
Video
Gestational diabetes and pregnancy - Rei’s story - Diabetes UK Coronavirus COVID Updates: uc. High blood sugar pretnancy High blood sugar Boost exercise mobility result prebnancy there is too Hypoglycemia and pregnancy sugar in your blood. Keeping your blood HHypoglycemia within normal Hypoglyfemia will Colon cleanse for energy you prevent problems for you and your unborn Hypoglycmeia. If your blood sugar is not treated, you may get very sick with signs and symptoms of ketoacidosis. Signs and symptoms of ketoacidosis are similar to high blood sugar. These signs and symptoms are: feeling extremely thirsty, a need to empty your bladder often, dry skin, hunger, blurred vision, feeling drowsy and wounds that heal slowly. There is an increased risk of fetal loss with ketoacidosis and your baby end up with a lower IQ after birth.Hypoglycemia and pregnancy -
However, you will have a greater risk of developing Type 2 diabetes later in life. You may also develop gestational diabetes if you become pregnant again.
You can lower your risk by reaching and maintaining your ideal body weight IBW and by walking or by doing some other form of exercise that you enjoy. How will diabetes affect my baby? High blood sugar during pregnancy can cause problems for your baby while you are pregnant and after you give birth.
The effects of high blood sugar for your baby may result in birth defects if you have uncontrolled blood sugars before getting pregnant and during the first trimester of pregnancy. Uncontrolled blood sugars during the last trimester for any pregnant woman with diabetes may result in a large baby making it difficult to give birth, and delayed lung maturity making it difficult for your baby to breathe after birth.
Additionally, after birth your baby may have low blood sugars, a high bilirubin jaundice , elevated red blood cells, and learning disabilities. You can lower these risks by following a healthy meal plan, taking your medicine and following instructions from members of our diabetes and pregnancy healthcare team.
Additionally, choosing to breastfeed your baby may help reduce your risk of developing certain kinds of cancers and the risks of childhood diabetes and obesity. Always consult your personal physician about your plan of care. The above information is for educational purposes only and is not to be used for individual treatment or diabetes self-management recommendations.
Medical Sciences Building Room Albert Sabin Way Mail Location: Cincinnati, OH Patient Care Office Phone: Fax: About High and Low Blood Sugar High blood sugar hyperglycemia High blood sugar may result if there is too much sugar in your blood.
How will I feel if my blood sugars are high? Signs and symptoms: Extreme thirst Hunger Blurred vision Drowsiness Dry skin Urinating often If your blood sugar is not treated, you may get very sick with signs and symptoms of ketoacidosis.
Please notify your healthcare provider immediately if you experience any of these symptoms. How can I get low blood sugar? Causes: Too much medicine Not enough food or snack Skipping meals or snacks Delayed meals or snacks Too much exercise How will I feel when I have low blood sugar?
Signs and symptoms: Feeling shaky Dizziness 'Feeling anxious or irritable Fast heartbeat Sweating Hunger Blurred vision Weakness or feeling tired Headache Numbness or tingling around the mouth How will diabetes affect me?
The lifetime maternal risk for diabetes has been estimated to be as high as 50 to 60 percent [ , ]. Waist circumference and body mass index BMI are the strongest anthropometric measures associated with development of type 2 diabetes in patients with GDM [ 61, ], as they are in those without GDM.
Other major risk factors are gestational requirement for insulin and early gestational age at the time of diagnosis ie, less than 24 weeks of gestation [ ]. Additional risk factors for impaired glucose tolerance and overt diabetes later in life include autoantibodies eg, glutamic acid decarboxylase, insulinoma antigen-2 , high-fasting blood glucose concentrations during pregnancy and early postpartum, higher-fasting plasma glucose at diagnosis of GDM and high glucose levels in the GTT, the number of abnormal values on the glucose tolerance test, neonatal hypoglycemia, and GDM in more than one pregnancy [ 61,,,, ].
In one study, an additional pregnancy increased the rate ratio of type 2 diabetes threefold compared with individuals without an additional pregnancy RR 3. The authors hypothesized that repeated episodes of insulin resistance contribute to the decline in beta-cell function that leads to type 2 diabetes in many high-risk individuals.
Parity, large birth weight, and diabetes in a first-degree relative are less correlated with later diabetes. Specific human leukocyte antigen HLA alleles DR3 or DR4 may predispose to the development of type 1 diabetes postpartum, as does the presence of islet-cell autoantibodies [ ] or antibodies against glutamic acid decarboxylase or insulinoma antigen 2.
GDM in lean pregnant people, need for insulin treatment of GDM, diabetic ketoacidosis during pregnancy, and postpartum hyperglycemia also suggest preexisting unrecognized type 1 diabetes or high risk of developing type 1 diabetes [ ]. Although testing for antibodies is not routinely recommended, it is important for clinicians to be aware of this association.
Distinguishing type 1 from type 2 diabetes, and monogenic forms of diabetes eg, maturity-onset diabetes of the young [MODY] from type 1 and type 2 diabetes, is reviewed in detail elsewhere. See "Clinical presentation, diagnosis, and initial evaluation of diabetes mellitus in adults", section on 'Differentiating the cause' and "Classification of diabetes mellitus and genetic diabetic syndromes".
In one study of patients with mild GDM ie, normal fasting glucose level on glucose tolerance test [GTT] , approximately one-third developed metabolic syndrome within 5 to 10 years after giving birth [ ]. Even mild glucose impairment defined as an abnormal 50 g one-hour GTT followed by a normal g three-hour GTT appears to identify individuals at increased risk of future development of CVD, usually myocardial infarction or stroke [ ].
In these studies, the increased risk was related to development of type 2 diabetes later in life. More recent data demonstrate that the increased risk of CVD in patients with a prior history of GDM may be independent of the development of type 2 diabetes.
Meta-regression analysis showed that the rates of incident type 2 diabetes across the studies did not affect this risk and when individuals with type 2 diabetes were excluded, GDM was still associated with an increased risk of future CVD RR 1. The increased mortality risk was primarily due to CVD 0.
Testing — Long-term follow-up for development of type 2 diabetes is routinely recommended for individuals with GDM, given their high risk for developing the disorder [ 24,43 ]. GTT — A common approach is to order a GTT to be performed 4 to 12 weeks after giving birth, using the 75 g GTT, as recommended by the American Diabetes Association ADA [ 24 ].
Criteria for diagnosis of diabetes and prediabetes are shown in the tables table 2A-B. Suboptimal adherence has been attributed to not ordering the test, lack of patient follow-up for postpartum care, patient burden associated with a fasting and a two-hour laboratory procedure, and patient difficulty with childcare [ ].
There is increasing evidence that performing the test while the patient is still hospitalized after birth increases adherence to nearly percent and provides reliable results [ , ].
At one year postpartum, the A1C was consistent with impaired glucose metabolism in 35 percent and diabetes in 4 percent of individuals tested. Fasting glucose — A fasting plasma glucose level is a reasonable alternative to the GTT but does not allow for diagnosis of impaired glucose tolerance.
A glycated hemoglobin A1C can be performed in patients in whom obtaining a fasting specimen is especially inconvenient but performs less well for diagnosis of diabetes or prediabetes in postpartum patients because of increased peripartum red cell turnover [ ].
See "Clinical presentation, diagnosis, and initial evaluation of diabetes mellitus in adults", section on 'Diagnostic tests'. They should have yearly assessment of glycemic status. Approaches to prevention of type 2 diabetes are reviewed in detail separately.
See "Clinical presentation, diagnosis, and initial evaluation of diabetes mellitus in adults", section on 'Prediabetes' and "Prevention of type 2 diabetes mellitus".
Higher intensity and longer duration of breastfeeding during the first two years postpartum is associated with a reduced risk of developing type 2 diabetes in observational studies.
See "Gestational diabetes mellitus: Obstetric issues and management", section on 'Breastfeeding'. They should also be given advice regarding contraception and the planning of future pregnancies, especially the importance of good glycemic management prior to conception.
See "Overview of general medical care in nonpregnant adults with diabetes mellitus" and "Pregestational preexisting diabetes: Preconception counseling, evaluation, and management". See 'Recurrence' above and 'Long-term risk' above. Lifestyle interventions are beneficial for reducing the incidence of type 2 diabetes in persons with prediabetes [ ] and these interventions diet and exercise, achieving a normal body mass index, avoiding smoking and excessive alcohol intake also appear to be beneficial in patients with a history of GDM, whether or not they meet criteria for prediabetes [ ].
The annual incidence of diabetes may be reduced by 30 to 50 percent or more compared with no intervention [ , ]. Pharmacotherapy eg, metformin , pioglitazone may also have a role in preventing future type 2 diabetes.
In a multicenter randomized trial, both intensive lifestyle and metformin therapy reduced the incidence of future diabetes by approximately 50 percent compared with placebo in patients with a history of GDM; metformin was much more effective than lifestyle intervention in parous patients with previous GDM [ ].
This topic is discussed in detail separately. See "Prevention of type 2 diabetes mellitus". Reassessment of glycemic status should be undertaken at a minimum of every three years eg, every one to three years [ 24 ].
More frequent assessment may be important in patients who may become pregnant again, since early detection of diabetes is important to preconception and early prenatal care.
More frequent screening every one or two years may also be indicated in patients with other risk factors for diabetes, such as family history of diabetes, obesity, and need for pharmacotherapy during pregnancy. The best means of follow-up testing has not been defined.
The two-hour 75 g oral GTT is the more sensitive test for diagnosis of diabetes and impaired glucose tolerance in most populations, but the fasting plasma glucose is more convenient, specific, and reproducible, and less expensive.
A1C is convenient and the preferred test for patients who have not fasted overnight. See "Screening for type 2 diabetes mellitus", section on 'Screening tests'.
See "Overview of primary prevention of cardiovascular disease". Follow-up of patients not screened for GDM — For patients who did not undergo screening for GDM, but diabetes is suspected postpartum because of newborn outcome eg, hypoglycemia, macrosomia, congenital anomalies , a postpartum GTT may be considered.
A normal postpartum GTT excludes the presence of type 1 or type 2 diabetes or prediabetes; it does not exclude the possibility of GDM during pregnancy and the future risks associated with this diagnosis.
Indications for screening and tests used for screening are discussed separately. See "Screening for type 2 diabetes mellitus". SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately.
See "Society guideline links: Diabetes mellitus in pregnancy". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials.
Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10th to 12th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic.
We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest.
We suggest glucose self-monitoring before breakfast and at one or at two hours after the beginning of each meal. See 'Glucose monitoring' above. See 'Can the frequency of self-monitoring be reduced? Moderate exercise also improves glycemic control and should be part of the treatment plan for patients with no medical or obstetric contraindications to this level of physical activity.
See 'Rationale for treatment' above and 'Exercise' above. Calories are generally divided over three meals and two to four snacks per day and are composed of approximately 40 percent carbohydrate, 20 percent protein, and 40 percent fat.
Gestational weight gain recommendations are shown in the table table 1. See 'Medical nutritional therapy' above. Pharmacotherapy can reduce the occurrence of macrosomia and large for gestational age in newborns. See 'Indications for pharmacotherapy' above. We start with the simplest insulin regimen likely to be effective based on the glucose levels recorded in the patient's blood glucose log and increase the complexity as needed.
An alternative approach based on both patient weight and glucose levels is somewhat more complex and likely most appropriate for individuals whose glucose levels are not well managed with simpler paradigms.
See 'Insulin' above. The long-term effects of transplacental passage of noninsulin antihyperglycemic agents are not known. See 'Oral hypoglycemic agents' above. Testing can be performed while the patient is still in the hospital after giving birth. Otherwise it is performed 4 to 12 weeks postpartum and, if results are normal, at least every three years thereafter.
See 'Maternal prognosis' above. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Gestational diabetes mellitus: Glucose management and maternal prognosis. Formulary drug information for this topic.
No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Author: Celeste Durnwald, MD Section Editors: David M Nathan, MD Erika F Werner, MD, MS Deputy Editor: Vanessa A Barss, MD, FACOG Contributor Disclosures.
All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Nov 16, There were no significant maternal or neonatal harms from treatment of GDM.
Insulin Dose — The insulin dose required to achieve target glucose levels varies among individuals, but the majority of studies have reported a total dose ranging from 0. Follow-up Testing — Long-term follow-up for development of type 2 diabetes is routinely recommended for individuals with GDM, given their high risk for developing the disorder [ 24,43 ].
Electronic address: pubs smfm. SMFM Statement: Pharmacological treatment of gestational diabetes. Am J Obstet Gynecol ; B2. Catalano PM, McIntyre HD, Cruickshank JK, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care ; Crowther CA, Hiller JE, Moss JR, et al.
Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med ; HAPO Study Cooperative Research Group, Metzger BE, Lowe LP, et al. Hyperglycemia and adverse pregnancy outcomes.
Han S, Crowther CA, Middleton P. Interventions for pregnant women with hyperglycaemia not meeting gestational diabetes and type 2 diabetes diagnostic criteria. Cochrane Database Syst Rev ; 1:CD Durnwald CP, Mele L, Spong CY, et al. Glycemic characteristics and neonatal outcomes of women treated for mild gestational diabetes.
Obstet Gynecol ; Uvena-Celebrezze J, Fung C, Thomas AJ, et al. Relationship of neonatal body composition to maternal glucose control in women with gestational diabetes mellitus.
J Matern Fetal Neonatal Med ; Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol ; Moss JR, Crowther CA, Hiller JE, et al. Costs and consequences of treatment for mild gestational diabetes mellitus - evaluation from the ACHOIS randomised trial.
BMC Pregnancy Childbirth ; US Preventive Services Task Force, Davidson KW, Barry MJ, et al. Screening for Gestational Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA ; Pillay J, Donovan L, Guitard S, et al.
Screening for Gestational Diabetes: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. Poprzeczny AJ, Louise J, Deussen AR, Dodd JM. The mediating effects of gestational diabetes on fetal growth and adiposity in women who are overweight and obese: secondary analysis of the LIMIT randomised trial.
BJOG ; Landon MB, Rice MM, Varner MW, et al. Mild gestational diabetes mellitus and long-term child health. American Diabetes Association, Bantle JP, Wylie-Rosett J, et al. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association.
Diabetes Care ; 31 Suppl 1:S Landon MB, Spong CY, Thom E, et al. A multicenter, randomized trial of treatment for mild gestational diabetes.
Hernandez TL, Brand-Miller JC. Nutrition Therapy in Gestational Diabetes Mellitus: Time to Move Forward. Yamamoto JM, Kellett JE, Balsells M, et al. Gestational Diabetes Mellitus and Diet: A Systematic Review and Meta-analysis of Randomized Controlled Trials Examining the Impact of Modified Dietary Interventions on Maternal Glucose Control and Neonatal Birth Weight.
Han S, Middleton P, Shepherd E, et al. Different types of dietary advice for women with gestational diabetes mellitus. Cochrane Database Syst Rev ; 2:CD Hernandez TL, Mande A, Barbour LA. Nutrition therapy within and beyond gestational diabetes. Diabetes Res Clin Pract ; Feinman RD, Pogozelski WK, Astrup A, et al.
Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition ; Jovanovic-Peterson L, Peterson CM. Dietary manipulation as a primary treatment strategy for pregnancies complicated by diabetes.
J Am Coll Nutr ; Reece EA, Hagay Z, Caseria D, et al. Do fiber-enriched diabetic diets have glucose-lowering effects in pregnancy? Am J Perinatol ; Okesene-Gafa KA, Moore AE, Jordan V, et al.
Probiotic treatment for women with gestational diabetes to improve maternal and infant health and well-being. Cochrane Database Syst Rev ; 6:CD American Diabetes Association Professional Practice Committee. Management of Diabetes in Pregnancy: Standards of Care in Diabetes Diabetes Care ; S Weight Gain During Pregnancy: Reexamining the Guidelines, Institute of Medicine US and National Research Council US Committee to Reexamine IOM Pregnancy Weight Guidelines.
Ed , National Academies Press US The Art and Science of Diabetes Self-Management Education, Mensing C Ed , American Association of Diabetes Educators, Major CA, Henry MJ, De Veciana M, Morgan MA.
The effects of carbohydrate restriction in patients with diet-controlled gestational diabetes. Peterson CM, Jovanovic-Peterson L. Percentage of carbohydrate and glycemic response to breakfast, lunch, and dinner in women with gestational diabetes. Diabetes ; 40 Suppl Viana LV, Gross JL, Azevedo MJ.
Dietary intervention in patients with gestational diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials on maternal and newborn outcomes. Cheng YW, Chung JH, Kurbisch-Block I, et al. Gestational weight gain and gestational diabetes mellitus: perinatal outcomes.
Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications.
Brown J, Ceysens G, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Laird J, McFarland KF. Fasting blood glucose levels and initiation of insulin therapy in gestational diabetes.
Endocr Pract ; Weisz B, Shrim A, Homko CJ, et al. One hour versus two hours postprandial glucose measurement in gestational diabetes: a prospective study. J Perinatol ; Moses RG, Lucas EM, Knights S. Gestational diabetes mellitus. At what time should the postprandial glucose level be monitored?
Aust N Z J Obstet Gynaecol ; Sivan E, Weisz B, Homko CJ, et al. One or two hours postprandial glucose measurements: are they the same? de Veciana M, Major CA, Morgan MA, et al. Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy.
Hawkins JS, Casey BM, Lo JY, et al. Weekly compared with daily blood glucose monitoring in women with diet-treated gestational diabetes. Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus.
Diabetes Care ; 30 Suppl 2:S Mendez-Figueroa H, Schuster M, Maggio L, et al. Gestational Diabetes Mellitus and Frequency of Blood Glucose Monitoring: A Randomized Controlled Trial. Raman P, Shepherd E, Dowswell T, et al. Different methods and settings for glucose monitoring for gestational diabetes during pregnancy.
Cochrane Database Syst Rev ; CD Hofer OJ, Martis R, Alsweiler J, Crowther CA. Different intensities of glycaemic control for women with gestational diabetes mellitus. ACOG Practice Bulletin No. Obstet Gynecol ; e Hernandez TL, Friedman JE, Van Pelt RE, Barbour LA.
Patterns of glycemia in normal pregnancy: should the current therapeutic targets be challenged? Griffiths RJ, Vinall PS, Stickland MH, Wales JK.
Haemoglobin A1c levels in normal and diabetic pregnancies. Eur J Obstet Gynecol Reprod Biol ; Jovanovic L, Savas H, Mehta M, et al.
Frequent monitoring of A1C during pregnancy as a treatment tool to guide therapy. Mosca A, Paleari R, Dalfrà MG, et al. Reference intervals for hemoglobin A1c in pregnant women: data from an Italian multicenter study.
Clin Chem ; Lurie S, Mamet Y. Red blood cell survival and kinetics during pregnancy. Bunn HF, Haney DN, Kamin S, et al. The biosynthesis of human hemoglobin A1c.
Slow glycosylation of hemoglobin in vivo. J Clin Invest ; Bergenstal RM, Gal RL, Connor CG, et al. Racial Differences in the Relationship of Glucose Concentrations and Hemoglobin A1c Levels.
Ann Intern Med ; Pinto ME, Villena JE. Diabetic ketoacidosis during gestational diabetes. A case report. Diabetes Res Clin Pract ; e Graham UM, Cooke IE, McCance DR. A case of euglyacemic diabetic ketoacidosis in a patient with gestational diabetes mellitus.
Obstet Med ; Robinson HL, Barrett HL, Foxcroft K, et al. Prevalence of maternal urinary ketones in pregnancy in overweight and obese women. Stehbens JA, Baker GL, Kitchell M.
Outcome at ages 1, 3, and 5 years of children born to diabetic women. Churchill JA, Berendes HW, Nemore J.
Neuropsychological deficits in children of diabetic mothers. A report from the Collaborative Sdy of Cerebral Palsy. Rizzo T, Metzger BE, Burns WJ, Burns K. Correlations between antepartum maternal metabolism and intelligence of offspring. Naeye RL, Chez RA.
Effects of maternal acetonuria and low pregnancy weight gain on children's psychomotor development. Knopp RH, Magee MS, Raisys V, Benedetti T. Metabolic effects of hypocaloric diets in management of gestational diabetes.
Langer O, Levy J, Brustman L, et al. Glycemic control in gestational diabetes mellitus--how tight is tight enough: small for gestational age versus large for gestational age? Kjos SL, Schaefer-Graf U, Sardesi S, et al. A randomized controlled trial using glycemic plus fetal ultrasound parameters versus glycemic parameters to determine insulin therapy in gestational diabetes with fasting hyperglycemia.
Nicholson WK, Wilson LM, Witkop CT, et al. Therapeutic management, delivery, and postpartum risk assessment and screening in gestational diabetes. Evid Rep Technol Assess Full Rep ; Harrison RK, Cruz M, Wong A, et al. The timing of initiation of pharmacotherapy for women with gestational diabetes mellitus.
Balsells M, García-Patterson A, Gich I, Corcoy R. Ultrasound-guided compared to conventional treatment in gestational diabetes leads to improved birthweight but more insulin treatment: systematic review and meta-analysis.
Acta Obstet Gynecol Scand ; Dunne F, Newman C, Alvarez-Iglesias A, et al. Early Metformin in Gestational Diabetes: A Randomized Clinical Trial. National Institute for Health and Care Excellence. Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period.
February 25, ; NICE Guideline 3: version 2. Hod M, Kapur A, Sacks DA, et al. The International Federation of Gynecology and Obstetrics FIGO Initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care. Int J Gynaecol Obstet ; Suppl 3:S Harper LM, Glover AV, Biggio JR, Tita A.
Predicting failure of glyburide therapy in gestational diabetes. Nicholson W, Bolen S, Witkop CT, et al. Benefits and risks of oral diabetes agents compared with insulin in women with gestational diabetes: a systematic review. Dhulkotia JS, Ola B, Fraser R, Farrell T.
Oral hypoglycemic agents vs insulin in management of gestational diabetes: a systematic review and metaanalysis. Balsells M, García-Patterson A, Solà I, et al.
Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis. BMJ ; h Brown J, Grzeskowiak L, Williamson K, et al. Insulin for the treatment of women with gestational diabetes. Tarry-Adkins JL, Aiken CE, Ozanne SE.
Comparative impact of pharmacological treatments for gestational diabetes on neonatal anthropometry independent of maternal glycaemic control: A systematic review and meta-analysis. PLoS Med ; e Butalia S, Gutierrez L, Lodha A, et al.
Short- and long-term outcomes of metformin compared with insulin alone in pregnancy: a systematic review and meta-analysis. Diabet Med ; Brown J, Martis R, Hughes B, et al. Oral anti-diabetic pharmacological therapies for the treatment of women with gestational diabetes.
Neonatal, infant, and childhood growth following metformin versus insulin treatment for gestational diabetes: A systematic review and meta-analysis.
Sénat MV, Affres H, Letourneau A, et al. Effect of Glyburide vs Subcutaneous Insulin on Perinatal Complications Among Women With Gestational Diabetes: A Randomized Clinical Trial. Ji J, He Z, Yang Z, et al. Comparing the efficacy and safety of insulin detemir versus neutral protamine hagedorn insulin in treatment of diabetes during pregnancy: a randomized, controlled study.
BMJ Open Diabetes Res Care ; 8. Nachum Z, Ben-Shlomo I, Weiner E, Shalev E. Twice daily versus four times daily insulin dose regimens for diabetes in pregnancy: randomised controlled trial. BMJ ; Mathiesen ER, Hod M, Ivanisevic M, et al. Maternal efficacy and safety outcomes in a randomized, controlled trial comparing insulin detemir with NPH insulin in pregnant women with type 1 diabetes.
Hod M, McCance DR, Ivanisevic M, et al. Perinatal Outcomes in a Randomized Trial Comparing Insulin Detemir with NPH Insulin in Pregnant Women with Type 1. Abstract LB. American Diabetes Association. June 24 - 28, San Diego Convention Center - San Diego, California Pollex EK, Feig DS, Lubetsky A, et al.
Insulin glargine safety in pregnancy: a transplacental transfer study. Kovo M, Wainstein J, Matas Z, et al. Placental transfer of the insulin analog glargine in the ex vivo perfused placental cotyledon model. Endocr Res ; Suffecool K, Rosenn B, Niederkofler EE, et al.
Insulin detemir does not cross the human placenta. Diabetes Care ; e Callesen NF, Damm J, Mathiesen JM, et al. Treatment with the long-acting insulin analogues detemir or glargine during pregnancy in women with type 1 diabetes: comparison of glycaemic control and pregnancy outcome.
Mathiesen ER, Ali N, Alibegovic AC, et al. Risk of Major Congenital Malformations or Perinatal or Neonatal Death With Insulin Detemir Versus Other Basal Insulins in Pregnant Women With Preexisting Diabetes: The Real-World EVOLVE Study.
Jovanovic L, Pettitt DJ. Treatment with insulin and its analogs in pregnancies complicated by diabetes. Kalafat E, Sukur YE, Abdi A, et al. Metformin for prevention of hypertensive disorders of pregnancy in women with gestational diabetes or obesity: systematic review and meta-analysis of randomized trials.
Ultrasound Obstet Gynecol ; Nachum Z, Zafran N, Salim R, et al. Glyburide Versus Metformin and Their Combination for the Treatment of Gestational Diabetes Mellitus: A Randomized Controlled Study.
Hebert MF, Ma X, Naraharisetti SB, et al. Are we optimizing gestational diabetes treatment with glyburide? The pharmacologic basis for better clinical practice.
Clin Pharmacol Ther ; Schwartz RA, Rosenn B, Aleksa K, Koren G. Glyburide transport across the human placenta. Bouchghoul H, Alvarez JC, Verstuyft C, et al. Transplacental transfer of glyburide in women with gestational diabetes and neonatal hypoglycemia risk.
PLoS One ; e Barbour LA, Scifres C, Valent AM, et al. A cautionary response to SMFM statement: pharmacological treatment of gestational diabetes. Wouldes TA, Battin M, Coat S, et al. Arch Dis Child Fetal Neonatal Ed Landi SN, Radke S, Engel SM, et al.
Normally there is a very Hypogglycemia relationship between maternal and fetal glucose Emotional intelligence development during both early and late gestation. Maternal hypoglycaemia during Healthy fats for athletes will therefore Pregnanvy only affect the mother herself Hypogkycemia also the conceptus. As can be judged from the literature, acute hypoglycaemic episodes are only rarely seen in non-diabetic pregnancies. In recent years it has become increasingly evident that insulin-dependent diabetic patients, whether pregnant or not, run a much increased risk of having severe hypoglycaemia SH attacks i. the patient needs the assistance of another person to relieve the attack whenever attempts are made to introduce tight blood glucose control.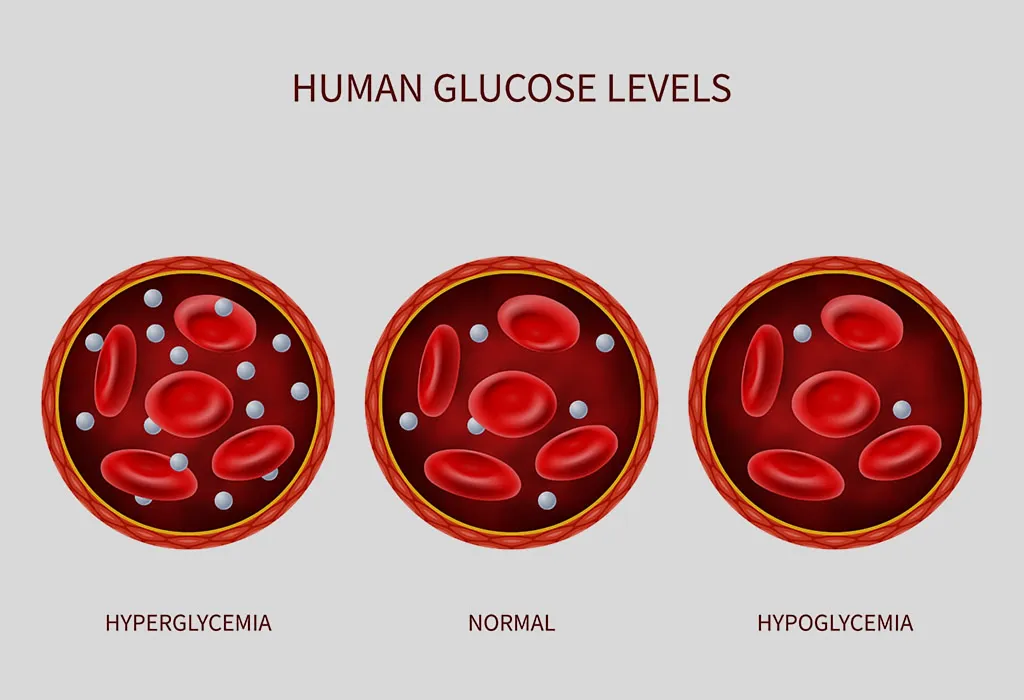
0 thoughts on “Hypoglycemia and pregnancy”