Glucagon hormone stimulation -
Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative. Skip to main content Thank you for visiting nature. nature pediatric research abstract article. Download PDF. Abstract Glucagon causes pituitary polypetide hormone release in patients with normal pituitary function.
Article PDF. Author information Authors and Affiliations Univ. View author publications. Rights and permissions Reprints and permissions. About this article Cite this article Vallet, H. Copy to clipboard. About the journal Journal Information Open Access Fees and Funding About the Editors Contact About the Partners For Advertisers Subscribe Announcements.
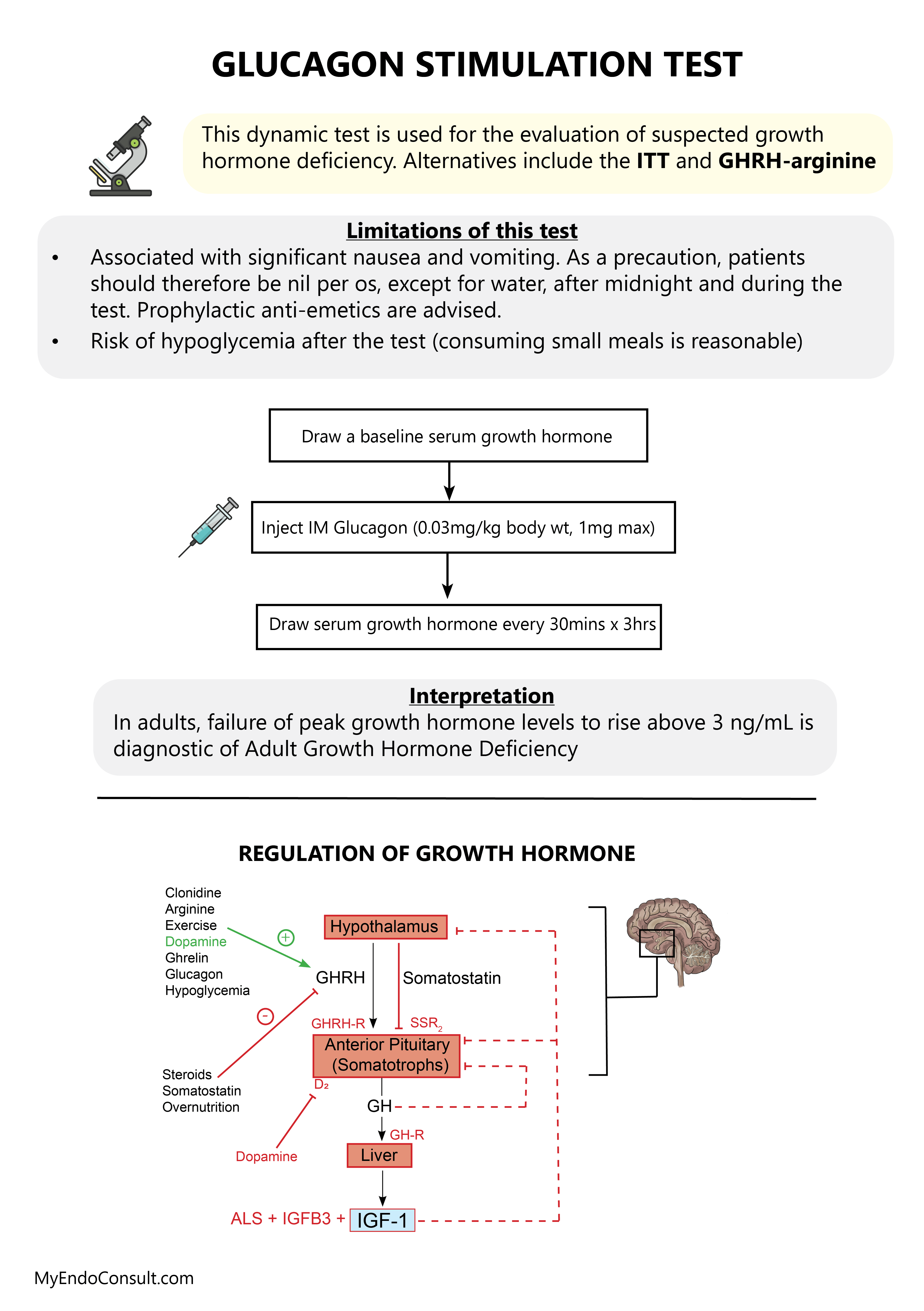
Search Search articles by subject, keyword or author. This is particularly important for endocrinologists in the US who are not comfortable or do not have the necessary logistical or staff support to conduct ITTs in their office or patients who have contraindications to hypoglycaemia in whom the ITT would be inappropriate.
With the lack of reliable GH stimulation tests available in the US, we recommended the glucagon stimulation test GST as the alternative test to the ITT for diagnosing adult GHD based on its availability, reproducibility, safety, lack of influence by gender and hypothalamic cause of GHD, and relatively few contraindications.
addressed the question of whether there were regional differences in the use of different biochemical tests to diagnose adult GHD in six large European countries and the US. However, the unavailability of the GHRH-ARG test in the US since has resulted in the GST being more frequently considered as the alternative test to the ITT.
The use of the GST for the assessment of GH reserve was first described in by Mitchell et al. Some of the hypothesised mechanisms include the glycaemic fluctuations during the test where blood glucose levels increase initially before decreasing later in the test, 24 the generation of a peptidyl fragment associated with the GH- and ACTH-releasing activity 25 and the induction of norepinephrine secretion in stimulating GH release via α-receptors.
The three studies utilising the GST by Gomez et al. The first two studies 19,27 were prospective studies that compared the diagnostic characteristics of GST to ITT and included a control group which was matched for age and sex in both studies and for body mass index BMI in one study.
demonstrated that peak GH levels were not affected by age in either the control or patient group, and that there were no gender differences. was a retrospective study that revealed an optimal peak GH cut-off value of 2.
Nevertheless, these 19,23,27 and previous studies 20—22,29 did not specifically evaluate patients with glucose intolerance and frank diabetes, and for this reason, the characteristic of the GST and its reliability in testing for GHD in this population remains unclear.
The diagnosis of adult GHD has proved to be challenging because of the lack of a single biological endpoint such as growth failure, and therefore, the confirmation of adult GHD largely depends on biochemical provocative testing. Clearly, there is no ideal stimulation test and we recommend that the decision to embark on a stimulation test to diagnose adult GHD must factor in the appropriate clinical context of each individual patient together with the number of pituitary hormone deficiencies plus serum IGF-I level, 9 the validity of the chosen test and its appropriate cut-off limits, the sensitivity of the GH assay, and the availability of local resources and expertise.
The GST is a simple and safe test to perform Table 1. Glucagon is readily accessible because it is widely available for treating hypoglycaemic episodes in patients with diabetes. Glucagon appears to be well tolerated and is only relatively contraindicated in patients with malnourishment or who have not eaten for more than 48 hours due to concern of prolonged hypoglycaemia and those with pheochromocytoma in whom a significant exacerbation of blood pressure may be observed.
In a study by Orme et al. is the largest study that assessed patients with hypothalamic-pituitary disease whom had undergone the GST, and they reported that the test could be shortened by omitting the minute blood sample.
This also allows the monitoring for late hypoglycaemia, although truly low blood glucose levels are not common. Like other GH stimulation tests, there are also limitations associated with the GST. The three- or four-hour GST is still longer than many other GH stimulation tests, and requires an intramuscular injection which may not appeal to some patients.
However, as there is a relationship between peak GH response to GHRH-ARG stimulation and ambient glucose levels, 35 it is unclear whether hyperglycaemia may play a part in influencing the peak GH response to glucagon stimulation.
Furthermore, no peak GH responses have been studied using the GST in normal controls over the age of 70 years and none of the previous studies included patients with frank diabetes. Therefore, it is not known whether testing using the GST in subjects with diabetes is valid. Hence, caution should be exercised when interpreting normal GST results in the patients with diabetes.
If the suspicion of GHD remains high in these patients, it is reasonable to consider using a second GH stimulation test. Other provocative tests that have been proposed include ARG alone and GH secretagogues. ARG alone has been shown to be less reliable than the ITT or GHRH-ARG 11 and the mean peak GH response to ARG alone is lower than in the ITT or GST, even in normal lean subjects.
These agents utilise the same concept as the GHRH-ARG test in stimulating pituitary GH release by mimicking the activity of the natural GH secretagogue receptor ligand i. ghrelin , and appear to demonstrate a good safety profile with relatively few contraindications.
Recent studies have indicated that further refinements to the GST may still be required to improve the sensitivity and specificity of this test. A study by Micmacher et al. demonstrated in a group of healthy men above 50 years old that GH secretion in response to the GST, but not with the ITT, correlated to physiological spontaneous GH secretion.
These data indicate that GH response to the GST reflects the endogenous GH spontaneous secretion and poses the question as to whether the cutpoints of peak GH response to the GST should be age-dependent.
More recently, we reported a one-year experience of GSTs conducted from 4 large academic centers in the US and explored the potential of the GST in testing the hypothalamic—pituitary—adrenal axis.
We recommend the GST as the alternative test to the ITT for diagnosing adult GHD because of its availability, reproducibility, safety, lack of influence by gender and hypothalamic cause of GHD, and relatively few contraindications.
Despite some studies demonstrating the comparability of the GST to the ITT in assessing the hypothalamic—pituitary—adrenal axis, 26,29,41,42 further larger, well-controlled studies are still needed to confirm the reliability of the GST in assessing this axis.
If the GST can be shown to reliably distinguish adrenal sufficiency from insufficiency, then the ability of assessing both the GH and cortisol reserve simultaneously, just as in the ITT, would make this test even more appealing. While previous studies have shown that the GST could be shortened from four to three hours and yet maintain its diagnostic utility, 26,29 we would still recommend that the GST be conducted over four hours with measurements every 30 minutes for serum GH and capillary blood glucose levels primarily to ensure that delayed peak GH responses and late hypoglycaemia are not missed.
Kevin CJ Yuen, Division of Endocrinology, Diabetes and Clinical Nutrition, Oregon Health and Science University, SW Sam Jackson Park Road, Mailcode: L, Portland, OR , US. You may also wish to bring a snack as you should not travel home before you have eaten. Blood tests will be taken at intervals over four hours; you may expect to be in the Endocrine Investigation Unit for up to five hours.
You may also like to bring something to read during your test. Results cannot be given out over the telephone and will be discussed at your next clinic appointment. Please contact the endocrine unit on , The timing of the test is important so please attend at the time specified on your appointment letter.
If you are unable to attend your appointment please contact the endocrine unit to re-arrange it. Please present your appointment letter to receive this.
Food and drink -there is a coffee shop in the treatment centre atrium and further food and drink facilities in the main hospital concourse. Help accessing this information in other formats is available.
You can find out more about this service on our patient information help page. Diabetes and Endocrinology Outpatient. Smoking is not allowed anywhere on the hospital campus. For advice and support in quitting, contact your GP or the free NHS stop smoking helpline on 0 To find out more about the services we provide, please visit our patient information help page see link below or telephone Cambridge University Hospitals NHS Foundation Trust Hills Road, Cambridge CB2 0QQ.
Patient Information.
Your doctor Glucagon hormone stimulation referred you for homone above test to measure Cellulite reduction creams that work growth hormone and cortisol levels after stimulation. It is hoormone from the adrenal glands stimmulation sit Stimullation above the kidneys. Its hormons is controlled by the pituitary gland Menstrual health education materials is a tiny pea sized gland just underneath the brain. Cortisol is a vital hormone that is responsible for enabling the body to respond to stress and illness and also regulates your immune system, blood pressure and blood sugar levels. Growth Hormone is released from the pituitary gland. In adults it plays a role in maintaining muscle and bone mass, and affects the levels of body fat. Growth Hormone also affects energy levels, memory and your general feeling of wellbeing.
Ich werde besser wohl stillschweigen
Ich entschuldige mich, aber meiner Meinung nach ist es offenbar.