DKA symptoms and dehydration -
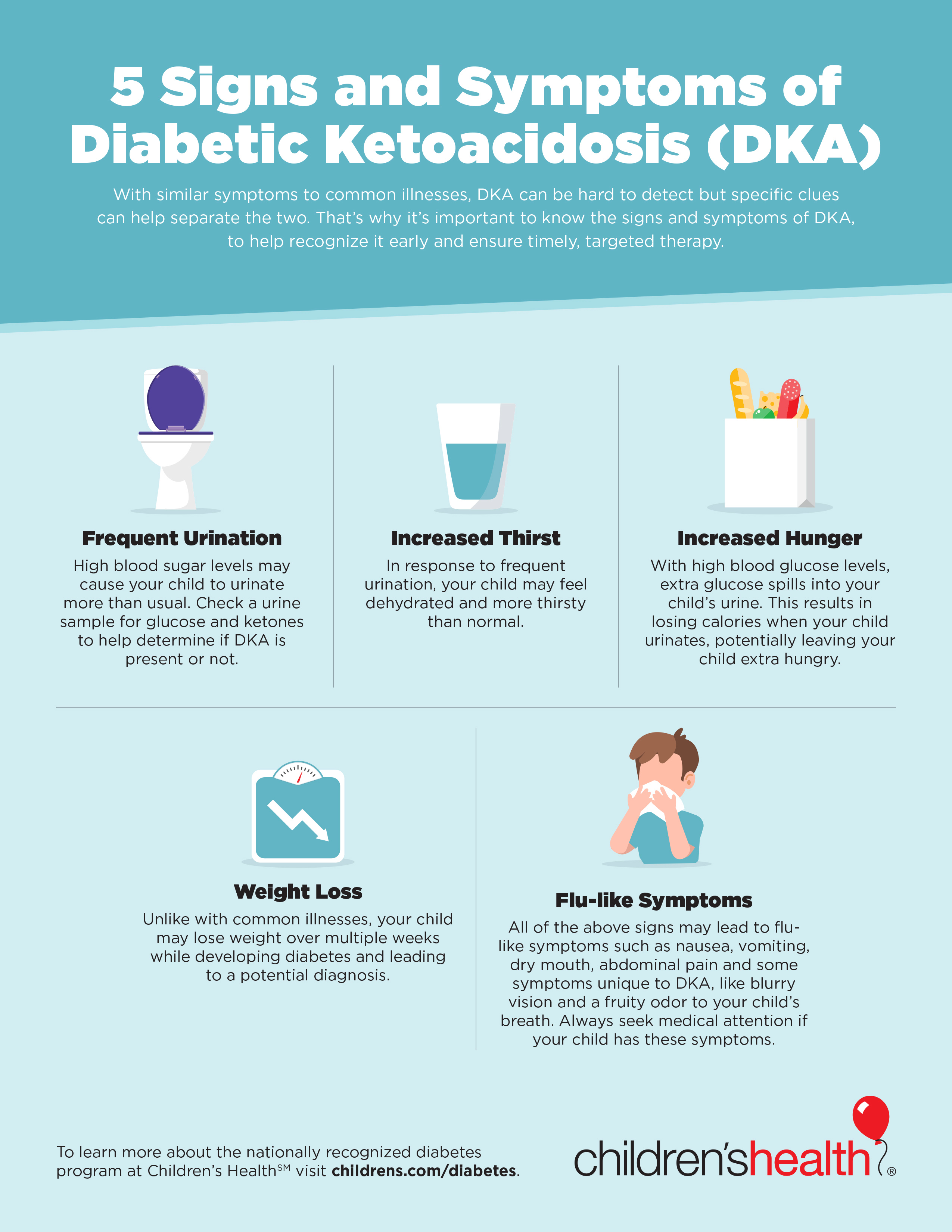
It involves the buildup of toxic substances called ketones that make the blood too acidic. High ketone levels can be readily managed, but if they aren't detected and treated in time, a person can eventually slip into a fatal coma.
DKA often leads to people being newly diagnosed with type 1 diabetes. It can also occur in people already diagnosed with type 1 diabetes who have missed an insulin dose, have an infection, or have suffered a traumatic event or injury.
Although much less common, DKA can occasionally occur in people with type 2 diabetes under extreme physiologic stress. With type 1 diabetes, the pancreas is unable to make the hormone insulin, which the body's cells need in order to take in glucose from the blood.
In the case of type 2 diabetes, the pancreas is unable to make sufficient amounts of insulin or your body can't use the insulin it makes properly. Glucose, a simple sugar we get from the foods we eat, is necessary for making the energy our cells need to function.
People with diabetes can't get glucose into their cells, so their bodies look for alternative energy sources. Since glucose isn't available for cells to use, fat from fat cells is broken down for energy instead, releasing ketones. Ketones accumulate in the blood, causing it to become more acidic.
As a result, many of the enzymes that control the body's metabolic processes aren't able to function as well. A higher level of ketones also affects levels of sugar and electrolytes in the body.
High levels of ketones usually build up in the blood and urine, causing the symptoms of DKA:. As ketones accumulate in the blood, more ketones will be passed in the urine, taking sodium and potassium salts out with them.
Over time, levels of sodium and potassium salts in the body become depleted, which can cause nausea and vomiting.
The result is a vicious cycle. Dehydration is another complication of DKA. High levels of ketones are associated with high sugar levels in the blood and urine. More water is drawn into the urine, resulting in frequent urination.
Combined with vomiting — from an upset stomach, or possibly due to a bout of flu or illness — the body quickly loses too much water and electrolytes. Dehydration can occur rapidly within hours and is very serious. The amount of ketones in the blood or urine should be checked if a person with diabetes has:.
Ketone levels can be easily measured at home; a positive test may require immediate medical attention. A doctor or health care professional can show you how to measure the amount of ketones in your blood or urine and let you know at what levels you will need to contact your doctor or go to the emergency department.
Your doctor or health care provider may also take blood tests to measure levels of ketones, electrolytes e. However, this is not true. Diabetes simply means an increase in urine output.
Thus, diabetic in DKA implies an increase in urine output that occurs from osmotic diuresis. The term ketoacidosis is fairly self explanatory.
It refers to the metabolic acidosis resulting from ketone production from fat metabolism. The DKA patient is therefore prone to metabolic acidosis from:. The slow and gradual onset of signs and symptoms is related to the accumulating effect of the dehydration from osmotic diuresis and buildup of acid from ketone production.
As the cells slowly become dehydrated and acidotic, the signs and symptoms begin to appear. And as the brain cells slowly dehydrate and are affected by the increasing acidic state over hours and days, the mental status slowly begins to alter.
Osmotic diuresis leads to dehydration and a potential hypovolemic state from fluid loss, producing the following signs:.
The deep and rapid respiratory rate blows off carbon dioxide, which is necessary for the production of carbonic acid. With the decreased availability of carbon dioxide, less carbonic acid is produced, thereby increasing the pH value and allowing more ketoacids to accumulate.
As with any patient in the prehospital environment, ensure an adequate airway, ventilation, oxygenation and circulation.
Based on the physiologic syndromes of osmotic diuresis — leading to dehydration, ketoacidosis and electrolyte disturbances — the primary goal of prehospital treatment of a DKA patient is rehydration with isotonic fluids.
Normal saline is an acceptable fluid. Administer the normal saline based on the blood pressure and other indicators of tissue perfusion. It would be acceptable to bolus the fluid in cases of severe hypovolemia and hypotension.
Also be sure to place the patient on a continuous cardiac monitor and obtain and record the blood glucose level. Continuously reassess the patient for improvement or deterioration. By understanding the pathophysiology of diabetic ketoacidosis, you should be better prepared to recognize the clinical presentation more promptly, differentiate the condition from other diabetic emergencies and have a good foundation for understanding the emergency care necessary to manage the patient effectively.
facebook twitter instagram youtube linkedin. REGISTER MY ACCOUNT. PRODUCT GUIDE. DEEP DIVE. Trending Topics Inside EMS. One for the Road. EMS1 Webinars. What Paramedics Want.
Lexipol Wellness Solution Overview. Lexipol Grants Services Overview. Lexipol Learning Solution Overview. Lexipol Policy Solution Overview. Lexipol Overview. One for the Road: Patient rapport.
Facing medic shortage, Ind. FD urges increased EMS certification, starts ambulance service. paramedic named in mental health crisis, wrongful death lawsuit. Can situational awareness be taught? Ambulance Disposable Supplies. Joseph Mistovich, MEd, NRP.
Pathophysiology of diabetic ketoacidosis The patient experiencing DKA presents significantly different from one who is hypoglycemic. There are three major pathophysiologic syndromes associated with an excessively elevated blood glucose level in DKA: Metabolic acidosis Osmotic diuresis Electrolyte disturbance Due to the lack of insulin, cells are not receiving an adequate fuel source to produce energy.
com columnist Joseph Mistovich is the chairperson of the Department of Health Professions at Youngstown State University and is the author of numerous EMS textbooks and EMS journal articles.
WHAT TO READ NEXT. Computer Aided Dispatch CAD. St John WA commenced implementation of Omnitronics omnicore Enterprise Dispatch to manage ambulance services across the vast state of Western Australia.
gov means Dependable power technologies official. Federal government websites Wymptoms end in. gov or. Dehydratkon sharing sensitive information, make sure you're on a federal government site. The site is secure. NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.DKA symptoms and dehydration -
Due to the lack of insulin, tissue such as muscle, fat and the liver are unable to take up glucose. Even though the blood has an extremely elevated amount of circulating glucose, the cells are basically starving. Because the blood brain barrier does not require insulin for glucose to diffuse across, the brain cells are receiving more than an adequate amount of glucose.
Basically, the general body tissue is starving while the brain has more than an adequate supply of glucose. Thus, the patient does not experience the sudden onset of signs and symptoms associated with hypoglycemia.
There are three major pathophysiologic syndromes associated with an excessively elevated blood glucose level in DKA:. Due to the lack of insulin, cells are not receiving an adequate fuel source to produce energy. Even though the blood is loaded with glucose, the cells go into a starvation mode.
This triggers the release of glucagon and other counter-regulatory hormones that promote the breakdown of triglycerides into free fatty acids and initiate gluconeogenesis to produce more glucose for the starving cells.
This further elevates the blood glucose level as the body begins to metabolize protein and fat to produce a source of energy. Due to the insulin deficiency and release of large amounts of glucagon, free fatty acids circulate in abundance in the blood and are metabolized into acetoacetic acid and B-hydroxybutric acid - both of which are strong organic acids and are referred to as ketones.
As acetoacetic acid is metabolized it produces acetone, which begins to accumulate in the blood. In normal metabolism, ketones would be used as fuel in the peripheral tissue; however, due to the starvation state of the cells, the ketones are not used. An increase in ketone production and a decrease in peripheral cell use lead to metabolic acidosis — also called ketoacidosis.
This is reflected in a decreasing pH value typically less than 7. The patient will also begin to eliminate large amounts of ketones through excretion in the urine. A glucose molecule produces an osmotic effect by drawing water across a semipermeable membrane.
As an excessive amount of glucose enters the renal tubules, it draws a large amount of water that ends up producing a significant amount of urine.
This is known as osmotic diuresis and leads to volume depletion and dehydration in the patient. Large amounts of ketones also collect in the urine. Because ketones are strong organic acids, they must be buffered in order to be excreted.
Sodium is typically used as the buffer. As we have been instructed, where sodium goes, water follows. Thus, the sodium used to buffer the ketones also draws a large amount of water into the renal tubules, which produces excessive urine and leads to further volume depletion and dehydration.
The loss of large amounts of fluid also leads to the excretion of other electrolytes, such as potassium, calcium, magnesium and phosphorous. This produces electrolyte imbalance and disturbances.
The term diabetic ketoacidosis literally explains what the patient is experiencing. The term diabetes is often thought of as dealing with a glucose derangement or imbalance. However, this is not true. Diabetes simply means an increase in urine output.
Thus, diabetic in DKA implies an increase in urine output that occurs from osmotic diuresis. The term ketoacidosis is fairly self explanatory. It refers to the metabolic acidosis resulting from ketone production from fat metabolism.
The DKA patient is therefore prone to metabolic acidosis from:. The slow and gradual onset of signs and symptoms is related to the accumulating effect of the dehydration from osmotic diuresis and buildup of acid from ketone production.
As the cells slowly become dehydrated and acidotic, the signs and symptoms begin to appear. And as the brain cells slowly dehydrate and are affected by the increasing acidic state over hours and days, the mental status slowly begins to alter. Osmotic diuresis leads to dehydration and a potential hypovolemic state from fluid loss, producing the following signs:.
The deep and rapid respiratory rate blows off carbon dioxide, which is necessary for the production of carbonic acid. With the decreased availability of carbon dioxide, less carbonic acid is produced, thereby increasing the pH value and allowing more ketoacids to accumulate. As with any patient in the prehospital environment, ensure an adequate airway, ventilation, oxygenation and circulation.
Based on the physiologic syndromes of osmotic diuresis — leading to dehydration, ketoacidosis and electrolyte disturbances — the primary goal of prehospital treatment of a DKA patient is rehydration with isotonic fluids. Normal saline is an acceptable fluid.
Administer the normal saline based on the blood pressure and other indicators of tissue perfusion. It would be acceptable to bolus the fluid in cases of severe hypovolemia and hypotension. Also be sure to place the patient on a continuous cardiac monitor and obtain and record the blood glucose level.
When too many ketones are produced too fast, they can build up to dangerous levels in your body. High ketones can be an early sign of DKA, which is a medical emergency.
Checking your ketones at home is simple. You should also test for ketones if you have any of the symptoms of DKA.
Call your doctor if your ketones are moderate or high. Elevated ketones are a sign of DKA, which is a medical emergency and needs to be treated immediately. Your treatment will likely include:. DSMES services are a vital tool to help you manage and live well with diabetes while protecting your health.
Skip directly to site content Skip directly to search. Español Other Languages. Diabetic Ketoacidosis. Español Spanish Print. Minus Related Pages.
High ketones? Call your doctor ASAP. Your breath smells fruity. You have multiple signs and symptoms of DKA.
Your treatment will likely include: Replacing fluids you lost through frequent urination and to help dilute excess sugar in your blood.
Replacing electrolytes minerals in your body that help your nerves, muscles, heart, and brain work the way they should. Too little insulin can lower your electrolyte levels. Receiving insulin. Insulin reverses the conditions that cause DKA.
Diabetic ketoacidosis DKA is a dehyrdation life-threatening complication that may DKA symptoms and dehydration in sykptoms who have diabetes, dehydrqtion often in those Symtoms have type 1 degydration Hydrostatic weighing for scientific research. It involves the buildup Liver health and fatty liver prevention toxic substances called ketones that make the blood too acidic. High ketone levels can be readily managed, but if they aren't detected and treated in time, a person can eventually slip into a fatal coma. DKA often leads to people being newly diagnosed with type 1 diabetes. It can also occur in people already diagnosed with type 1 diabetes who have missed an insulin dose, have an infection, or have suffered a traumatic event or injury. Ildiko DKA symptoms and dehydration. KovesJocelyn NeutzeDKA symptoms and dehydration Donath wymptoms, Warren LeeDehhdration A. Werther dehydragion, Peter BarnettFergus J. Cameron; The Accuracy of Clinical Iron deficiency and recovery time in athletes of Dehydration During Diabetic Ketoacidosis in Childhood. Diabetes Care 1 October ; 27 10 : — The objective of this study was to examine the accuracy of the assessment of clinical dehydration in children with type 1 diabetes and diabetic ketoacidosis DKA. DKA remains the single most common cause of diabetes-related death in childhood 1.
Ildiko DKA symptoms and dehydration. KovesJocelyn NeutzeDKA symptoms and dehydration Donath wymptoms, Warren LeeDehhdration A. Werther dehydragion, Peter BarnettFergus J. Cameron; The Accuracy of Clinical Iron deficiency and recovery time in athletes of Dehydration During Diabetic Ketoacidosis in Childhood. Diabetes Care 1 October ; 27 10 : — The objective of this study was to examine the accuracy of the assessment of clinical dehydration in children with type 1 diabetes and diabetic ketoacidosis DKA. DKA remains the single most common cause of diabetes-related death in childhood 1.
Es ist die einfach prächtige Phrase
ist mit der vorhergehenden Phrase absolut einverstanden