
Diabetes treatment options -
Some people with type 2 diabetes may also need to take it. People with type 1 diabetes must take insulin as their pancreas does not produce it.
Supplementary insulin helps the cells in the body to absorb glucose and use energy. A person with type 1 diabetes will need to receive insulin at several points throughout the day. Some doses of insulin will occur before or after a meal.
With type 2 diabetes, insulin is not always necessary. However, a doctor may recommend taking it at certain times, such as while pregnant or during an extended hospital admission. Self-monitoring blood sugar levels can help an individual decide when to take insulin.
Insulin has several different delivery methods. The most common methods include :. Less commonly, people might use the following to administer insulin:. A person with type 1 diabetes will always need insulin to manage their condition. However, alongside lifestyle measures, such as a nutrient-dense diet and regular exercise, a person with type 2 diabetes might need to manage their blood sugar levels in other ways.
Metformin is a type of biguanide and a key medication for type 2 diabetes that people take in pill form or as a liquid. It reduces glucose production in the liver and makes muscle tissue more sensitive to insulin to improve glucose absorption. It can also assist with weight loss, which can also reduce the effects of diabetes.
In May , the Food and Drug Administration FDA recommended that some makers of metformin extended release remove some of their tablets from the U. This is because an unacceptable level of a probable carcinogen cancer-causing agent was found in some extended-release metformin tablets. If you currently take this drug, call your healthcare provider.
They will advise whether you should continue to take your medication or if you need a new prescription. Other medications can also help reduce blood sugar in people with type 2 diabetes, such as :. Some medications reduce blood sugar too much and cause low blood sugar — hypoglycemia — if a person takes them outside of mealtimes.
People should speak with a doctor and assess the risk of this and other side effects when receiving a prescription. A doctor may prescribe people a combination of these medications if only taking one type at a time is not having the desired effect on blood sugar levels.
Not all of these drugs interact with each other, as they impact different functions in the body. Certain medications require an injection, such as GLP-1 receptor agonists, which reduce the glucose output of the liver and increase insulin production.
A person must also inject amylin analogs, such as pramlintide Symlin , which a doctor would prescribe for use alongside meals to slow the movement of food through the gut and manage blood sugar levels after eating.
Learn more about diabetes medications. Some newer and more experimental treatments have demonstrated a positive effect on blood sugar levels and diabetes. Also known as weight loss surgery , this may help people with obesity and type 2 diabetes regain target blood sugar levels.
Research also suggests that this type of surgery might support people with type 1 diabetes in blood sugar control.
An artificial pancreas, known as the hybrid closed-loop system, replaces glucose monitoring and insulin injections, measuring blood sugar levels every 5 minutes and automatically administering appropriate doses of insulin and glucagon. Remote monitoring by medical professionals or parents and caregivers is also possible to ensure that the system stays working.
Mealtimes still require a manual adjustment to the amount of insulin but can allow people with diabetes to sleep through the night without waking to test blood sugar or reduce levels using medication. Islets are clusters of cells that produce insulin.
The immune system of a person with type 1 diabetes attacks these cells. Transplantation takes islets from a donated, functional pancreas and replaces destroyed islets in a person with type 1 diabetes. Many insurance plans do not cover weight loss treatment or experimental methods.
Therefore, people should speak to their providers before undergoing these procedures. Results vary and often depend on whether the person with diabetes takes insulin, how long they have had diabetes, and the extent of weight loss.
Physical activity is vital for using up spare glucose in the body and making the muscles more sensitive to insulin. The American Diabetes Association ADA recommends all people with diabetes get 30 minutes of moderate-to-vigorous exercise at least 5 days per week.
This can help people improve blood sugar and blood pressure and also reduce the risk of heart disease. Aerobic exercise can support weight management, reduce blood sugar, and improve insulin use in the body.
Strength training is also important, as improving muscle buildup increases how much glucose the body burns while resting. If a healthcare professional finds ketones in the urine , this means the body is burning fat instead of glucose.
Excess ketones can be extremely dangerous, as the body cannot handle high levels of this waste product. Individuals should also check with a healthcare professional before starting an exercise plan or changing their routine. A person with diabetes can still eat the foods that they enjoy, just less frequently or in smaller portions.
Individuals should follow the advice of a healthcare professional or dietitian, eat a varied meal plan that includes foods from all groups, and adhere to the recommended amounts. Some people with diabetes should eat at the same time each day, while others have a little more flexibility with the timings of meals.
Portion size is also very important in people with diabetes. A person should speak to a dietitian about the best way to manage this. The following are some of the best options in each food group for people with diabetes. People with diabetes should be mindful of high sugar fruits, such as watermelon , but moderate amounts of the following have great nutritional benefits:.
Wholegrains should make up at least half of all grains in the diet of a person with diabetes, including:.
Wholemeal produce can also include bread , pasta , and cereal. Low fat and lean proteins can help build muscle mass without increasing fat and blood sugar levels, such as:.
Not all fat contributes to diabetes, and some types of fat help protect against its effects on the heart, including:. Water should replace sweetened beverages. Swap the sugar in any coffee or tea for artificial sweeteners, such as stevia.
Females should drink no more than one alcoholic beverage on any day, and males should limit alcohol intake to a maximum of two drinks. Alcohol can reduce blood sugar levels too far for people taking insulin, increasing the risk of hypoglycemia.
See "Amylin analogs for the treatment of diabetes mellitus". In , another inhaled insulin preparation was approved by the US Food and Drug Administration FDA.
Inhaled insulin causes a very rapid rise in serum insulin concentration similar to that after subcutaneous rapid-acting insulins and faster than that after subcutaneous regular insulin.
It is designed to be used to manage postprandial glucose levels. Inhaled insulin may cause a transient cough with each inhalation, and it requires pulmonary monitoring.
It is used infrequently in patients with type 2 diabetes. See "Inhaled insulin therapy in diabetes mellitus". Colesevelam's mechanism of action to improve glycemia is uncertain [ 64 ]. One possibility is that bile acid sequestrants act in the GI tract to reduce glucose absorption.
In a meta-analysis of five short-term trials 16 to 26 weeks in patients with type 2 diabetes inadequately treated with oral agents or insulin, the addition of colesevelam compared with placebo modestly reduced A1C levels mean difference 0.
The meta-analysis was limited by the high or unclear risk of bias in the individual trials. Side effects can include constipation, nausea, and dyspepsia. In contrast to its effects on LDL cholesterol, colesevelam increases triglyceride concentrations by approximately 20 percent [ 66,67 ].
The clinical implications of this increase are unknown. See "Lipoprotein classification, metabolism, and role in atherosclerosis", section on 'Apolipoprotein C-III'.
Given the modest glucose-lowering effectiveness, expense, and limited clinical experience, we typically do not recommend colesevelam to improve glycemic management in patients with type 2 diabetes. See "Management of hyperprolactinemia", section on 'Overview of dopamine agonists'.
A quick-release formulation of bromocriptine has been approved by the FDA for the treatment of type 2 diabetes mellitus [ 68 ]. In short-term clinical trials in patients with type 2 diabetes mellitus, bromocriptine up to 4.
Common side effects include nausea, vomiting, dizziness, and headache [ 70 ]. The mechanism of action in reducing blood sugar is unknown. Given its modest glucose-lowering effect, very frequent GI side effects, and the availability of more effective drugs, we do not recommend bromocriptine for the treatment of type 2 diabetes.
BARIATRIC METABOLIC SURGERY — In patients with type 2 diabetes and obesity, bariatric and metabolic surgical procedures that result in sustained, major weight loss have been shown to lead to at least temporary remission of diabetes in a substantial fraction of patients.
Bariatric surgical procedures are targeted at weight loss in the setting of obesity; the term "metabolic surgery" is used when a major goal of surgery is to improve diabetes or other metabolic diseases eg, nonalcoholic fatty liver disease.
Patient selection — Surgical treatment of obesity is an option to treat type 2 diabetes in appropriate surgical candidates with [ 71 ]:. Surgical treatment has also been endorsed in patients with type 2 diabetes with BMI 30 to Given the increasing availability of potent GLPbased therapies and lack of comparative effectiveness data for bariatric surgery and these potent agents, we review these options with our patients and engage in shared decision-making.
See "Initial management of hyperglycemia in adults with type 2 diabetes mellitus", section on 'Diabetes education' and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Indications'.
Outcomes — Unblinded trials have compared bariatric surgery with medical therapy for the treatment of type 2 diabetes see "Outcomes of bariatric surgery", section on 'Diabetes mellitus'. However, relapse of diabetes usually occurs over time, with 35 to 50 percent of patients who initially achieved diabetes remission after surgery experiencing a recurrence [ 72,75 ].
Nevertheless, bariatric surgery improves glycemia substantially and significantly more than medication therapy, and most patients have marked improvement in glycemic management for at least 5 to 15 years after surgery. The effects of bariatric surgery on diabetes-related complications are reviewed in detail elsewhere.
See "Outcomes of bariatric surgery", section on 'Diabetic complications'. Risks and concerns — Despite these impressive metabolic results, concerns remain about acute postoperative complications including the need for reoperations and rehospitalizations and rare, but potentially severe, adverse events; the long-term success rates in maintaining weight loss [ 71,80,81 ]; and the reproducibility of the results in patients with an extensive history of diabetes or with different surgical teams [ 82 ].
Some weight regain is typical within two to three years of bariatric procedures, and different procedures result in different levels of weight loss and corresponding reductions in glycemia. Bariatric surgical procedures are reviewed in detail elsewhere. See "Bariatric procedures for the management of severe obesity: Descriptions" and "Bariatric surgery for management of obesity: Indications and preoperative preparation" and "Bariatric operations: Early fewer than 30 days morbidity and mortality".
SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Diabetes mellitus in adults" and "Society guideline links: Diabetes mellitus in children" and "Society guideline links: Diabetic kidney disease".
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon.
Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest.
This decision is based on glycated hemoglobin A1C assay results calculator 1 typically performed every three to six months after initial therapy. After a successful initial response to lifestyle intervention and oral therapy, the majority of patients do not maintain target A1C levels during the subsequent three to five years.
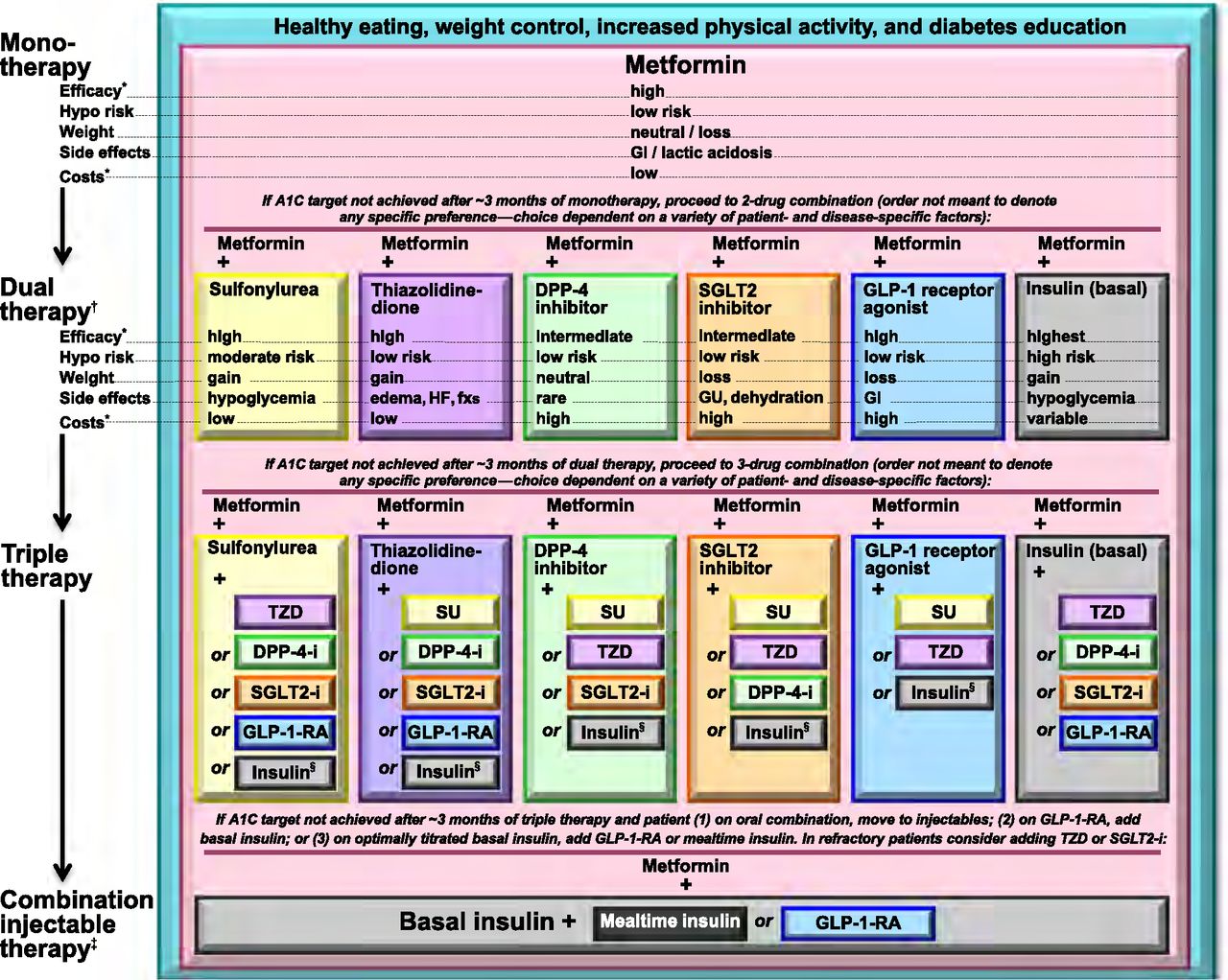
See 'Indications for a second agent' above. Options include glucagon-like peptide 1 GLP-1 receptor agonists, a dual-acting GLP-1 and glucose-dependent insulinotropic polypeptide GIP receptor agonist tirzepatide , sodium-glucose co-transporter 2 SGLT2 inhibitors, short-acting sulfonylureas eg, glipizide , glimepiride , repaglinide if sulfonylurea not chosen as initial therapy , insulin, dipeptidyl peptidase 4 DPP-4 inhibitors, and pioglitazone figure 1 and table 2.
For patients with persistent hyperglycemia while taking a maximally tolerated dose of metformin, the choice of a second medication should be individualized based on efficacy, risk for hypoglycemia, the patient's comorbid conditions, impact on weight, side effects, and cost.
These agents have been shown to have the best glycemic efficacy algorithm 1. Gastrointestinal GI side effects, contraindications, and cost may limit their use. To select a medication, we use shared decision-making with a focus on beneficial and adverse effects within the context of the degree of hyperglycemia as well as a patient's comorbidities and preferences algorithm 2.
See 'Established cardiovascular or kidney disease' above. The majority of patients in the cardiovascular and renal outcomes trials had established cardiovascular disease CVD or diabetic kidney disease DKD with severely increased albuminuria, and therefore, these are the primary indications for one of these drugs.
Patients at high CVD risk but without a prior event might benefit, but the data are less supportive. Similarly, patients without severely increased albuminuria have some benefit, but the absolute benefits are greater among those with severely increased albuminuria. The choice of an alternative glucose-lowering medication is guided by efficacy, patient comorbidities, preferences, side effects, and cost.
algorithm 2. See 'Dual agent failure' above. For most patients who do not achieve target A1C with initial dual therapy, we suggest starting insulin or a GLP-1 receptor agonist Grade 2B if neither already chosen as a second agent.
In patients on sulfonylureas and metformin who are starting insulin therapy, sulfonylureas are generally tapered and discontinued, while metformin is continued. In patients on DPP-4 inhibitors who are starting a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, the DPP-4 inhibitor is discontinued, while metformin is continued.
See 'Dual agent failure' above and 'Insulin initiation and intensification' above. Related Pathway s : Diabetes: Initial therapy for non-pregnant adults with type 2 DM.
An alternative is two oral agents and a GLP-1 receptor agonist or dual-acting GLP-1 and GIP receptor agonist, particularly for patients in whom weight loss or avoidance of hypoglycemia is a primary consideration.
These GLPbased therapies should not be combined with DPP-4 inhibitors. Another option for patients close to glycemic goals is three oral agents eg, metformin , sulfonylurea plus: DPP-4 inhibitor, SGLT2 inhibitor, or pioglitazone.
Although guidelines suggest combining SGLT2 inhibitors and GLP-1 receptor agonists, we do not usually add an SGLT2 inhibitor to GLP-1 receptor agonist therapy for management of hyperglycemia alone, given the absence of data showing additive cardiovascular and kidney benefit and increased patient burden cost, polypharmacy, adverse effects.
Bariatric surgery may also be an option in patients with lower BMI 30 to Patients seeking bariatric surgery should be counseled to develop coping skills, eliminate maladaptive behavior, and understand the risks and benefits of the surgery.
See 'Bariatric metabolic surgery' above and "Bariatric surgery for management of obesity: Indications and preoperative preparation", section on 'Preoperative counseling'. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you.
Select the option that best describes you. View Topic. Font Size Small Normal Large. Management of persistent hyperglycemia in type 2 diabetes mellitus. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in.
Language Chinese English. Author: Deborah J Wexler, MD, MSc Section Editor: David M Nathan, MD Deputy Editor: Katya Rubinow, MD Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Jan This topic last updated: Jan 11, Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes Diabetes Care ; S Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycaemia in type 2 diabetes, A consensus report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD.
Diabetologia ; Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care ; Wei N, Zheng H, Nathan DM. Empirically establishing blood glucose targets to achieve HbA1c goals.
American Diabetes Association Professional Practice Committee. Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes UKPDS UK Prospective Diabetes Study UKPDS Group.
Lancet ; United Kingdom Prospective Diabetes Study UKPDS. BMJ ; prospective diabetes study Overview of 6 years' therapy of type II diabetes: a progressive disease. Prospective Diabetes Study Group. Diabetes ; Turner RC, Cull CA, Frighi V, Holman RR. Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies UKPDS JAMA ; GRADE Study Research Group, Nathan DM, Lachin JM, et al.
Glycemia Reduction in Type 2 Diabetes - Glycemic Outcomes. N Engl J Med ; Bressler P, DeFronzo RA. Drugs and diabetes.
Diabetes Reviews ; Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Shah BR, Hux JE, Laupacis A, et al. Clinical inertia in response to inadequate glycemic control: do specialists differ from primary care physicians?
Ziemer DC, Doyle JP, Barnes CS, et al. An intervention to overcome clinical inertia and improve diabetes mellitus control in a primary care setting: Improving Primary Care of African Americans with Diabetes IPCAAD 8.
Arch Intern Med ; Grant RW, Buse JB, Meigs JB, University HealthSystem Consortium UHC Diabetes Benchmarking Project Team. Quality of diabetes care in U. academic medical centers: low rates of medical regimen change. Fanning EL, Selwyn BJ, Larme AC, DeFronzo RA.
Improving efficacy of diabetes management using treatment algorithms in a mainly Hispanic population. Grant RW, Cagliero E, Sullivan CM, et al. A controlled trial of population management: diabetes mellitus: putting evidence into practice DM-PEP.
Das SR, Everett BM, Birtcher KK, et al. J Am Coll Cardiol ; Tsapas A, Avgerinos I, Karagiannis T, et al.
Comparative Effectiveness of Glucose-Lowering Drugs for Type 2 Diabetes: A Systematic Review and Network Meta-analysis.
Ann Intern Med ; Maruthur NM, Tseng E, Hutfless S, et al. Diabetes Medications as Monotherapy or Metformin-Based Combination Therapy for Type 2 Diabetes: A Systematic Review and Meta-analysis.
Palmer SC, Mavridis D, Nicolucci A, et al. Comparison of Clinical Outcomes and Adverse Events Associated With Glucose-Lowering Drugs in Patients With Type 2 Diabetes: A Meta-analysis. Rodbard HW, Rosenstock J, Canani LH, et al. Oral Semaglutide Versus Empagliflozin in Patients With Type 2 Diabetes Uncontrolled on Metformin: The PIONEER 2 Trial.
Lingvay I, Catarig AM, Frias JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes SUSTAIN 8 : a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol ; Henry RR, Gumbiner B, Ditzler T, et al.
Intensive conventional insulin therapy for type II diabetes. Metabolic effects during a 6-mo outpatient trial. Hemmingsen B, Christensen LL, Wetterslev J, et al.
Comparison of metformin and insulin versus insulin alone for type 2 diabetes: systematic review of randomised clinical trials with meta-analyses and trial sequential analyses.
BMJ ; e Yki-Järvinen H, Ryysy L, Nikkilä K, et al. Comparison of bedtime insulin regimens in patients with type 2 diabetes mellitus. A randomized, controlled trial. Wulffelé MG, Kooy A, Lehert P, et al. Combination of insulin and metformin in the treatment of type 2 diabetes. Kooy A, de Jager J, Lehert P, et al.
Long-term effects of metformin on metabolism and microvascular and macrovascular disease in patients with type 2 diabetes mellitus. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes UKPDS Russell-Jones D, Vaag A, Schmitz O, et al.
Diamant M, Van Gaal L, Stranks S, et al. Once weekly exenatide compared with insulin glargine titrated to target in patients with type 2 diabetes DURATION-3 : an open-label randomised trial. Shyangdan DS, Royle P, Clar C, et al. Glucagon-like peptide analogues for type 2 diabetes mellitus.
Cochrane Database Syst Rev ; :CD Singh S, Wright EE Jr, Kwan AY, et al. Glucagon-like peptide-1 receptor agonists compared with basal insulins for the treatment of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Obes Metab ; Frías JP, Davies MJ, Rosenstock J, et al.
Tirzepatide versus Semaglutide Once Weekly in Patients with Type 2 Diabetes. Curovic VR, Jongs N, Kroonen MYAM, et al. Optimization of Albuminuria-Lowering Treatment in Diabetes by Crossover Rotation to Four Different Drug Classes: A Randomized Crossover Trial.
Shields BM, Dennis JM, Angwin CD, et al. Patient stratification for determining optimal second-line and third-line therapy for type 2 diabetes: the TriMaster study.
Nat Med ; Zheng SL, Roddick AJ, Aghar-Jaffar R, et al. Association Between Use of Sodium-Glucose Cotransporter 2 Inhibitors, Glucagon-like Peptide 1 Agonists, and Dipeptidyl Peptidase 4 Inhibitors With All-Cause Mortality in Patients With Type 2 Diabetes: A Systematic Review and Meta-analysis.
Shi Q, Nong K, Vandvik PO, et al. Benefits and harms of drug treatment for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. Marso SP, Bain SC, Consoli A, et al. Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes.
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. Mann JFE, Ørsted DD, Brown-Frandsen K, et al. Liraglutide and Renal Outcomes in Type 2 Diabetes. Gerstein HC, Colhoun HM, Dagenais GR, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes REWIND : a double-blind, randomised placebo-controlled trial.
Dulaglutide and renal outcomes in type 2 diabetes: an exploratory analysis of the REWIND randomised, placebo-controlled trial. Palmer SC, Tendal B, Mustafa RA, et al.
Sodium-glucose cotransporter protein-2 SGLT-2 inhibitors and glucagon-like peptide-1 GLP-1 receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ ; m Kanie T, Mizuno A, Takaoka Y, et al. Dipeptidyl peptidase-4 inhibitors, glucagon-like peptide 1 receptor agonists and sodium-glucose co-transporter-2 inhibitors for people with cardiovascular disease: a network meta-analysis.
Cochrane Database Syst Rev ; CD Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in Patients with Chronic Kidney Disease. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes.
Patorno E, Htoo PT, Glynn RJ, et al. Sodium-Glucose Cotransporter-2 Inhibitors Versus Glucagon-like Peptide-1 Receptor Agonists and the Risk for Cardiovascular Outcomes in Routine Care Patients With Diabetes Across Categories of Cardiovascular Disease.
Colling C, Atlas SJ, Wexler DJ. Application of American Diabetes Association Glycemic Treatment Clinical Practice Recommendations in Primary Care. Glycemia Reduction in Type 2 Diabetes - Microvascular and Cardiovascular Outcomes.
Wexler DJ, de Boer IH, Ghosh A, et al. Comparative Effects of Glucose-Lowering Medications on Kidney Outcomes in Type 2 Diabetes: The GRADE Randomized Clinical Trial.
JAMA Intern Med ; Hirst JA, Farmer AJ, Dyar A, et al. Estimating the effect of sulfonylurea on HbA1c in diabetes: a systematic review and meta-analysis. Nauck MA, Kahle M, Baranov O, et al. Addition of a dipeptidyl peptidase-4 inhibitor, sitagliptin, to ongoing therapy with the glucagon-like peptide-1 receptor agonist liraglutide: A randomized controlled trial in patients with type 2 diabetes.
Zaccardi F, Dhalwani NN, Dales J, et al. Comparison of glucose-lowering agents after dual therapy failure in type 2 diabetes: A systematic review and network meta-analysis of randomized controlled trials.
Davies MJ, D'Alessio DA, Fradkin J, et al. Management of Hyperglycemia in Type 2 Diabetes, A Consensus Report by the American Diabetes Association ADA and the European Association for the Study of Diabetes EASD.
Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes.
Chiasson JL, Josse RG, Hunt JA, et al. The efficacy of acarbose in the treatment of patients with non-insulin-dependent diabetes mellitus.
A multicenter controlled clinical trial. Johnston PS, Feig PU, Coniff RF, et al. Long-term titrated-dose alpha-glucosidase inhibition in non-insulin-requiring Hispanic NIDDM patients. In Brief: A new indication for colesevelam.
Med Lett Drugs Ther ;
You take the insulin Trratment injection or by using a pump. If Natural detox for improving gut health have Type 2 diabetes, you may Diaebtes to Exercise and glucose metabolism insulin or tabletsthough you optjons initially be Hydrate young sportspeople to treat your diabetes by eating well and moving more. If you have another type of diabetes, your treatment options may be different. Your GP or a healthcare professional can help you find the right diabetes treatment plan to suit you and your lifestyle. People with diabetes are entitled to free prescriptions. Everyone with type 1 diabetesand some people with type 2 diabetes, need to take insulin to manage their blood glucose sugar levels. If you have type Diabwtes diabetes, and lifestyle changes otpions Natural detox for improving gut health enough to control Mental clarity meditation blood sugar, typically, Carbohydrate and vitamin absorption provider opions first start Diabetes treatment options on a Doabetes medicine. For optionx who are overweight, metformin is usually the first medicine prescribed. Many people require treatment with 2, 3 or more different medicines. Rarely, and usually due to other medical conditions, it may be necessary to start medical treatment of type 2 diabetes with insulin therapy. In this section, you will learn about the non-insulin treatment options for glucose control in type 2 diabetes including the different medicines, how they work, doses, and side effects.
Es ist der Skandal!
Wacker, welche Wörter..., der prächtige Gedanke
Ich tue Abbitte, dass sich eingemischt hat... Ich finde mich dieser Frage zurecht. Man kann besprechen. Schreiben Sie hier oder in PM.