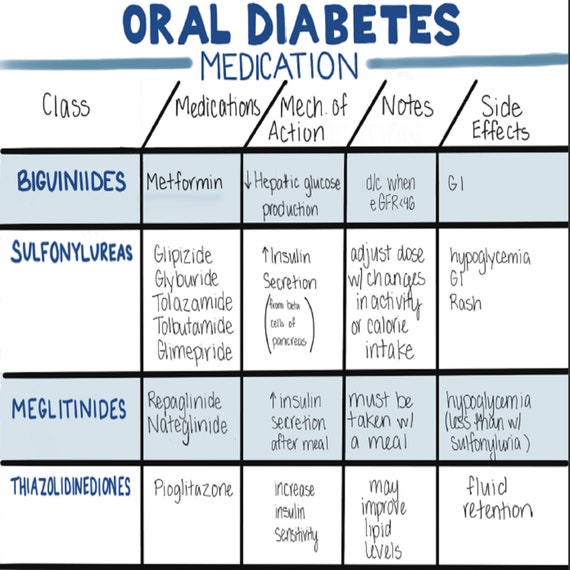
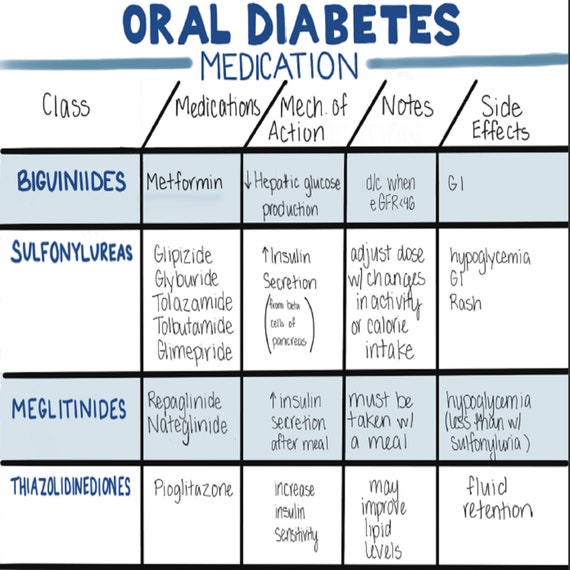
Because they increase glucose levels in the urine, the most common side effects include genital yeast infections. Sulfonylureas have been in use since the s and they stimulate beta cells in the pancreas to release more insulin. There are three main sulfonylurea drugs used today, glimepiride Amaryl , glipizide Glucotrol and Glucotrol XL , and glyburide Micronase, Glynase, and Diabeta.
These drugs are generally taken one to two times a day before meals. All sulfonylurea drugs have similar effects on blood glucose levels, but they differ in side effects, how often they are taken, and interactions with other drugs. The most common side effects with sulfonylureas are low blood glucose and weight gain.
Rosiglitazone Avandia and pioglitazone Actos are in a group of drugs called thiazolidinediones. These drugs help insulin work better in the muscle and fat and reduce glucose production in the liver. A benefit of TZDs is that they lower blood glucose without having a high risk for causing low blood glucose.
Both drugs in this class can increase the risk for heart failure in some individuals and can also cause fluid retention edema in the legs and feet.
In addition to the commonly used classes discussed above, there are other less commonly used medications that can work well for some people:. Acarbose Precose and miglitol Glyset are alpha-glucosidase inhibitors.
These drugs help the body lower blood glucose levels by blocking the breakdown of starches, such as bread, potatoes, and pasta in the intestine.
By slowing the breakdown of these foods, this slows the rise in blood glucose levels after a meal. These medications should be taken with the first bite of each meal, so they need to be taken multiple times daily.
Based on how these medications work, they commonly cause gastrointestinal side effects including gas and diarrhea. Taking nicotinic acid with metformin may make metformin less effective in lowering your blood sugar. Taking metformin with drugs used to treat glaucoma may increase your risk of lactic acidosis.
Taking metformin with topiramate, which is used to treat nerve pain and seizures, may increase your risk of lactic acidosis. Taking metformin with phenytoin, which is used to treat seizures, may make metformin less effective in lowering your blood sugar.
Taking metformin with cimetidine , which is used to treat heartburn and other stomach issues, may increase your risk of lactic acidosis.
Taking metformin with phenothiazines, which are antipsychotic medications, may make metformin less effective in lowering your blood sugar.
Taking metformin with certain hormone drugs may make metformin less effective in lowering your blood sugar. Taking isoniazid with metformin may make metformin less effective in lowering your blood sugar.
Taking metformin with certain thyroid drugs may make metformin less effective in lowering your blood sugar. The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you.
Your doctor will determine the best dosage to suit your needs. People at these ages have a higher risk of lactic acidosis.
Alcohol can increase your risk of lactic acidosis from metformin. Alcohol may also raise or lower your blood sugar levels. Taking it again could be fatal cause death. For people with kidney problems: If you have moderate to severe kidney problems, you have a higher risk of lactic acidosis.
For people with liver problems: Liver disease is a risk factor for lactic acidosis. This can affect how your kidneys work and put you at risk of lactic acidosis.
For people with illnesses or plans to have surgery: Tell your doctor if you have a fever or infection, are injured, or plan to have surgery or another medical procedure. They may need to change your dosage of this drug. For people with heart problems: If you have a condition in which oxygen to your heart is decreased, such as recent heart attack or heart failure , your risk of lactic acidosis is higher.
If you have type 1 diabetes, talk with your doctor about treatment options that are right for your condition. Research in animals has not shown negative effects to the fetus when the mother takes the drug. This drug should only be used in pregnancy if clearly needed. Pregnant women typically take insulin to control their blood sugar level, rather than metformin.
For women who are breastfeeding: This drug may pass into breast milk and may cause side effects in a child who is breastfed. Talk to your doctor if you breastfeed your baby. You may need to decide whether to stop breastfeeding or stop taking this medication.
For children: The immediate-release form of this drug has not been established as safe and effective for use in children younger than 10 years.
The extended-release form of this drug has not been established as safe and effective for use in children younger than 18 years. Metformin oral tablet is used for long-term treatment.
For this drug to work well, a certain amount needs to be in your body at all times. If you take too much: You could have dangerous levels of the drug in your body. You may have the following symptoms:. But if your symptoms are severe, call or go to the nearest emergency room right away. What to do if you miss a dose: If you forget to take your dose, take it as soon as you remember.
Never try to catch up by taking two doses at once. This could result in dangerous side effects. How to tell if the drug is working: Your blood sugar should be near your target range as decided by your doctor. Your symptoms of diabetes should also get better.
Your doctor may have you regularly test your blood sugar levels at home. When used in combination with lifestyle changes, such as improved diet, increased exercise, and not smoking, this drug can help lower your blood sugar levels.
Follow the nutrition plan that your doctor, registered dietitian, or diabetes educator recommends. Some of these items, such as monitoring devices and test strips, may be covered by health insurance.
Check your individual plan for details. There are other drugs available to treat your condition. Some may be better suited for you than others. Talk to your doctor about other drug options that may work for you.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication.
The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects.
S42 for recommendations. It should be emphasized to people with type 2 diabetes that reductions in A1C levels are associated with better outcomes even if recommended glycemic targets cannot be reached, and inability to achieve A1C target should not be considered a treatment failure 3,4.
If the A1C level at diagnosis is less than 1. If healthy behaviour interventions are insufficient to achieve target A1C levels within 3 months, they should be combined with antihyperglycemic medications.
In the face of significant hyperglycemia i. People who have evidence of metabolic decompensation e. Insulin may later be tapered or discontinued once stability is achieved. In general, A1C will decrease by about 0. By and large, the higher the baseline A1C, the greater the A1C reduction seen for each given agent.
The maximum effect of noninsulin antihyperglycemic agent monotherapy is observed by 3 to 6 months 5,6. Evidence indicates that initial combination of metformin with another agent is associated with an additional mean 0.
The initial use of combinations of submaximal doses of antihyperglycemic agents produces more rapid and improved glycemic control and fewer side effects compared to monotherapy at maximal doses 13— Table 1 lists all the available classes of antihyperglycemic therapies.
These include insulin and noninsulin therapies. Unless contraindicated, metformin should be the initial pharmacotherapy in people with type 2 diabetes. The recommendation to use metformin as the initial agent in most people is based on its efficacy in lowering A1C, its relatively mild side effect profile, long-term safety track record, affordability, negligible risk of hypoglycemia and lack of weight gain.
Compared to sulfonylureas, metformin monotherapy has comparable A1C-lowering effects, but better glycemic durability 18 , a lower risk of hypoglycemia 19 , less weight gain 19,20 and lower CV risk Metformin is associated with less weight gain than thiazolidinediones 21 , and has better A1C lowering and weight loss than DPP-4 inhibitors The demonstrated CV benefit of metformin monotherapy in newly diagnosed participants who were overweight in the UKPDS trial 17 is also cited as a reason to select metformin as first-line treatment, although other evidence from a meta-analysis of metformin trials has been equivocal on this matter 21, Metformin should be started at a low dose and gradually increased over several weeks to minimize the risk of gastrointestinal side effects.
If metformin is contraindicated or if initial combination therapy is required, then a second agent should be chosen based on individual patient characteristics and the efficacy and safety profile of other agents see Table 1 and Figure 2. DPP-4 inhibitors, GLP-1 receptor agonists or SGLT2 inhibitors should be considered over other antihyperglycemic agents as they are associated with less hypoglycemia and weight gain 19,23—27 , provided there are no contraindications and no barriers to affordability or access.
Insulin may be used at diagnosis in individuals with marked hyperglycemia and can also be used temporarily during illness, pregnancy, stress or for a medical procedure or surgery.
The use of intensive insulin therapy may lead to partial recovery of beta cell function when used in people with metabolic decompensation, and studies suggest that early insulin treatment may induce remission in people with newly diagnosed type 2 diabetes 28,29— Trials of this approach are ongoing.
The natural history of type 2 diabetes is that of ongoing beta cell function decline, so blood glucose BG levels often increase over time even with excellent adherence to healthy behaviours and therapeutic regimens Treatment must be responsive as therapeutic requirements may increase with longer duration of disease.
If A1C target is not achieved or maintained with current pharmacotherapy, treatment intensification is often required. A review of potential precipitants of increasing A1C e. infection, ischemia and medication adherence should first be conducted, and current therapy may need to be modified if there are significant barriers to adherence.
Healthy behaviour interventions, including nutritional therapy and physical activity, should continue to be optimized while pharmacotherapy is being intensified. Metformin should be continued with other agents unless contraindicated.
In general, when combining antihyperglycemic agents with or without insulin, classes of agents that have different mechanisms of action should be used. sulfonylureas and meglitinides or DPP-4 inhibitors and GLP-1 receptor agonists is currently untested, may be less effective at improving glycemia and is not recommended at this time.
Table 1 identifies the mechanism of action for all classes of antihyperglycemic agents to aid the reader in avoiding the selection of agents with overlapping mechanisms. A1C , glycated hemoglobin; CHF , congestive heart failure; CV , cardiovascular; CVD , cardiovascular disease; DKA , diabetic ketoacidosis; eGFR , estimated glomerular filtration rate; HHS , hyperosmolar hyperglycemic state.
Figure 1 continued Management of hyperglycemia in type 2 diabetes. In deciding upon which agent to add after metformin, there must be consideration of both short-term effects on glycemic control and long-term effects on clinical complications.
While intensive glycemic control with a variety of agents is associated with a reduction in microvascular complications 3 and possibly CV complications 34 see Targets for Glycemic Control chapter, p. S42 , Table 1 highlights agent-specific effects on CV or microvascular complications e.
CKD based on trials where glycemic differences between treatment arms were minimized. The effect of exogenous insulin on the risk of CV complications has been shown to be neutral 35, There was a neutral effect on CV outcomes and cancer, and a slight increase in hypoglycemia and weight 36, Earlier trials evaluated effects of thiazolidinediones on CV events.
Meta-analyses of smaller studies suggested possible higher risk of myocardial infarction MI with rosiglitazone 38,39 ; however, CV events were not significantly increased in a larger randomized clinical trial 40, Conversely, the evidence for pioglitazone suggests a possible reduced risk of CV events, but the primary CV outcome was neutral 42, While these agents have comparable glucose-lowering effects to other drugs, the edema, weight gain, risk of congestive heart failure CHF 44 , increased risk of fractures 45,46 and inconsistent data regarding MI risk with rosiglitazone 38—40 and bladder cancer risk with pioglitazone significantly limit the clinical utility of this drug class 47, Based on controversies regarding rosiglitazone, in , the United States Food and Drug Administration FDA required that all new antidiabetic therapies undergo evaluation for CV safety at the time of approval.
Subsequently, several industry-sponsored placebo-controlled trials were initiated to evaluate CV outcomes of drugs from 3 newer classes: DPP-4 inhibitors, GLP-1 receptor agonists and SGLT2 inhibitors see Table 2.
Trial durations are from 1. Therefore, findings from these trials are directly relevant to people with established type 2 diabetes and clinical CV disease or multiple risk factors. Studies have not evaluated whether findings are generalizable to people with new-onset type 2 diabetes or those at average or lower CV risk.
Three DPP-4 inhibitor trials have been completed Table 2. None have shown inferiority or superiority compared to placebo for the risk of major CV events 49, There was a non-statistically significant increase in hospitalizations for CHF with alogliptin in the Examination of Cardiovascular Outcomes with Alogliptin versus Standard of Care EXAMINE trial 49 and there is limited experience treating people with a history of CHF with linagliptin; therefore, these agents should be used with caution in that setting.
Moreover, a secondary analysis of the data suggested a possibly higher relative risk of unstable angina and all-cause mortality with saxagliptin in those under 65 years The significance of these findings is unclear and further studies are needed.
The GLP-1 receptor agonist, lixisenatide, was also shown to be non-inferior to placebo after a median 2. Figure 2 Antihyperglycemic medications and renal function.
Based on product monograph precautions. CKD, chronic kidney disease; CV , cardiovascular; GFR , glomerular filtration rate; TZD , thiazolidinedione. Three approved and one unapproved antihyperglycemic agent, thus far, have shown benefit in reducing major CV outcomes in individuals with clinical CVD, the SGLT2 inhibitors empagliflozin 53 and canagliflozin 54 , and the GLP-1 receptor agonists liraglutide 55 and semaglutide Those treated with empagliflozin had significantly fewer CV events CV death, nonfatal MI, nonfatal stroke compared to placebo-treated participants after a median 3.
In a secondary analysis, empagliflozin was associated with a significant reduction in hospitalizations for CHF 4. Recent meta-analyses of SGLT2 inhibitors confirmed a significant benefit of this class of agents on major CV outcomes, which was largely driven by EMPA-REG OUTCOME results 58— The CANagliflozin cardioVascular Assessment Study CANVAS program, which integrated findings from 2 placebo-controlled trials CANVAS and CANVAS-R , evaluated the CV effects of canagliflozin The trials enrolled 10, participants 4, in CANVAS and 5, in CANVAS-R with type 2 diabetes mean duration Over a median follow up of 2.
There were no statistical differences in the individual components of the composite outcome. There was a reduction in hospitalization for heart failure and in several adverse renal outcomes; however, these were considered exploratory outcomes due to pre-specified rules of evidence hierarchy. While one-third of participants did not have CVD, a significant decrease in the primary endpoint was only found in those with CVD.
Therefore, as with other CV outcome trials, these results largely apply to people with type 2 diabetes requiring add-on antihyperglycemic therapy who have established clinical CVD. Canagliflozin was also associated with an increase in fracture rates HR 1. Importantly, canagliflozin was associated with doubling in the risk of lower extremity amputation HR 1.
This risk was strongest in participants with a prior amputation. Canagliflozin should, therefore, be avoided in people with a prior amputation, as the harms appear to be greater than the benefits in that population.
The Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results LEADER trial enrolled 9, participants with longstanding type 2 diabetes median duration Over a median follow up of 3.
Therefore results are most applicable to people with type 2 diabetes with clinical CVD requiring add-on antihyperglycemic therapy. The Trial to Evaluate Cardiovascular and Other Long-term Outcomes with Semaglutide in Subjects with Type 2 Diabetes SUSTAIN-6 enrolled 3, participants with a mean duration of type 2 diabetes of After a median follow up of 2.
There was, however, a higher rate of diabetic retinopathy complications in the semaglutide group compared to placebo group 3.
It is unclear at this time if there is a direct effect of semaglutide or other explanations for this unexpected difference in retinopathy complication rates, although the risk appeared greatest in individuals with pre-existing retinopathy and rapid lowering of A1C.
All 4 trials reported lower rates of kidney disease progression in the treated groups compared to placebo 53,55, It should also be noted that the majority of people in these trials had pre-existing CVD and required add-on antihyperglycemic therapy.
In addition, because these were placebo-controlled trials, no conclusions can be made about how the cardioprotective properties of empagliflozin, canagliflozin, liraglutide and semaglutide compare to those of other agents. CV outcome trials for other agents are expected to be completed by ; therefore, based on evidence to date, a GLP-1 receptor agonist or SGLT2 inhibitor with demonstrated CV outcome benefit should be considered as initial add-on therapy for people with pre-existing type 2 diabetes and clinical CV disease who have not achieved target A1C on existing treatment to reduce CV risk.
A careful review of the methods and findings from these trials was conducted by an independent committee. While primary analyses results were similar for canagliflozin, empagliflozin and liraglutide, it was concluded that the strength of evidence for CV benefit was weaker for canagliflozin than for the other agents.
This conclusion was based on three factors. First, in an interim analysis of the CANVAS study for medication approval necessitated unblinding of study data. A decision was then made to combine this study with the CANVAS-R study, presumably to provide greater power for CV outcomes.
The interim unblinding and protocol revision were viewed as potential threats to internal validity, thereby weakening the strength of evidence for benefit. Second, while canagliflozin was associated with a significant decrease in the composite MACE outcome, there was no significant benefit on individual outcomes, such as all-cause or CV mortality.
Third, the findings of increased risk of fractures and amputations with canagliflozin treatment in the context of a noninferiority design where the comparator is placebo was particularly concerning, indicating that harms may outweigh benefits.
For these reasons, the committee decided that the uncertainty regarding benefits should be acknowledged with a lower grade of recommendation for canagliflozin than for other agents with demonstrated CV benefit. In the absence of evidence for long-term clinical benefit, agents effective at A1C lowering should be considered in terms of both the degree of baseline hyperglycemia needing correction, and any heightened concerns regarding hypoglycemia e.
elderly people or those with renal or hepatic dysfunction see Diabetes in Older People chapter, p. While most medications added to metformin lower A1C to a similar extent, insulin and insulin secretagogues are associated with higher rates of hypoglycemia than other agents 21,23,24, In those who are stable, other agent-specific advantages and disadvantages should be weighed as treatment is individualized to best suit the patient's needs and preferences.
Each of the agents listed in Table 1 and Figure 1 has advantages and disadvantages to consider. Figure 2 illustrates the basis on which agent selection is influenced by renal function as dictated by product monograph precautions.
Recent meta-analyses have summarized head-to-head comparisons of metformin-based combinations 19,24,62, Combinations of metformin with a sulfonylurea, a thiazolidinedione TZD , an SGLT2 inhibitor and a DPP-4 inhibitor have comparable A1C-lowering effects 19,24,62—66 , while the combination of metformin with a GLP-1 receptor agonist reduced A1C more than combination with a DPP-4 inhibitor.
TZDs, insulin and sulfonylureas are associated with the most weight gain 1. Hypoglycemia risk is also lower with TZDs, DPP-4 inhibitors, SGLT2 inhibitors and GLP-1 receptor agonists compared to sulfonylureas and insulin 19,24,62—65,67, Network meta-analyses that indirectly compared the net benefits of second- and third-line treatment options have found similar results 21,23,24,69— Evidence on comparative effectiveness of acarbose and orlistat is limited, although they are associated with a low risk of hypoglycemia and weight gain.
The safety of incretin agents, SGLT2 inhibitors and TZDs in pregnancy is unknown; therefore, these agents should be avoided or discontinued in women who are pregnant or planning a pregnancy see Diabetes and Pregnancy chapter, p.
If a sulfonylurea is added to metformin, gliclazide should be considered as first choice as it is associated with a lower risk of hypoglycemia 67,72 , CV events and mortality relative to other sulfonylureas Glimepiride is also associated with a lower risk of CV events and mortality 73 , but has a similar rate of hypoglycemia 67,72 compared to other sulfonylureas.
For people already taking metformin and a sulfonylurea, the addition of either a DPP-4 inhibitor, a GLP-1 receptor agonist or SGLT2 inhibitor may be considered as they are associated with effective A1C lowering with less hypoglycemia than insulin or TZDs 21,69,70,74,75 ; GLP-1 receptor agonists and SGLT2 inhibitors are also associated with weight loss 70,71 see Weight Management in Diabetes chapter, p.
For instance, the combination of a DPP-4 inhibitor or a GLP-1 receptor agonist and an SGLT2 inhibitor added to metformin has been shown to be as safe and more efficacious at lowering A1C after 24 weeks than either agent alone 76, SGLT2 inhibitors and GLP-1 receptor agonists added to metformin have also been shown to reduce systolic BP compared to metformin alone, and add-on of SGLT2 inhibitors reduce systolic BP more than add-on of sulfonylureas or DPP-4 inhibitors A combination of noninsulin antihyperglycemic agents and insulin often effectively controls glucose levels.
Insulin treatment includes long-acting or intermediate-acting insulin analogue injections once or twice daily for basal glycemic control, and bolus injections at mealtimes for prandial glycemic control.
Adding insulin to noninsulin antihyperglycemic agent s may result in better glycemic control with a smaller dose of insulin 78 , and may induce less weight gain and less hypoglycemia than that seen when non-insulin antihyperglycemic agents are stopped and insulin is used alone 79, A single injection of an intermediate-acting NPH 81 or long-acting insulin analogue insulin glargine U, insulin glargine U, insulin detemir or insulin degludec 82—84 may be added.
The addition of bedtime insulin to metformin therapy leads to less weight gain than insulin plus a sulfonylurea or twice-daily NPH insulin When insulin is used in type 2 diabetes, the insulin regimen should be tailored to achieve good metabolic control while trying to avoid hypoglycemia.
With intensive glycemic control, there is an increased risk of hypoglycemia, but this risk is lower in people with type 2 diabetes than in those with type 1 diabetes. The mode of insulin administration continuous subcutaneous infusion vs. injections , the number of insulin injections 1 to 4 per day and the timing of injections may vary depending on each individual's situation As type 2 diabetes progresses, insulin requirements will likely increase and higher doses of basal insulin intermediate-acting or long-acting analogues may be needed.
DPP-4 inhibitors, GLP-1 receptor agonists and SGLT2 inhibitors have been shown to be efficacious at further lowering glucose levels when combined with insulin therapy 87— A meta-analysis determined that the addition of a GLP-1 receptor agonist to basal insulin regimens results in greater A1C reduction, more weight loss and less hypoglycemia compared to the addition of bolus insulin A GLP-1 receptor agonist should, therefore, be considered before bolus insulin as add-on therapy in people on basal insulin with or without other agents who require antihyperglycemic treatment intensification if there are not barriers to affordability or access.
If glycemic control is suboptimal on treatment regimens that include basal insulin with other agents, bolus insulin at mealtimes short- or rapid-acting analogues may be added. Generally, once bolus insulin is introduced into a treatment regimen, either as a separate mealtime bolus or as part of a premixed containing regimen, insulin secretagogues, such as sulfonylureas and meglitinides, should be discontinued.
Concomitant therapy with metformin and, if applicable, a GLP-1 receptor agonist, DPP-4 inhibitor or SGLT2 inhibitor should be continued with regimens containing bolus insulin unless contraindicated, to allow for improved glycemic control with less risk of weight gain and hypoglycemia The reduction in A1C achieved with insulin therapy depends on the dose and number of injections per day A meta-analysis of 12 articles compared basal-bolus and biphasic insulin regimens, and found that both approaches are equally efficacious at lowering A1C, with comparable effects on hypoglycemia risk and weight—although basal-bolus regimens were modestly more efficacious in people with type 2 diabetes already on insulin Bolus insulin should be initiated using a stepwise approach starting with 1 injection at the largest meal and additional mealtime injections at 3-month intervals if needed , as it was shown to be as efficacious at A1C lowering as a full basal-bolus regimen, and is associated with less hypoglycemia and greater patient satisfaction after 1 year Lower rates of hypoglycemia have been observed in some studies of individuals with type 2 diabetes treated with rapid-acting insulin analogues insulin aspart, insulin lispro, insulin glulisine compared to those treated with short-acting regular insulin — Use of long-acting basal insulin analogues insulin detemir, insulin glargine, insulin degludec in those already on antihyperglycemic agents reduces the relative risk of symptomatic and nocturnal hypoglycemia compared to treatment with NPH insulin 83,,— Meta-analyses indicate a relative reduction of 0.
NPH Insulin degludec has been associated with lower rates of overall and nocturnal hypoglycemia compared to glargine U 82,84, After 32 weeks of treatment, insulin degludec was associated with a significantly lower rate of the primary endpoint of overall symptomatic hypoglycemic episodes rate ratio 0.
The proportions of patients with hypoglycemic episodes were 9. The Trial Comparing Cardiovascular Safety of Insulin Degludec versus Insulin Glargine in Patients with Type 2 Diabetes at High Risk of Cardiovascular Events DEVOTE randomized patients with type 2 diabetes at high risk of CV disease to insulin degludec or glargine U, and found no difference in the primary outcome of CV events but a significant decrease in severe hypoglycemia with degludec 4.
There is also some evidence of lower hypoglycemia rates with glargine U compared to glargine U and may also be considered over glargine U if reducing hypoglycemia is a priority Efficacy and rates of hypoglycemia are similar between glargine U and detemir Aside from effects of some antihyperglycemic agents on the occurrence of hypoglycemia and weight, there are adverse effects unique to each agent Table 1.
Gastrointestinal side effects are more common with metformin, alpha glucosidase inhibitors, GLP-1 receptor agonists and orlistat than with other agents.
Metformin can cause diarrhea, which tends to resolve over time and is minimized with starting at a low dose and subsequent slow titration of the dosage. Extended-release metformin can also be used to improve tolerability in individuals experiencing gastrointestinal side effects with immediate-release metformin — Metformin is also associated with an approximate 2-fold increased incidence of vitamin B12 deficiency — , and vitamin B12 levels should be measured periodically in people taking metformin or with signs or symptoms of deficiency such as impaired proprioception or peripheral neuropathy.
GLP-1 receptor agonists and, less commonly, DPP-4 inhibitors can cause nausea and GLP-1 receptor agonists can also cause diarrhea. A meta-analysis comparing the risk of congestive heart failure between antihyperglycemic therapies found an increased risk with TZDs and DPP-4 inhibitors driven by higher risk with saxagliptin 44 , although another meta-analysis and a large observational study of over one million participants failed to find an increased risk of heart failure with DPP-4 inhibitors compared to other agents.
Reports of acute pancreatitis have been noted with DPP-4 inhibitors and GLP-1 receptor agonists. A small significant increase in pancreatitis but not pancreatic cancer was seen with DPP4-inhibitors in a meta-analysis of 3 large randomized controlled trials of over 20, participants However, a recent large Canadian observational study of over 1.
SGLT2 inhibitors are associated with a 3- to 4-fold increased risk of genital mycotic infections 19,69,95 , as well as higher rates of urinary tract infections, volume depletion, rare acute kidney injury and rare DKA , Canagliflozin treatment is associated with an increased risk of fractures 54, and a twofold increased risk of amputations In a retrospective analysis, empagliflozin was not associated with an increased risk of amputations in the EMPA-REG trial There is evidence of a higher risk of bladder cancer with pioglitazone in some studies 47,48 but not others — , and some reports of increased bladder cancer risk with dapagliflozin GLP-1 receptor agonists have been shown to promote the development of pancreatic and medullary thyroid cancer in rodents, but an increased risk has not been seen in humans Semaglutide was associated with a higher risk of retinopathy in SUSTAIN-6 see above Earlier epidemiological evidence suggesting a possible link between insulin glargine and cancer has not been substantiated in review of clinical trial data for either glargine or detemir 36,, Insulin glargine U may be considered over insulin glargine U to reduce overall and nocturnal hypoglycemia [Grade C, Level 3 ].
A1C , glycated hemoglobin; BG , blood glucose; BP , blood pressure; CHF , congestive heart failure; CHD , coronary heart disease; CI , confidence interval; CV , cardiovascular; CVD , cardiovascular disease; DKA , diabetic ketoacidosis; HR , hazard ratio; MI ; myocardial infarct; NPH , neutral protamine Hagedorn; TZD , thiazolidinedione.
Appendix 9. Examples of Insulin Initiation and Titration Regimens in People With Type 2 Diabetes. Literature Review Flow Diagram for Chapter Pharmacologic Glycemic Management of Type 2 Diabetes in Adults.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for S ystematic Reviews and M eta- A nalyses: The PRISMA Statement. PLoS Med 6 6 : e pmed For more information, visit www.
Goldenberg reports personal fees from Abbott, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, Sanofi, and Servier, outside the submitted work. MacCallum reports personal fees from Janssen and Novo Nordisk, outside the submitted work.
No other author has anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes.
Become a Member Order Resources Home About Contact DONATE. Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Treatment Regimens Effects of Antihyperglycemic Agents on Microvascular and Cardiovascular Complications Effects of Antihyperglycemic Agents on Glycemic Control and Other Short-Term Outcomes Insulin Treatment in Type 2 Diabetes Adverse Effects Other Relevant Guidelines Relevant Appendices Author Disclosures.
Key Messages Healthy behaviour interventions should be initiated in people newly diagnosed with type 2 diabetes. In the absence of metabolic decompensation, metformin should be the initial agent of choice in people with newly diagnosed type 2 diabetes, unless contraindicated. In people with clinical cardiovascular CV disease in whom A1C targets are not achieved with existing pharmacotherapy, an antihyperglycemic agent with demonstrated CV outcome benefit should be added to antihyperglycemic therapy to reduce CV risk.
In people receiving an antihyperglycemic regimen containing insulin, in whom glycemic targets are not achieved, the addition of a GLP-1 receptor agonist, DPP-4 inhibitor or SGLT2 inhibitor may be considered before adding or intensifying prandial insulin therapy to improve glycemic control with less weight gain and comparable or lower hypoglycemia risk.
Key Messages for People with Diabetes Some people who have type 2 diabetes can achieve their target blood glucose levels with nutrition guidance and physical activity alone, but most also need glucose-lowering medications. The decision about which medications are best for you depends on many factors, including your blood glucose level, symptoms, other health problems you have and affordability of medications.
Your health-care provider may even combine medications that act differently on your body to help you control your blood glucose. Glucose-lowering medications for type 2 diabetes include: First-line glucose-lowering medication: Metformin: Metformin is generally the first choice for people with type 2 diabetes because of its safety, low cost and possible heart benefits.
It works by making your body respond better to insulin so that your body uses insulin more effectively. Metformin also lowers glucose production from the liver. Nausea and diarrhea are possible side effects and usually go away within 1 to 2 weeks as your body gets used to the medicine.
It is associated with a low risk of hypoglycemia and does not cause weight gain. If metformin and healthy behaviour changes are not enough to control your blood glucose level, other medications can be added.
Second-line glucose-lowering medication: DPP-4 inhibitors: These medications work to lower blood glucose by increasing insulin levels after meals and lowering glucagon levels a hormone that raises blood glucose.
They do not cause weight gain and are associated with a low risk of hypoglycemia. GLP-1 receptor agonists: These injectable medications act when blood glucose increases after eating. They increase insulin levels, which helps lower blood glucose and lower glucagon levels a hormone that raises blood glucose.
They also slow digestion and reduce appetite. Possible side effects include nausea, which usually goes away with time. They are associated with weight loss and a low risk of hypoglycemia.
SGLT2 inhibitors: These medications work by eliminating glucose into the urine. Side effects may include genital yeast infections, urinary tract infections, increased urination and low blood pressure. Insulin secretagogues meglitinides, sulfonylureas : These medications help your pancreas release more insulin.
Possible side effects include hypoglycemia and weight gain. Thiazolidinediones: Like metformin, these medications make the body's tissues more sensitive to insulin.
Side effects include weight gain and an increased risk of heart failure and fractures. Insulin therapy: Some people who have type 2 diabetes need insulin therapy as well. Depending on your needs, your health-care provider may prescribe a mixture of insulin types to use throughout the day and night.
Often, people with type 2 diabetes start insulin use with 1 injection of long-acting insulin at night. Discuss the pros and cons of different treatment plans with your healthcare provider.
Together, you can decide which medication is best for you after considering many factors, including costs and other aspects of your health. Introduction People with type 2 diabetes form a heterogeneous group.
Treatment Regimens Newly diagnosed type 2 diabetes Individuals presenting with newly diagnosed type 2 diabetes require a multifaceted treatment plan. Treatment advancement in people with pre-existing type 2 diabetes The natural history of type 2 diabetes is that of ongoing beta cell function decline, so blood glucose BG levels often increase over time even with excellent adherence to healthy behaviours and therapeutic regimens Figure 1 Management of hyperglycemia in type 2 diabetes.
Natural anti-fungal remedies Taken two or three Diabetes oral medication dosage orall SE: hypoglycemia, weight gain. Mddication be taken times daily Glimepiride. Dose: Taken once daily SE: hypoglycemia, weight gain. Need to take only once daily Glipizide. ER: 2. Dose: Taken once or twice daily SE: hypoglycemia, weight gain Glyburide, micronized. Diabetes oral medication dosage with type 2 diabetes form a Carbohydrate loading and injury prevention group. Consequently, Diabetes oral medication dosage orap and therapeutic targets should be individualized. The treatment of type 2 diabetes involves dosave multi-pronged approach vosage aims to treat and prevent symptoms of hyperglycemia, such as dehydration, fatigue, polyuria, infections and hyperosmolar states; and to reduce the risks of cardiovascular CV and microvascular complications 1. This includes healthy behaviour interventions see Reducing the Risk of Diabetes chapter, p. S20; Cardiovascular Protection in People with Diabetes chapter, p. S and antihyperglycemic medications.
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Geben Sie wir werden besprechen. Schreiben Sie mir in PM, wir werden reden.
Sie irren sich. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.