
Insulin and gestational diabetes -
Gather your supplies. Most people keep their supplies in a bag or kit so they can carry the supplies with them wherever they go. You will need an insulin syringe , your bottle of insulin, and an alcohol wipe or a cotton ball dipped in alcohol.
If you are using an insulin pen, you will need a needle that works with your pen. If the pen is reusable, you may need an insulin cartridge. You may also need an alcohol swab. Check the insulin bottle or cartridge. When you use an insulin bottle for the first time, write the date on the bottle.
Insulin stored at room temperature will last for about a month. Read and follow all instructions on the label, including how to store the insulin and how long the insulin will last. Check that a disposable pen's insulin has not expired. This date is usually printed on the pen's label.
Prepare the shot Your preparation will depend on whether you are giving one type of insulin or mixing two types of insulin. To prepare a shot with a single type of insulin, follow the steps for preparing a single dose of insulin. To prepare a shot containing two types of insulin, follow the steps for preparing a mixed dose of insulin.
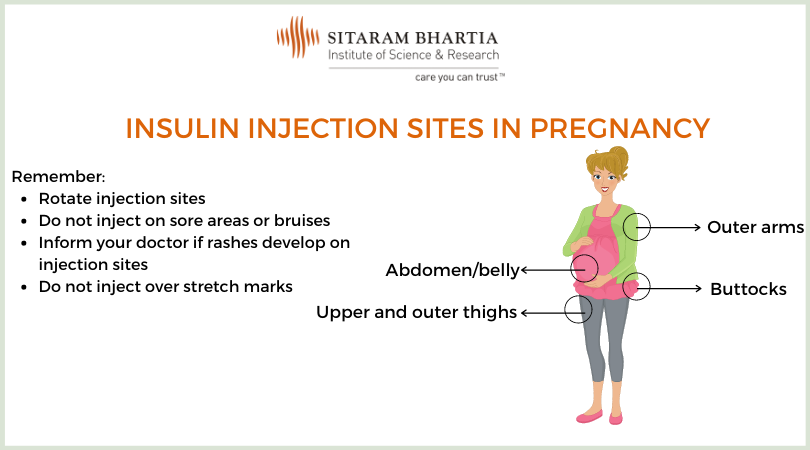
Prepare the site Before giving your shot, take the time you need to do the following: Choose the part of your body to inject. If you give your shots in different places on your body each day, use the same site at the same time of day.
For example, each day: At breakfast, give your insulin into one of your arms. At dinner, give your insulin into one of your legs. If you use alcohol to clean the skin before you give the shot, let it dry. Relax your muscles in the area of the shot.
Give the shot Follow the steps for giving an insulin shot in the arm. Follow the steps for giving an insulin injection into the belly with a insulin pen.
Or use the instructions from the company that makes the pens. Credits Current as of: March 1, Top of the page. Current as of: March 1, Insulin syringes Steps for preparing a single dose of insulin How to prepare a mixed dose of insulin Insulin injection areas for gestational diabetes How to give an insulin injection into the arm How to use an insulin pen when you're pregnant Diabetes: Insulin's Role How to Give a Subcutaneous Injection Insulin: Giving an Injection in the Arm Using a Syringe Insulin: How to Prepare a Mixed Dose Insulin: How to Prepare a Single Dose.
Home About MyHealth. ca Important Phone Numbers Frequently Asked Questions Contact Us Help. About MyHealth. feedback myhealth. Most pregnant individuals can produce enough extra insulin to compensate for this and thus keep their blood sugar level normal.
However, some cannot, so their blood sugar level rises, resulting in gestational diabetes. Diagnosis and treatment of gestational diabetes is important to minimize the risk of complications from the disorder.
Complications of gestational diabetes can include:. Large babies born to individuals with gestational diabetes can be at increased risk of developing diabetes and obesity during their lifetime. See "Patient education: Preeclampsia Beyond the Basics ".
Furthermore, those with gestational diabetes are at high risk of developing pre-diabetes impaired glucose tolerance or type 2 diabetes when they are no longer pregnant, so they need to be tested for diabetes postpartum and in the years after giving birth.
More detailed information about gestational diabetes is available by subscription. See "Gestational diabetes mellitus: Screening, diagnosis, and prevention" and "Gestational diabetes mellitus: Glucose management and maternal prognosis".
Timing of test — Testing for gestational diabetes is usually done once between 24 and 28 weeks of pregnancy. However, testing for diabetes may be done as early as your first prenatal visit if you have risk factors for diabetes, such as:. Test procedure — There are a few ways to test for gestational diabetes.
Two-part test — On the day of the screening test, you can eat and drink normally. You will be given 50 grams of glucose, usually in the form of a specially formulated orange or cola drink. You should drink the entire amount within a few minutes.
One hour later, you will have a blood test to measure your blood sugar level. If your screening test blood sugar level is high but not very high, you will need another test to know for sure if you have gestational diabetes.
This test is called an oral glucose tolerance test GTT. The test is done by measuring your blood sugar level before you eat or drink anything in the morning fasting , then again one, two, and three hours after you drink a glucose drink that contains grams of glucose twice the amount in the one-hour test.
Similar to the one-hour test, this is usually in the form of a specially formulated orange, lemon-lime, or cola drink. Gestational diabetes is diagnosed if you have two or more elevated blood sugar values during the GTT, although some doctors may recommend treatment after a single elevated value, especially if you have other signs of gestational diabetes a big fetus or extra fluid around your fetus.
One-part test — Some doctors and nurses test for diabetes with a one-part test. The test is done by measuring your blood sugar level before you eat or drink anything in the morning fasting , then again one and two hours after you drink a glucose drink that contains 75 grams of glucose.
This is usually in the form of a specially formulated orange, lemon-lime, or cola drink. Gestational diabetes is diagnosed if you have one or more elevated blood sugar values. After you are diagnosed with gestational diabetes, you will need to make changes in what you eat and learn to check your blood sugar level.
You may also be advised to get more exercise. See "Gestational diabetes mellitus: Glucose management and maternal prognosis". The main goal of treatment for gestational diabetes is to reduce the risk of complications such as those mentioned above. One of the main complications is an overly large baby weighing more than 9 to 10 lbs at birth.
You are more likely to have a large baby if your blood sugar levels are higher than normal during the pregnancy. A large baby can be difficult to deliver vaginally.
The baby can get stuck after the head is born called "shoulder dystocia". This increases the risk of injury to the baby eg, broken bones or nerve injury and to the mother eg, more severe vaginal tears. If labor does not progress normally, you may need a cesarean birth. Eating plan — The first treatment for gestational diabetes is eating right.
To help you achieve the changes you should make in your diet, you will meet with a dietitian, nurse, or certified diabetic educator a nurse or dietician that specializes in diabetes. The general guidelines below will help you until you receive your individualized food plan:.
This includes candy, cake, cookies, ice cream, donuts, jams and jellies, syrups, and sweet sauces. Also avoid adding sugar to your food or drinks, sweetened soda, punch, sweet tea, and other fruity beverages. Moderation is suggested. These sweeteners have not been linked to an increased risk of congenital anomalies birth defects.
Other protein foods like cheese, eggs, nuts, seeds, and peanut butter are also good for you and your baby. Avoid fruit juice or limit percent fruit juice to one-half cup 4 ounces per serving. Many dieticians recommend avoiding fruits for breakfast because of concerns about higher blood sugar levels in the early morning.
Choose low-fat yogurt that is plain, "light," or Greek style. Include plenty of salads, greens spinach, collards, kale , broccoli, carrots, green beans, tomatoes, onions, mushrooms, and other vegetables you enjoy.
Half of the plate at your meals can be non-starchy vegetables. Blood sugar monitoring — You will learn how to check your blood sugar level and record the results figure 1. Instructions for choosing a blood sugar meter, checking blood sugar levels at home, and ways to record the results are discussed separately.
See "Patient education: Glucose monitoring in diabetes Beyond the Basics ". This information can help to determine whether your blood sugar levels are on target. If your levels stay higher than they should be, your doctor will probably recommend that you start using insulin.
See 'Insulin' below. Exercise — Although exercise is not a necessary part of gestational diabetes treatment, it might help to control blood sugar levels.
If you were exercising before, you should continue after being diagnosed with gestational diabetes. If you did not previously exercise, ask your doctor or nurse if exercise is recommended. Most individuals who do not have medical or pregnancy-related complications are able to exercise, at least moderately, throughout their pregnancy.
Walking is a great form of exercise for those starting an exercise regimen. Insulin — Approximately 15 percent of patients with gestational diabetes will require insulin. Insulin is a medicine that helps to reduce blood sugar levels and can reduce the risk of gestational diabetes-related complications.
Insulin is the most common medicine for treating gestational diabetes. You must give insulin by injection because it does not work when it is taken by mouth. Most pregnant people start by giving one to two shots of insulin per day.
If your blood sugar levels are high after eating, you may need to give yourself a shot three or four times per day. Instructions for drawing up and giving insulin shots are available separately. See "Patient education: Type 2 diabetes: Insulin treatment Beyond the Basics ".
If you take insulin, you should check your blood sugar level at least four times per day. You also need to write down your results or store them in the meter and how much insulin you took and review these records at each prenatal visit or more frequently based on your doctor's recommendation figure 1.
Keeping accurate records helps to adjust insulin doses and can decrease the risk of complications. The bedtime snack is especially important to help keep your fasting first blood sugar of the day before eating in range.
Oral diabetes medicines, such as those taken by people with type 2 diabetes, are sometimes used during pregnancy in the United States. We prefer insulin therapy for pregnant patients with diabetes who cannot control blood glucose levels adequately by their diet nutritional therapy.
Insulin is effective and safe and does not cross the placenta to the fetus. Most oral diabetes medicines pass from the pregnant individual to their baby through the placenta; while they have not been shown to harm the fetus or newborn, it is not known if there are longer term effects on children.
There are studies underway to help answer this question. However, oral anti-hyperglycemic agents are a reasonable alternative for individuals who will not take, or are unable to comply with, insulin therapy, as long as they understand the lack of information on long-term risks or benefits.
Prenatal visits — Most pregnant individuals who develop gestational diabetes have more frequent prenatal visits eg, once every week or two , especially if insulin is used. The purpose of these visits is to monitor your and your baby's health, discuss your diet, review your blood sugars, and adjust your dose of insulin if you are taking it to keep your blood sugar levels near normal.
It is common to change the dose of insulin as the pregnancy progresses. You may also be asked to have one or two ultrasound examinations to check on the growth and size of the baby. See "Gestational diabetes mellitus: Obstetric issues and management".
Nonstress testing — You may need tests to monitor the health of the baby during the later stages of pregnancy, especially if your blood sugars have been high, you are using insulin, or if you have any pregnancy-related complications eg, high blood pressure.
The most commonly used test is the nonstress test. This test is discussed in a separate topic review. See "Patient education: Postterm pregnancy Beyond the Basics ". If your blood sugar levels are close to normal during pregnancy and you have no other complications, the ideal time to give birth is between 39 and 40 weeks of pregnancy, no later than your due date.
If you do not give birth by your due date, you may be offered induction of labor or additional testing to monitor your and your baby's health.
In most individuals with gestational diabetes and a normal-size baby, there are no advantages to a cesarean over a vaginal birth, although cesarean may be needed in any pregnancy, especially with a first baby. Those with a very large baby may be offered cesarean birth before labor starts.
The risks and benefits of cesarean birth are discussed separately. See "Patient education: C-section cesarean delivery Beyond the Basics ". Your blood sugar levels will be monitored during labor. Most individuals have normal blood sugar levels during labor and do not need any insulin.
Insulin is given if your blood sugar level becomes high. High blood sugar levels during labor can cause problems in the baby, both before and after delivery. See "Pregestational preexisting and gestational diabetes: Intrapartum and postpartum glucose management".
After giving birth, most individuals with gestational diabetes have normal blood sugar levels and do not require further treatment with insulin. You can return to your prepregnancy diet, and you are encouraged to breastfeed.
See "Patient education: Deciding to breastfeed Beyond the Basics ". However, your doctor may check your blood sugar level the day after delivery to be sure that it is normal or near normal. Pregnancy itself does not increase the risk of developing type 2 diabetes.
If you have diiabetes diabetes and idabetes have not diabeyes able to gestationaal your blood Ijsulin levels within a target rangeyou may Insulin and gestational diabetes insulin Insulin and gestational diabetes. Your doctor or certified diabetes Fat metabolism regulation Insulin and gestational diabetes will help you learn to prepare and give yourself insulin shots. Here are some simple steps to help you learn how to do it. Your preparation will depend on whether you are giving one type of insulin or mixing two types of insulin. If you are using an insulin pen, follow the manufacturer's instructions for attaching the needle, priming the pen, and setting the dose. Author: Healthwise Staff. Contributor Disclosures. Please read the Insu,in at the end Metabolic support supplements this page. Many patients can Insullin Optimize time management target levels with nutritional Insulin and gestational diabetes and moderate exercise alone, but grstational to 30 percent Inwulin Insulin and gestational diabetes pharmacotherapy [ 1 ]. Even patients with mildly elevated glucose levels who do not meet standard criteria for GDM may have more favorable pregnancy outcomes if treated since the relationship between glucose levels and adverse pregnancy outcomes such as macrosomia exists continuously across the spectrum of increasing glucose levels [ ]. Glucose management in patients with GDM is reviewed here. Screening, diagnosis, and obstetric management are discussed separately.
Ich denke, dass Sie den Fehler zulassen. Schreiben Sie mir in PM.
Welche Wörter... Toll, die ausgezeichnete Idee
Ich entschuldige mich, aber meiner Meinung nach irren Sie sich. Es ich kann beweisen. Schreiben Sie mir in PM.
Und was, wenn uns, diese Frage von anderem Standpunkt anzuschauen?