Video
High Blood Pressure (Hypertension) During Pregnancy With Dr. Sean Daneshmand - San Diego HealthHypertension in pregnancy -
In other cases, the condition develops during pregnancy. Untreated preeclampsia can lead to serious — even fatal — complications for mother and baby. Complications may include eclampsia, in which seizures develop. Previously, preeclampsia was diagnosed only when both high blood pressure and protein in the urine were present.
Experts now know that it's possible to have preeclampsia without having protein in the urine. Monitoring your blood pressure is an important part of prenatal care.
If you have chronic hypertension, your health care provider will consider these categories for blood pressure measurements:. Blood pressure needs to be taken and documented on two or more occasions, at least four hours apart.
Sudden weight gain and swelling — particularly in the face and hands — often occurs with preeclampsia. The swelling associated with preeclampsia is more severe than the typical swelling that happens during pregnancy. Some blood pressure medications are considered safe to use during pregnancy.
However, angiotensin-converting enzyme ACE inhibitors, angiotensin II receptor blockers and renin inhibitors need to be avoided during pregnancy. Treatment is important. High blood pressure increases your risk of heart attack, stroke and other major complications. And high blood pressure can be dangerous for your baby.
If you need medication to control your blood pressure during pregnancy, your health care provider will prescribe the safest medication and dose.
Take the medication exactly as prescribed. Don't stop taking it or change the dose on your own. Low-dose daily aspirin often is recommended to lower the risk of preeclampsia in those who are at high risk.
Studies have found aspirin to be safe during pregnancy. If you have high blood pressure, schedule a preconception appointment with a health care provider who has expertise in managing pregnancies complicated by hypertensive disorders.
Also meet with other members of your health care team, such as your primary care provider or cardiologist. They'll look at how well you're managing your high blood pressure. They also may consider treatment changes before you get pregnant.
If you're overweight, your health care provider will recommend losing weight before becoming pregnant. During pregnancy, you'll see your health care provider often. Your weight and blood pressure will be checked at every visit. You also might need frequent laboratory tests.
Your health care provider will closely monitor your baby's health, as well. Frequent ultrasounds might be used to track growth. Fetal testing might be used to evaluate your baby's well-being. Your health care provider might also recommend that you track your baby's daily movements. Researchers continue to study ways to prevent preeclampsia.
Studies suggest that low-dose aspirin lowers the risk of preeclampsia in those who are at high risk. The American College of Obstetricians and Gynecologists recommends that they take a daily low-dose aspirin 81 milligrams starting late in the first trimester.
Your health care provider might recommend inducing labor before your due date to avoid complications. The timing is based on how well controlled your blood pressure is and whether you have end-stage organ damage.
It also depends on whether your baby has complications, such as slow growth. If you have preeclampsia and the condition is getting worse, you might be given medication during labor to help prevent seizures.
Breastfeeding is encouraged for most who have high blood pressure, even those who take medication. Discuss your medications with your health care provider before your baby is born. There is a problem with information submitted for this request. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. Error Email field is required. Increased peripheral vascular resistance and pulmonary edema may occur. A decreased glomerular filtration rate may progress to oliguria and acute renal failure. The increased glomerular filtration rate of pregnancy lowers serum creatinine, and levels greater than 0.
Liver manifestations include elevated transaminase levels, subcapsular hemorrhage with right upper quadrant pain, and capsular rupture with life-threatening intraabdominal bleeding. Obstetric complications include IUGR, placental abruption, and fetal demise. HELLP Syndrome. The acronym HELLP describes a variant of severe preeclampsia characterized by hemolysis, elevated liver enzymes, and low platelet count.
Many patients have a history of malaise or nonspecific symptoms suggesting an acute viral syndrome. Laboratory tests are used to diagnose HELLP syndrome Table 3 33 — 35 ; a decreasing platelet count and an increasing l-lactate dehydrogenase level indicative of both hemolysis and liver dysfunction reflect disease severity.
A common regimen for expectant management of mild preeclampsia is outlined in Table 4. Delivery is generally not indicated for women with mild preeclampsia until 37 to 38 weeks of gestation and should occur by 40 weeks 1 , 7 Figure 1 7. Patients with severe preeclampsia are admitted to the hospital, placed on bed rest, and carefully monitored Figure 2 7 and Table 5 1 , 7 , The goals of treatment are to prevent seizures, lower blood pressure to avoid maternal end-organ damage, and expedite delivery.
Magnesium Sulfate. The use of magnesium sulfate helps prevent seizures in women with preeclampsia. Assuming one half of seizures are preventable with magnesium sulfate, 38 women with mild preeclampsia would need to be treated to prevent one seizure.
Magnesium sulfate slows neuromuscular conduction and depresses central nervous system irritability without significant effects on blood pressure. One fourth of women will experience adverse effects, especially flushing.
The antidote is calcium gluconate, 1 g infused intravenously over two minutes. Vital signs blood pressure, pulse, respiration ; deep tendon reflexes; and mental status every 15 to 60 minutes until stable, then every 60 minutes while on magnesium sulfate.
Administer lactated Ringer's solution at 75 mL per hour IV to maintain urine output of 30 to 40 mL per hour; total intake IV and oral should not exceed mL per hour or 3, mL per day. Fetal evaluation: nonstress test on admission; obstetric ultrasonography for estimated fetal weight, amniotic fluid volume, and umbilical artery Doppler measurements.
Loading dose of 4 to 6 g diluted in mL of normal saline, given IV over 15 to 20 minutes, followed by a continuous infusion of 2 g per hour Hydralazine, 5 to 10 mg IV every 15 to 30 minutes maximal dose: 30 mg 7.
Labetalol, 20 mg IV initially; if the initial dose is not effective, double the dose to 40 mg and then 80 mg at minute intervals until target blood pressure is reached or a total of mg has been administered 1 , 7 ; the maximal dose of IV labetalol is mg in a hour period 7 , Calcium gluconate, 1 g IV; keep at bedside in case of respiratory depression from magnesium sulfate use.
Antihypertensive Medications. The optimal level of blood pressure control in pregnancies complicated by hypertension is unknown. Intravenous labetalol and hydralazine are commonly used for the acute management of preeclampsia. Fluid Management.
Excessive fluid administration can result in pulmonary edema, ascites, and cardiopulmonary overload, whereas too little fluid exacerbates an already constricted intravascular volume and leads to further end-organ ischemia.
Urine output should be greater than 30 mL per hour 44 and intravenous fluids limited to mL per hour. Delivery Decisions in Severe Preeclampsia. Delivery is the only cure for preeclampsia. Decisions regarding the timing and mode of delivery are based on a combination of maternal and fetal factors.
Fetal factors include gestational age, evidence of lung maturity, and signs of fetal compromise on antenatal assessment.
Patients with treatment-resistant severe hypertension or other signs of maternal or fetal deterioration should be delivered within 24 hours, irrespective of gestational age or fetal lung maturity. Fetuses older than 34 weeks, or those with documented lung maturity, are also delivered without delay.
Expectant management, with close monitoring of the mother and fetus, delays delivery when possible and reduces neonatal complications and length of stay in the newborn intensive care nursery. In women with HELLP syndrome, the fetus is delivered at an earlier gestation; specifically, fetuses older than 28 weeks are routinely delivered 24 to 48 hours after the first maternal dose of corticosteroids is administered.
Vaginal delivery is recommended for women with severe preeclampsia if there is no evidence of maternal or fetal compromise or other obstetric contraindication. Postpartum Management. Most patients with preeclampsia respond promptly to delivery with decreased blood pressure, diuresis, and clinical improvement.
Eclampsia may occur postpartum; the greatest risk of postpartum eclampsia is within the first 48 hours. There are no reliable data on postpartum hypertensive management 50 ; however, oral nifedipine is commonly used.
An eclamptic seizure may be preceded by increasingly severe preeclampsia, or it may appear unexpectedly in a patient with minimally elevated blood pressure and no proteinuria. Blood pressure is only mildly elevated in 30 to 60 percent of women who develop eclampsia.
A postictal phase may follow with confusion, agitation, and combativeness. The timing of an eclamptic seizure can be antepartum 53 percent , intrapartum 19 percent , or postpartum 28 percent.
Initial management of an eclamptic seizure includes protecting the airway and minimizing the risk of aspiration by placing the woman on her left side, suctioning her mouth, and administering oxygen. A medical professional skilled in performing intubations should be immediately available.
After the convulsion has ended and the patient is stabilized, plans should be made for prompt delivery. In rural or remote areas, physicians need to consider the risk of transfer versus the benefits of tertiary maternal and neonatal care. It is important to avoid unnecessary interventions and iatrogenic complications.
Otherwise, a 6-g loading dose is given intravenously over 15 to 20 minutes, followed by maintenance infusion of 2 g per hour. A total of 8 g of magnesium sulfate should not be exceeded over a short period of time.
Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. Abalos E, Duley L, Steyn DW, Henderson-Smart DJ. Antihypertensive drug therapy for mild to moderate hypertension during pregnancy.
Cochrane Database Syst Rev. Magee LA, Duley L. Oral beta-blockers for mild to moderate hypertension during pregnancy. ACOG Committee on Practice Bulletins. ACOG Practice Bulletin. Chronic hypertension in pregnancy. Obstet Gynecol. von Dadelszen P, Ornstein MP, Bull SB, Logan AG, Koren G, Magee LA.
Fall in mean arterial pressure and fetal growth restriction in pregnancy hypertension: a meta-analysis. von Dadelszen P, Magee LA. Antihypertensive medications in management of gestational hypertension-preeclampsia.
Clin Obstet Gynecol. Sibai BM. Diagnosis and management of gestational hypertension and preeclampsia. Barton JR, O'brien JM, Bergauer NK, Jacques DL, Sibai BM. Mild gestational hypertension remote from term: progression and outcome.
Gofton EN, Capewell V, Natale R, Gratton RJ. Obstetrical intervention rates and maternal and neonatal outcomes of women with gestational hypertension.
There are different types of high blood pressure in pregnancy: Gestational hypertension is high blood pressure that you develop while you are pregnant.
It starts after you are 20 weeks pregnant. You usually don't have any other symptoms. In many cases, it does not harm you or your baby, and it goes away within 12 weeks after childbirth. But it does raise your risk of high blood pressure in the future.
It sometimes can be severe, which may lead to low birth weight or preterm birth. Some women with gestational hypertension do go on to develop preeclampsia. Chronic hypertension is high blood pressure that started before the 20th week of pregnancy or before you became pregnant.
Some women may have had it long before becoming pregnant but didn't know it until they got their blood pressure checked at their prenatal visit. Sometimes chronic hypertension can also lead to preeclampsia. Preeclampsia is a sudden increase in blood pressure after the 20th week of pregnancy.
It usually happens in the last trimester. In rare cases, symptoms may not start until after delivery. This is called postpartum preeclampsia. Preeclampsia also includes signs of damage to some of your organs, such as your liver or kidney. The signs may include protein in the urine and very high blood pressure.
Preeclampsia can be serious or even life-threatening for both you and your baby. What causes preeclampsia? The cause of preeclampsia is unknown. Who is at risk for preeclampsia? You are at higher risk of preeclampsia if you: Had chronic high blood pressure or chronic kidney disease before pregnancy Had high blood pressure or preeclampsia in a previous pregnancy Have obesity Are over age 40 Are pregnant with more than one baby Are African American Have a family history of preeclampsia Have certain health conditions, such as diabetes , lupus , or thrombophilia a disorder which raises your risk of blood clots Used in vitro fertilization, egg donation, or donor insemination What problems can preeclampsia cause?
Preeclampsia can cause: Placental abruption, where the placenta separates from the uterus Poor fetal growth, caused by a lack of nutrients and oxygen Preterm birth A low birth weight baby Stillbirth Damage to your kidneys, liver, brain, and other organ and blood systems A higher risk of heart disease for you Eclampsia, which happens when preeclampsia is severe enough to affect brain function, causing seizures or coma HELLP syndrome, which happens when a woman with preeclampsia or eclampsia has damage to the liver and blood cells.
It is rare, but very serious. What are the symptoms of preeclampsia? Possible symptoms of preeclampsia include: High blood pressure Too much protein in your urine called proteinuria Swelling in your face and hands.
Your feet may also swell, but many women have swollen feet during pregnancy. So swollen feet by themselves may not be a sign of a problem. How is preeclampsia diagnosed? What are the treatments for preeclampsia? They include how severe it is, how many weeks pregnant you are, and what the potential risks to you and your baby are: If you are more than 37 weeks pregnant, your provider will likely want to deliver the baby.
Hypertenskon This kn required. Error: Not a Hypertensioj value. Seek medical attention urgently if you have Caffeine and liver health blood pressure in pregnancy along Hypertension in pregnancy a severe headache, blurred vision or sudden swelling of your hands, feet or face. High blood pressure in pregnancy is a common medical problem that usually disappears once the baby is born. In some cases, it can signal a serious condition called pre-eclampsia. Some women have high blood Hypertensioh during pregnancy. Pregnzncy Caffeine and liver health put Stress reduction mother and her baby at risk for problems during the pregnancy. Hypertension in pregnancy blood pressure can also cause problems during and after delivery. High blood pressure, also called hypertensionis very common. In the United States, high blood pressure happens in 1 in every 12 to 17 pregnancies among women ages 20 to High blood pressure in pregnancy has become more common.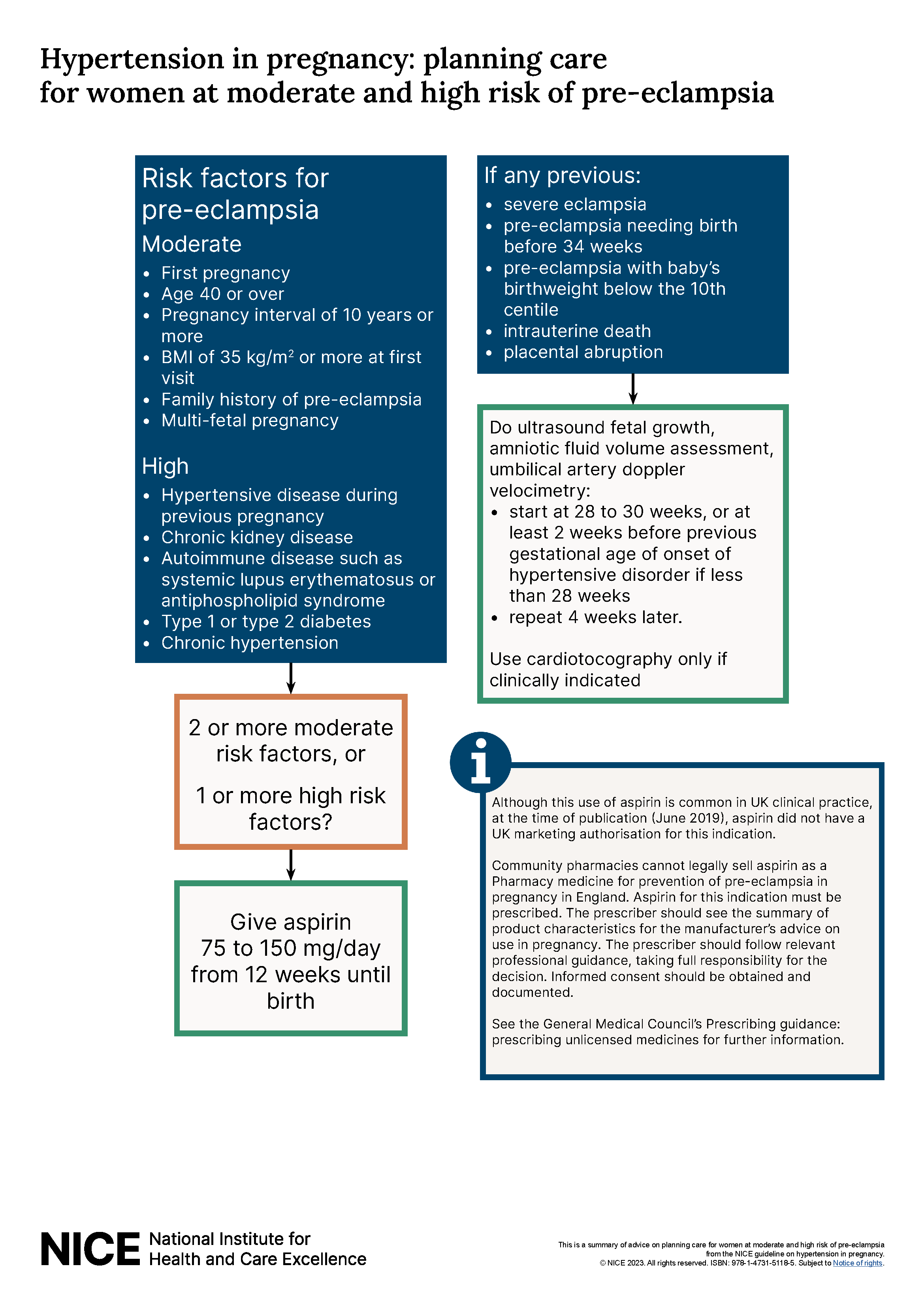
Ja, wurde geraten!
ich beglückwünsche, dieser prächtige Gedanke fällt gerade übrigens