Hypoglycemia and sleep disorders -
Furthermore, CPAP treatment significantly improved HBGI from 0. Average glucose levels measured using flash glucose monitoring device.
Average glucose levels recorded by flash glucose monitoring before CPAP treatment solid line and 1-week time point after CPAP treatment dotted line in patients with OSA. Our study demonstrated significantly greater GV, evidenced by nocturnal values of SD, CV, TIR, and HBGI, in patients with OSA and normal glucose tolerance, compared with healthy individuals.
The results also suggested possible increase in various markers of hypoglycemia in patients with REM-related OSA. In addition, various indexes of OSA severity, particularly percent time in hypoxemia, were associated with nocturnal GV.
Our results also showed that 1-week CPAP treatment significantly improved nocturnal GV in patients with OSA. We consider it particularly important to evaluate GV during sleep in patients with OSA.
Peng et al. They showed that the OSA group had significantly higher levels of postprandial blood glucose and within-day and nighttime mean amplitude of glycemic excursion MAGE than the control group and concluded that OSA severity AHI was positively correlated with these GV indicators [ 21 ].
Nakata et al. reported a positive correlation between log MAGE and AHI [ 22 ], and concluded that AHI negatively affects GV.
Kurosawa et al. found a significant and positive correlation between AHI and NREM-AHI with SD [ 23 ], another index of GV. Khaire et al. In the present study, the values of various markers of GV e.
We also examined the associations between various indices related to breathing disorders and markers of GV during sleep. The results showed worsened GV SD and hyperglycemic risk HGBI with increased severity of OSA, especially with the percent time in hypoxemia SLT90 , rather than with AHI.
What is the underlying mechanism s of GV during sleep in non-diabetic patients with OSA? While our study did not directly examine these mechanisms, previous studies hinted to the potential roles of hypoxemia.
In this regard, Hui et al. reported that the more pronounced the sleep-related hypoxemia is in patients with OSA and T2DM, the higher the likelihood of hyperglycemia [ 25 ].
Their results also suggested the presence of mechanisms that increase oxidative stress and catecholamine release. Sun et al. used experimental animals to show that acute hypoxia promoted glycogenolysis and glycolysis in the liver and consequently increased plasma glucose levels, suggesting that energy metabolism is defined by the degree and duration of hypoxemia [ 26 ].
It is possible that the observed GV in our patients with OSA and normal glucose tolerance is related to one or more of the above effects of acute hypoxemia on glucose metabolism. Further clinical and experimental studies are needed to determine the true mechanism of OSA-related changes in glucose metabolism.
Several studies have demonstrated the beneficial effects of CPAP therapy in patients with T2DM. Morariu et al. studied 23 patients with OSA and T2DM were divided into using active CPAP group and sham CPAP group for 30 days. Active CPAP therapy demonstrated improvements in glycemic control as determined using serum fructosamine but not coutinuous glucose monitoring [ 27 ].
Another study reported improvement in blood glucose fluctuations after CPAP therapy [ 28 , 29 ]. The above studies were conducted in patients with T2DM, and CPAP therapy was considered to have contributed to improvement in insulin resistance, which was considered the primary factor contributing to these improvements.
In contrast to the above studies, another study of 13 patients with OSA free of T2DM showed no significant improvement in HOMA-IR after 2. Unlike the preceding studies, the latter study focused on GV in patients with OSA and normal glucose tolerance. Similarly, our study was conducted in patients with normal glucose tolerance and we also showed marked improvement in GV after 1 week of CPAP therapy.
In this study, we further found that the risks of hypoglycemia, such as TBR and LBGI, were significantly higher in the REM-related OSA group than those in the non-specific OSA group. In contrast, the risk of hyperglycemia was positively correlated with NREM-AHI, arousal index, and percentage of stage N1.
What are the mechanisms of hyperglycemia or hypoglycemia risks increase even during sleep? Regarding the risks of hyperglycemia, hypoxemia and the resultant sleep fragmentation [ 1 ] are important factors.
The assumed mechanism is that both conditions can lead to extreme hypertonicity of the sympathetic nervous system, which stimulates the glycolytic system.
Regarding the risks of hypoglycemia in REM-related OSA, the mechanism is probably related to the enhanced dominance of the parasympathetic activities during NREM sleep by counter adjustment of the autonomic nervous system and the insufficient prevention of hypoglycemia due to the suppressed flash secretion of growth hormones [ 30 ].
Jones et al. reported possible nocturnal counter-regulatory hormone responses even in healthy individuals [ 31 ]. Furthermore, Bialasiewicz et al.
reported that the early morning fall in blood glucose levels is reversed by sleep breathing disorders during the REM sleep, presumably due to the involvement of altered neuroendocrine regulation [ 32 ].
Since the longest phase of REM sleep occurs in the latter part of the sleep cycle, patients with typical REM-related OSA experience relatively long and frequent apneas during the early morning hours compared to fewer apneas in the first few hours of sleep.
Based on the compensatory decrease in epinephrine secretion due to counter-regulatory hormone responses, parasympathetic nerves become relatively dominant in the first part of sleep, leading to a decrease in glucagon secretion or downregulation of other pathways, possibly resulting in falls in blood glucose levels.
Furthermore, in this study, many patients did not reach stage N3. Therefore, there was a possibility that the hypoglycemia prevention mechanism did not work due to the suppressed flash secretion of growth hormones [ 30 ].
There are some limitations to this study. First, the diet of each patient was not standardized because we enrolled outpatients. Second, the sample size in the present study was relatively small.
In particular, the number of control participants was small, and PSG testing was not performed. Our results should be verified in another study that includes a larger number of subjects. In conclusion, the results of the present study demonstrated greater GV during sleep in patients with OSA and normal glucose tolerance, compared with healthy individuals.
In addition, GV during sleep and the risk of hyperglycemia increased with the severity of OSA. Furthermore, several indexes of GV during sleep improved significantly after 7-day CPAP therapy.
On the other hand, our results demonstrated that patients with REM-related OSA are potentially at higher risk of developing hypoglycemia.
Arnardottir ES, Mackiewicz M, Gislason T, Teff KL, Pack AI Molecular signatures of obstructive sleep apnea in adults: a review and perspective. Sleep 32 4 — Article Google Scholar. Yoshihisa A, Owada T, Hoshino Y et al Flow-mediated dilatation identifies impaired endothelial function in patients with sleep apnea syndrome.
Fukushima J Med Sci 56 2 — Iguchi A, Yamakage H, Tochiya M, Muranaka K, Sasaki Y, Kono S, Shimatsu A, Satoh-Asahara N Effects of weight reduction therapy on obstructive sleep apnea syndrome and arterial stiffness in patients with obesity and metabolic syndrome.
J Atheroscler Thromb 20 11 — Hirakawa Y, Arima H, Zoungas S, Ninomiya T, Cooper M, Hamet P, Mancia G, Poulter N, Harrap S, Woodward M, Chalmers J Impact of visit-to-visit glycemic variability on the risks of macrovascular and microvascular events and all-cause mortality in type 2 diabetes: the ADVANCE trial.
Diabetes Care 37 8 — Article CAS Google Scholar. Su G, Mi SH, Tao H, Li Z, Yang HX, Zheng H, Zhou Y, Tian L Impact of admission glycemic variability, glucose, and glycosylated hemoglobin on major adverse cardiac events after acute myocardial infarction.
Diabetes Care 36 4 — Hanefeld M, Fischer S, Julius U, Schulze J, Schwanebeck U, Schmechel H, Ziegelasch HJ, Lindner J Risk factors for myocardial infarction and death in newly detected NIDDM: the Diabetes Intervention Study, year follow-up.
Diabetologia 39 12 — Cavalot F, Petrelli A, Traversa M, Bonomo K, Fiora E, Conti M, Anfossi G, Costa G, Trovati M Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: lessons from the San Luigi Gonzaga Diabetes Study.
J Clin Endocrinol Metab 91 3 — Ceriello A The post-prandial state and cardiovascular disease: relevance to diabetes mellitus. Diabetes Metab Res Rev 16 2 — Bonds DE, Miller ME, Bergenstal RM, Buse JB, Byington RP, Cutler JA, Dudl RJ, Ismail-Beigi F, Kimel AR, Hoogwerf B, Horowitz KR, Savage PJ, Seaquist ER, Simmons DL, Sivitz WI, Speril-Hillen JM, Sweeney ME The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study.
BMJ b Article PubMed PubMed Central Google Scholar. Khunti K, Davies M, Majeed A, Thorsted BL, Wolden ML, Paul SK Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: a cohort study. Diabetes Care 38 2 — Torimoto K, Okada Y, Tanaka Y Hypoglycemia abrogates the vascular endothelial protective effect of exenatide in type 2 diabetes mellitus.
Diabetes Ther 10 3 — Gami AS, Howard DE, Olson EJ, Somers VK Day-night pattern of sudden death in obstructive sleep apnea. N Engl J Med 12 — Chow E, Bernjak A, Williams S, Fawdry RA, Hibbert S, Freeman J, Sheridan PJ, Heller SR Risk of cardiac arrhythmias during hypoglycemia in patients with type 2 diabetes and cardiovascular risk.
Diabetes 63 5 — Diabetologia 52 1 — Özlek B, Özlek E, Doğan V, Başaran Ö, Çil C, Çelik O, Biteker M, Bilge AR Implications of continuous positive airway pressure on heart rate variability in patients with obstructive sleep apnea: does gender matter?
Turk Kardiyol Dern Ars 48 1 — PubMed Google Scholar. Bergenstal RM, Beck RW, Close KL, Grunberger G, Sacks DB, Kowalski A, Brown AS, Heinemann L, Aleppo G, Ryan DB, Riddlesworth TD, Cefalu WT Glucose management indicator GMI : a new term for estimating A1C from continuous glucose monitoring.
Diabetes Care 41 11 — Molnar GD, Taylor WF, Ho MM Day-to-day variation of continuously monitored glycaemia: a further measure of diabetic instability. Diabetologia 8 5 — Kovatchev BP, Cox DJ, Gonder-Frederick LA, Clarke W Symmetrization of the blood glucose measurement scale and its applications.
Diabetes Care 20 11 — Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, Troester MT, Vaughn BV AASM Scoring Manual Updates for Version 2. J Clin Sleep Med 13 5 — Hoshino T, Sasanabe R, Tanigawa T, Murotani K, Arimoto M, Ueda H, Shiomi T Effect of rapid eye movement-related obstructive sleep apnea on adherence to continuous positive airway pressure.
J Int Med Res 46 6 — You must accept the terms and conditions. Add comment Cancel. Submit a comment. Comment title. You have entered an invalid code. Submit Cancel. Thank you for submitting a comment on this article. Your comment will be reviewed and published at the journal's discretion.
Please check for further notifications by email. Views More metrics information. Total Views Email alerts Article activity alert. Advance article alerts. New issue alert.
Subject alert. Receive exclusive offers and updates from Oxford Academic. Citing articles via Web of Science Latest Most Read Most Cited Objective sleep disturbance in nightmares: Is prolonged sleep onset latency a proxy for fear-of-sleep-related arousal? Tracked and self-reported nighttime smartphone use, general health, and healthcare utilization: results from the SmartSleep Study.
Wake Intrusions in the EEG: A Novel Application of the Odds Ratio Product in Identifying Subthreshold Arousals. Medication-Induced Central Sleep Apnea: A Unifying Concept. More from Oxford Academic.
Clinical Medicine. Clinical Neuroscience. Medicine and Health. Science and Mathematics. Sleep Medicine. Looking for your next opportunity? Director, Ruth L. and David S. Gottesman Institute for Stem Cell Research and Regenerative Medicine.
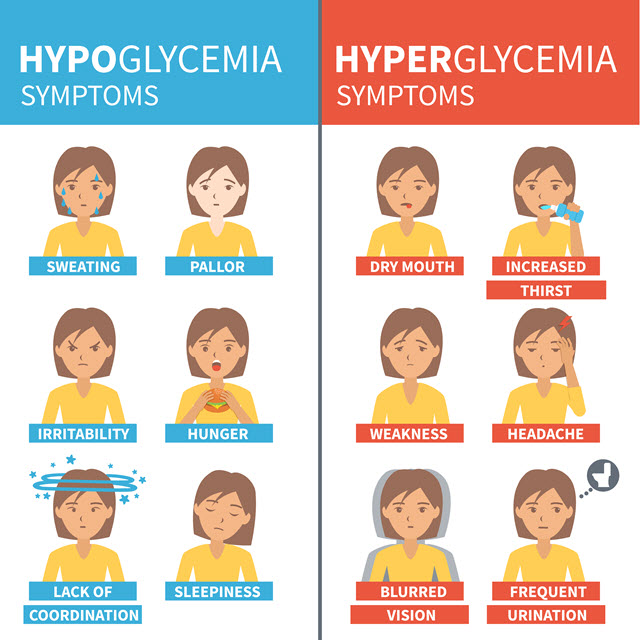
Assistant Professor. Symptoms may include: Inability to concentrate. Confusion and irritability. Slurred speech. Unsteadiness when standing or walking. Muscle twitching. Personality changes, such as anger or crying. Loss of consciousness coma. Signs of low blood sugar at night If your blood sugar drops while you are sleeping, your partner or other family members may notice that you are sweating and behaving differently.
Signs of low blood sugar at night nocturnal hypoglycemia include: Restless Legs Syndrome. Making unusual noises. Attempting to get out of bed or accidentally rolling out of bed. You may wake up with a headache in the morning if your blood sugar was low during the night.
Free Sleep Consultation. Refer a patient.
Stress affects Hypoglycemia and sleep disorders Hypoblycemia many ways and one of the most disprders results Boosts digestive health lack of sleep. This Sldep leads to difficulty focusing, fatigue, insomnia and ahd health problems. Lack of quality sleep can have profound effects on the way we perceive our world and navigate our day. A frequently examined cause of sleep problems is caffeine. One area of interest to scientists is carbohydrates and how they affect nocturnal hypoglycemia. Hypoglycemia tends to happen when blood glucose levels are abnormally low — too low for the body to function properly.
0 thoughts on “Hypoglycemia and sleep disorders”