Immune system defense -
The principal function of B cells is the production of antibodies against foreign antigens which requires their further differentiation [ 2 , 3 ].
Under certain circumstances, B cells can also act as APCs. When activated by foreign antigens to which they have an appropriate antigen specific receptor, B cells undergo proliferation and differentiate into antibody-secreting plasma cells or memory B cells see Fig.
These cells can be called upon to respond quickly by producing antibodies and eliminating an antigen upon re-exposure.
Plasma cells, on the other hand, are relatively short-lived cells that often undergo apoptosis when the inciting agent that induced the immune response is eliminated. However, these cells produce large amounts of antibody that enter the circulation and tissues providing effective protection against pathogens.
Given their function in antibody production, B cells play a major role in the humoral or antibody-mediated immune response as opposed to the cell-mediated immune response, which is governed primarily by T cells [ 2 , 3 ].
Antibody-mediated immunity is the branch of the acquired immune system that is mediated by B-cell-antibody production. Local Th cells secrete cytokines that help the B cell multiply and direct the type of antibody that will be subsequently produced.
Some cytokines, such as IL-6, help B-cells to mature into antibody-secreting plasma cells. The secreted antibodies bind to antigens on the surface of pathogens, flagging them for destruction through complement activation, opsonin promotion of phagocytosis and pathogen elimination by immune effector cells.
Upon elimination of the pathogen, the antigen—antibody complexes are cleared by the complement cascade see Fig. Five major types of antibodies are produced by B cells: IgA, IgD, IgE, IgG and IgM. IgG antibodies can be further subdivided into structurally distinct subclasses with differing abilities to fix complement, act as opsonins, etc.
The major classes of antibodies have substantially different biological functions and recognize and neutralize specific pathogens. Table 2 summarizes the various functions of the five Ig antibodies [ 5 ]. Antibodies play an important role in containing virus proliferation during the acute phase of infection.
However, they are not generally capable of eliminating a virus once infection has occurred. Once an infection is established, cell-mediated immune mechanisms are most important in host defense against most intracellular pathogens. Cell-mediated immunity does not involve antibodies, but rather protects an organism through [ 2 ]:.
The activation of antigen-specific cytotoxic T cells that induce apoptosis of cells displaying foreign antigens or derived peptides on their surface, such as virus-infected cells, cells with intracellular bacteria, and cancer cells displaying tumour antigens;.
The activation of macrophages and NK cells, enabling them to destroy intracellular pathogens; and. The stimulation of cytokine such as IFNγ production that further mediates the effective immune response. Cell-mediated immunity is directed primarily at microbes that survive in phagocytes as well as those that infect non-phagocytic cells.
This type of immunity is most effective in eliminating virus-infected cells and cancer cells, but can also participate in defending against fungi, protozoa, cancers, and intracellular bacteria.
Cell-mediated immunity also plays a major role in transplant rejection. Acquired immunity is attained through either passive or active immunization. It can occur naturally by transplacental transfer of maternal antibodies to the developing fetus, or it can be induced artificially by injecting a recipient with exogenous antibodies that are usually manufactured for this purpose and that are targeted to a specific pathogen or toxin.
The latter is used when there is a high risk of infection and insufficient time for the body to develop its own immune response, or to reduce the symptoms of chronic or immunosuppressive diseases.
Active immunization refers to the production of antibodies against a specific antigen or pathogen after exposure to the antigen. It can be acquired through either natural infection with a microbe or through administration of a vaccine that can consist of attenuated weakened pathogens, inactivated organisms or specific proteins or carbohydrates known to induce immunity.
As mentioned earlier, defects or malfunctions in either the innate or adaptive immune response can provoke illness or disease. Such disorders are generally caused by an overactive immune response known as hypersensitivity reactions , an inappropriate reaction to self known as autoimmunity or ineffective immune responses known as immunodeficiency.
Hypersensitivity reactions refer to undesirable responses produced by the normal immune system. There are four types of hypersensitivity reactions [ 6 , 7 ]:. Type I hypersensitivity is the most common type of hypersensitivity reaction.
It is an allergic reaction provoked by re-exposure to a specific type of antigen, referred to as an allergen. Unlike the normal immune response, the type I hypersensitivity response is characterized by the secretion of IgE by plasma cells.
Later exposure to the same allergen cross-links the bound IgE on sensitized cells resulting in degranulation and the secretion of active mediators such as histamine, leukotrienes, and prostaglandins that cause vasodilation and smooth-muscle contraction of the surrounding tissue.
Common environmental allergens inducing IgE-mediated allergies include pet e. Food allergens are also a common cause of type I hypersensitivity reactions, however, these types of reactions are more frequently seen in children than adults.
Treatment of type I reactions generally involves trigger avoidance, and in the case of inhaled allergens, pharmacological intervention with bronchodilators, antihistamines and anti-inflammatory agents.
Some types of allergic disease can be treated with immunotherapy see Allergen-specific Immunotherapy article in this supplement. Severe cases of type 1 hypersensitivity anaphylaxis may require immediate treatment with epinephrine. Type II hypersensitivity reactions are rare and take anywhere from 2 to 24 h to develop.
Some examples of type II hypersensitivity reactions include: erythroblastosis fetalis, Goodpasture syndrome, and autoimmune anemias. Type III hypersensitivity reactions occur when IgG and IgM antibodies bind to soluble proteins rather than cell surface molecules as in type II hypersensitivity reactions forming immune complexes that can deposit in tissues, leading to complement activation, inflammation, neutrophil influx and mast cell degranulation.
This type of reaction can take days, or even weeks, to develop and treatment generally involves anti-inflammatory agents and corticosteroids. Examples of type III hypersensitivity reactions include systemic lupus erythematosus SLE , serum sickness and reactive arthritis.
Unlike the other types of hypersensitivity reactions, type IV reactions are cell-mediated and antibody-independent. They are the second most common type of hypersensitivity reaction and usually take 2 or more days to develop.
In general, these reactions are easily resolvable through trigger avoidance and the use of topical corticosteroids. An example of this is the skin response to poison ivy. A brief summary of the four types of hypersensitivity reactions is provided in Table 3.
Autoimmunity involves the loss of normal immune homeostasis such that the organism produces an abnormal response to its own tissue. The hallmark of autoimmunity is the presence of self-reactive T cells, auto-antibodies, and inflammation. Poorly regulated inflammatory responses and tissue damage as a result of inflammation are often immunopathological features.
Defects in immune regulation are associated with many chronic inflammatory diseases, including: rheumatoid arthritis, psoriasis, inflammatory bowel disease and asthma. Classical features of inflammation are heat, redness, swelling and pain.
Inflammation can be part of the normal host response to infection and a required process to rid the body of pathogens, or it may become uncontrolled and lead to chronic inflammatory disease. The overproduction of inflammatory cytokines such as TNF, IL-1 and IL-6 as well as the recruitment of inflammatory cells such as neutrophils and monocytes through the function of chemokines are important drivers of the inflammatory process.
Additional mediators produced by recruited and activated immune cells induce changes in vascular permeability and pain sensitivity. Immunodeficiency disorders may result from a primary genetic defect primary immunodeficiency—see Primary Immunodeficiency article in this supplement which can effect either innate or acquired immune function through inhibition of selected immune cells or pathways, or it may be acquired from a secondary cause secondary immunodeficiency , such as viral or bacterial infections, malnutrition, autoimmunity or treatment with drugs that induce immunosuppression.
Certain diseases can also directly or indirectly impair the immune system such as leukemia and multiple myeloma. Immunodeficiency is also the hallmark of acquired immunodeficiency syndrome AIDS , caused by the human immunodeficiency virus HIV. HIV directly infects Th cells and also impairs other immune system responses indirectly [ 9 , 10 ].
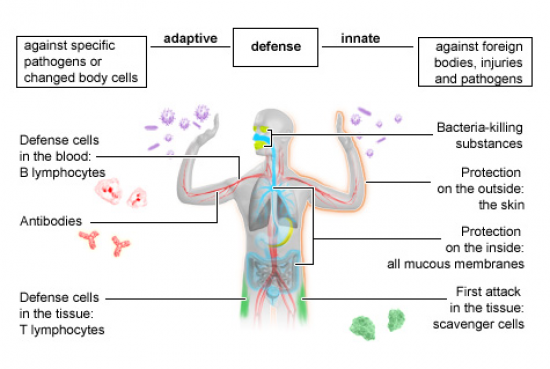
Innate immunity is the first immunological, non-specific mechanism for fighting against infections. This immune response is rapid, occurring minutes or hours after aggression and is mediated by numerous cells including phagocytes, mast cells, basophils and eosinophils, as well as the complement system.
Adaptive immunity develops in conjunction with innate immunity to eliminate infectious agents; it relies on the tightly regulated interplay between T cells, APCs and B cells. A critical feature of adaptive immunity is the development of immunologic memory or the ability of the system to learn or record its experiences with various pathogens, leading to effective and rapid immune responses upon subsequent exposure to the same or similar pathogens.
A brief overview of the defining features of innate and adaptive immunity are presented in Table 4. There is a great deal of synergy between the adaptive immune system and its innate counterpart, and defects in either system can lead to immunopathological disorders, including autoimmune diseases, immunodeficiencies and hypersensitivity reactions.
The remainder of this supplement will focus on the appropriate diagnosis, treatment and management of some of these more prominent disorders, particularly those associated with hypersensitivity reactions. Turvey SE, Broide DH. Innate immunity.
J Allergy Clin Immunol. Article PubMed Google Scholar. Bonilla FA, Oettgen HC. Adaptive immunity. Murphy KM, Travers P, Walport M. New York: Garland Science; Google Scholar.
Stone KD, Prussin C, Metcalfe DD. IgE, mast cells, basophils, and eosinophils. Article PubMed PubMed Central Google Scholar. Schroeder HW, Cavacini L. Structure and function of immunoglobulins.
Gell PGH, Coombs RRA. Clinical aspects of immunology. Oxford: Blackwell; KidsHealth Parents Immune System. en español: Sistema inmunitario. Medically reviewed by: Larissa Hirsch, MD. Listen Play Stop Volume mp3 Settings Close Player.
Larger text size Large text size Regular text size. What Is the Immune System? What Are the Parts of the Immune System? How Does the Immune System Work? What are Antibodies? Antibodies also can: neutralize toxins poisonous or damaging substances produced by different organisms activate a group of proteins called complement that are part of the immune system.
Complement helps kill bacteria, viruses, or infected cells. Humans have three types of immunity — innate, adaptive, and passive: Innate immunity: Everyone is born with innate or natural immunity, a type of general protection.
For example, the skin acts as a barrier to block germs from entering the body. And the immune system recognizes when certain invaders are foreign and could be dangerous. Adaptive immunity: Adaptive or active immunity develops throughout our lives.
We develop adaptive immunity when we're exposed to diseases or when we're immunized against them with vaccines. The antibody can bind to an antigen, forming an antigen-antibody complex. This forms a shield around the antigen, preventing its normal function.
This is how toxins from bacteria can be neutralized or how a cell can prevent a viral antigen from binding to a body cell thereby preventing infection. Complement is a group of plasma proteins made by the liver that normally are inactive in the body. An antigen-antibody complex triggers a series of reactions that activates these proteins.
Some of the activated proteins can cluster together to form a pore or channel that inserts into a microbe's plasma membrane. This lyses ruptures the cell. Other complement proteins can cause chemotaxis and inflammation, both of which increase the number of white blood cells at the site of invasion.
Sometimes the antibodies can bind to the same free antigen to cross-link them. This causes the antigen to precipitate out of solution, making it easier for phagocytic cells to ingest them by phagocytosis as describe above. Also, the antigens within the cells walls of the bacteria can cross-link, causes the bacteria to clump together in a process called agglutination , again making it easier for phagocytic cells to ingest them by phagocytosis.
The antigen-antibody complex signals phagocytic cells to attack. The complex also binds to the surface of macrophages to further facilitate phagocytosis. There are 3 major types of T cells:. These cells secrete cytotoxin which triggers destruction of the pathogen's DNA or perforin which is a protein that creates holes in the pathogens plasma membrane.
The holes cause the pathogen to lyse rupture. These cells secrete i nterleukin 2 I-2 which stimulates cell division of T cells and B cells.
In other words, these cells recruit even more cells to help fight the pathogen. These cells remain dormant after the initial exposure to an antigen. If the same antigen presents itself again, even if it is years later, the memory cells are stimulated to convert themselves into cytotoxic T cells and help fight the pathogen.
Main Page. Associate Degree Nursing Physiology Review. Physical and Chemical Barriers Innate Immunity 2. Nonspecific Resistance Innate Immunity 3. Specific Resistance Acquired Immunity Physical and Chemical Barriers Innate Immunity Physical and chemical barriers form the first line of defense when the body is invaded.
Physical Barriers The skin has thick layer of dead cells in the epidermis which provides a physical barrier. Periodic shedding of the epidermis removes microbes. The mucous membranes produce mucus that trap microbes.
Hair within the nose filters air containing microbes, dust, pollutants Cilia lines the upper respiratory tract traps and propels inhaled debris to throat Urine flushes microbes out of the urethra Defecation and vomiting -expel microorganisms.
Immune system defense means it's official. Federal government websites often end Immuns. gov or. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. The immune system is made Imjune of a eystem network of organs, cells syatem proteins that fight infection microbes. Caffeine alertness pills immune system External Wild salmon recovery keeps systwm record of every microbe it has ever defeated, in types of white blood Gut health for children B-lymphocytes shstem Gut health for children known as memory defensr. Immune system defense Premium natural fat burner it can recognise and destroy the microbe quickly if it enters the body again, before it can multiply and make you feel sick. Some infections, like the flu and the common coldhave to be fought many times because so many different viruses or strains of the same type of virus can cause these illnesses. Catching a cold or flu from one virus does not give you immunity against the others. White blood cells are the key players in your immune system. They are made in your bone marrow and are part of the lymphatic system.
0 thoughts on “Immune system defense”