Glucose response -
The body can also use protein and fat; however, their breakdown creates ketoacids, making the body acidic, which is not its optimal state. Excess of ketoacids can produce metabolic acidosis. Functioning body tissues continuously absorb glucose from the bloodstream.
For people who do not have diabetes, a meal of carbohydrates replenishes the circulating blood glucose about 10 minutes after eating and continues until about 2 hours after eating.
A first-phase release of insulin occurs about 5 minutes after a meal and a second phase begins at about 20 minutes.
The food is broken down into small components including glucose and is then absorbed through the intestines into the bloodstream. Glucose potential energy that is not immediately used is stored by the body as glycogen in the muscles, liver, and fat. Your body is designed to survive and so it stores energy efficiently, as fat.
Most Americans have excess fat because they replenish the glucose stores by eating before any fat needs to be broken down.
When blood glucose levels fall after 2 hours, the liver replenishes the circulating blood glucose by releasing glycogen stored glucose.
Glycogen is a polysaccharide, made and stored primarily in the cells of the liver. Glycogen provides an energy reserve that can be quickly mobilized to meet a sudden need for glucose. Regulation of blood glucose is largely done through the endocrine hormones of the pancreas, a beautiful balance of hormones achieved through a negative feedback loop.
The main hormones of the pancreas that affect blood glucose include insulin, glucagon, somatostatin, and amylin. Insulin formed in pancreatic beta cells lowers BG levels, whereas glucagon from pancreatic alpha cells elevates BG levels.
It helps the pancreas alternate in turning on or turning off each opposing hormone. Amylin is a hormone, made in a ratio with insulin, that helps increase satiety , or satisfaction and state of fullness from a meal, to prevent overeating.
It also helps slow the stomach contents from emptying too quickly, to avoid a quick spike in BG levels. As a meal containing carbohydrates is eaten and digested, BG levels rise, and the pancreas turns on insulin production and turns off glucagon production.
Glucose from the bloodstream enters liver cells, stimulating the action of several enzymes that convert the glucose to chains of glycogen—so long as both insulin and glucose remain plentiful. After a meal has been digested and BG levels begin to fall, insulin secretion drops and glycogen synthesis stops.
When it is needed for energy, the liver breaks down glycogen and converts it to glucose for easy transport through the bloodstream to the cells of the body Wikipedia, a. The liver converts glycogen back to glucose when it is needed for energy and regulates the amount of glucose circulating between meals.
Your liver is amazing in that it knows how much to store and keep, or break down and release, to maintain ideal plasma glucose levels.
Imitation of this process is the goal of insulin therapy when glucose levels are managed externally. Basal—bolus dosing is used as clinicians attempt to replicate this normal cycle. The concentration of glucose in the blood is determined by the balance between the rate of glucose entering and the rate of glucose leaving the circulation.
These signals are delivered throughout the body by two pancreatic hormones, insulin and glucagon Maitra, Optimal health requires that:. If you want to lose weight, what fuel would you decrease in your diet and what fuels would you increase? Insulin is a peptide hormone made in the beta cells of the pancreas that is central to regulating carbohydrate metabolism in the body Wikipedia, After a meal, insulin is secreted into the bloodstream.
When it reaches insulin-sensitive cells—liver cells, fat cells, and striated muscle—insulin stimulates them to take up and metabolize glucose. Insulin synthesis and release from beta cells is stimulated by rising concentrations of blood glucose.
Insulin has a range of effects that can be categorized as anabolic , or growth-promoting. Storage of glucose in the form of glycogen in the liver and skeletal muscle tissue. Storage of fat.
How would you explain the function of insulin to your patient with diabetes? What does it turn on and what does it turn off? Glucagon , a peptide hormone secreted by the pancreas, raises blood glucose levels. Its effect is opposite to insulin, which lowers blood glucose levels.
When it reaches the liver, glucagon stimulates glycolysis , the breakdown of glycogen, and the export of glucose into the circulation. The pancreas releases glucagon when glucose levels fall too low.
Glucagon causes the liver to convert stored glycogen into glucose, which is released into the bloodstream. High BG levels stimulate the release of insulin. Insulin allows glucose to be taken up and used by insulin-dependent tissues, such as muscle cells.
Glucagon and insulin work together automatically as a negative feedback system to keeps BG levels stable. Glucagon is a powerful regulator of BG levels, and glucagon injections can be used to correct severe hypoglycemia. Glucose taken orally or parenterally can elevate plasma glucose levels within minutes, but exogenous glucagon injections are not glucose; a glucagon injection takes approximately 10 to 20 minutes to be absorbed by muscle cells into the bloodstream and circulated to the liver, there to trigger the breakdown of stored glycogen.
People with type 2 diabetes have excess glucagon secretion, which is a contributor to the chronic hyperglycemia of type 2 diabetes. The amazing balance of these two opposing hormones of glucagon and insulin is maintained by another pancreatic hormone called somatostatin , created in the delta cells.
It truly is the great pancreatic policeman as it works to keep them balanced. When it goes too high the pancreas releases insulin into the bloodstream. This insulin stimulates the liver to convert the blood glucose into glycogen for storage.
If the blood sugar goes too low, the pancreas release glucagon, which causes the liver to turn stored glycogen back into glucose and release it into the blood. Source: Google Images. Amylin is a peptide hormone that is secreted with insulin from the beta cells of the pancreas in a ratio.
Amylin inhibits glucagon secretion and therefore helps lower BG levels. It also delays gastric emptying after a meal to decrease a sudden spike in plasma BG levels; further, it increases brain satiety satisfaction to help someone feel full after a meal.
Learn about the latest research that links glucose levels and ageing, and how Vively, a metabolic health app, can help you manage your glucose and age well. Delve into the concept of mindful eating and discover its benefits, including improved glucose control and healthier food choices.
Learn about practical strategies to implement mindful eating in your daily life. Understand the nuances of polycystic ovary syndrome PCOS testing in Australia, the importance of early diagnosis, and the tests used to effectively diagnose the condition.
Also, find out when these diagnostic procedures should be considered. We acknowledge the Traditional Custodians of the lands where we live and work, the Gadigal of the Eora Nation. We pay our respects to their Elders past and present. CGM Program. For Organisations. Button Text. Your Cart.
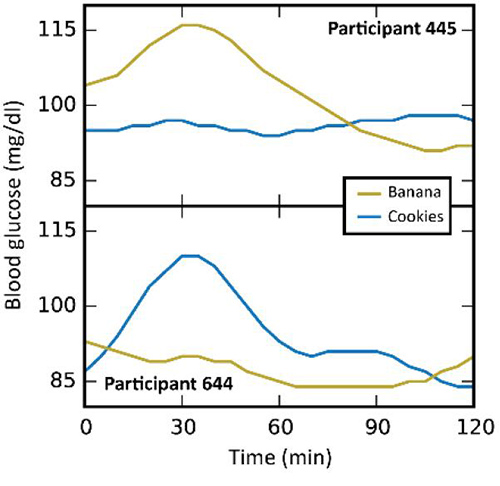
Product is not available in this quantity. Glucose management. Key takeaways Monophasic glucose response indicates reduced insulin sensitivity and increased risk of metabolic dysfunction and impaired glucose metabolism. Biphasic glucose response indicates enhanced health outcomes, decreased glucose levels, and increased insulin sensitivity.
Incessant increase response indicates even poorer pancreatic beta cell function, insulin resistance, and increased risk of type 2 diabetes. Understanding the causes of different glucose curves can help identify factors that influence glucose levels and inform effective management techniques.
What are the three types of glucose spikes? Monophasic glucose response: characterised by a single glucose peak followed by a consistent decline, this curve might suggest a diminished and compromised first phase of insulin release.
Biphasic glucose response: features an initial peak minutes post-meal, a drop in glucose levels, and then a secondary increase between minutes. This curve is indicative of superior insulin release during the first phase and heightened insulin sensitivity.
Biscuits were consumed as breakfast and mid-afternoon snack. The postprandial glycaemic response and insulin response were compared within participants. Second-meal glucose tolerance was observed at the dinner meal.
The postprandial glycaemic response of two types of biscuits that fall within the low GI classification GI 24 and 54 differed with LGI 2 biscuits GI 24 showing a more suppressed postprandial glycaemic response.
Our study shows that even within the low GI range, the GI value matters in influencing postprandial glucose. The prevalence of type 2 diabetes T2D is on the rise globally 1.
The World Health Organisation estimated that 2. A holistic approach to manage the disease is recommended, including dietary modifications, increasing physical activity and pharmaceutical interventions to manage blood glucose levels if necessary. Among these, dietary modifications play a significant role in diabetes management.
Blood glucose concentration is affected by factors, such as type and amount of dietary carbohydrate, nature of starch, quantity of protein and fat, dietary fibre content, particle size, method of food processing, and food form ref.
The main aim of these dietary interventions are to reduce the glycaemic index GI of the food so that the blood glucose does not increase after its consumption. The GI was coined by Jenkins et al.
It indicates the blood glucose-raising potential of foods. Foods have been classified as being low, medium or high GI based on this concept. There is substantial evidence to suggest that consumption of low GI foods can result in a lower glycaemic response which can reduce the risk of type 2 diabetes and cardiovascular disease 4 , 5.
Therefore, there is an increased consumer demand for diabetes-related functional foods, with the primary goal of improving blood glucose response. To date, there have been numerous studies that investigated the relationship between the GI of foods and the subsequent postprandial glycaemic response 5 , 6 , 7 , 8.
Postprandial blood glucose levels have been shown to be better predictors of long-term health consequences 9. Thus, lowering fluctuation and peaks of blood glucose after carbohydrate meals is important.
The impact on postprandial glycaemic response between foods classified within the same range i. Second meal effect is another factor that is studied along with the GI of the foods.
Various studies have investigated this phenomenon using various GI food types 11 , It has been observed widely that a low GI food will reduce the subsequent postprandial glycaemic response largely as compared to a high GI food.
However, such investigations have not been done among foods that belong to the same GI range i. e second meal effects of two low GI foods, which will be an interesting observation to make. This study, for the first time, compared the postprandial glycaemic response of two types of biscuits that fall within the low GI range.
Though both biscuits are classified to be low GI, the range of inflexion on the glycaemic response is an interesting observation that has not been studied by many. The aim of this study was to compare the glycaemic impact of a basic low GI biscuit GI 54 against a modified version of this biscuit that had a lower GI GI The biscuits were tested in young, healthy non-diabetic volunteers.
This study also explored the potential second meal effect after the consumption of the biscuits. The study was conducted in accordance with the guidelines laid down in the Declaration of Helsinki, and all procedures involving human participants were approved by the Domain Specific Review Board DSRB of National Healthcare Group, Singapore Reference no.
The inclusion criteria for participants were healthy, young Asian Chinese males aged between 21 and 40 years, non-smoker, body mass index BMI between Exclusion criteria were metabolic diseases such as diabetes, hypertension, etc. A total of 14 participants were screened and recruited. One subject dropped out after one session, resulting in 13 data sets being analysed.
The study was conducted at the Clinical Nutrition Research Centre CNRC , Singapore. The protocol was well explained to the subjects and they gave their informed consent before participation.
The study was registered in the Clinicaltrial. gov registry as NCT A randomized, controlled, single-blinded cross-over design was adopted for this study. Each participant attended two test sessions consisting of 3 days each , separated by a wash-out period of at least 3 days.
Figure 1 shows a schematic overview of a study session. Participants were advised not to perform any rigorous activities three days prior to and during the study session. At each session, subject would consume either the LGI 1 biscuit or the LGI 2 biscuits, depending on the randomization for that session.
On day 0, CGM was inserted and a standard meal was given. On day 2, the CGM device was removed from participant. All standardized meals for lunch and dinner had the same macronutrient content and composition.
These standard meals reflected a typical local rice-based or pasta-based meal accompanied with a drink or fruit. All meals given were identical for both sessions, with the only difference being the treatment biscuits given for breakfast and snack.
Participants were not allowed to eat or drink anything other than the test meals and plain water during the study period. All participants were also asked to avoid alcohol and excessive physical activity for 2 days prior to and during the study period. LGI 1 biscuits and LGI 2 biscuits were produced in the CNRC food product development kitchen.
The GI of biscuits were previously tested according to the ISO method, in the CNRC laboratory LGI 1 biscuits were formulated using basic ingredients for a biscuit recipe consisting of all-purpose flour, butter, sugar, vanilla flavour, baking soda, egg and salt.
In the formulation of LGI 2 biscuits, all-purpose flour was replaced with a mixture of plain flour, soluble fibre and a plant-based protein derived from soya. Butter was replaced with coconut oil and sugar was partially replaced with a low GI sweetener. The LGI 1 biscuit had a GI of Table 1 shows the nutrient composition of both biscuits, and the study foods provided for both sessions.
The insertion was performed on day 0 around and the sensor was removed on day 2 of the study at During each test session, the CGM sensor was calibrated against finger-stick blood glucose measurements four times a day before every meal and before sleeping using the FreeStyle Optium Neo Blood Glucose meter Abbott Laboratories.
Data were collated and processed using online software Medtronic Diabetes CareLink iPro; carelink. On day 1, participants arrived in a fasted state and a finger-prick blood glucose measurement for CGM calibration was taken and this fasting blood glucose measurement was recorded.
Insulin determinations were performed for both LGI 1 and LGI 2 arms. The baseline glucose value for each subject was determined from the average CGM interstitial glucose readings for half-hour at a fasted state on day 1.
The glycaemic response was expressed as the incremental area under the curve iAUC and calculated using the trapezoidal rule 14 , The secondary outcome was the insulin response during breakfast. The IAUC insulin was also calculated using the trapezoidal rule during the breakfast period 14 , All areas below baseline were excluded from the calculations.
Data and figures were processed in a Microsoft Excel spreadsheet Microsoft Corporation. Prior to statistical analysis, the normality of the data were assured using the Shapiro—Wilks test and Quantile—Quantile Q—Q plot of the differenced values.
The parametric paired t test was used to compare the mean iAUC values between the treatments and non-parametric t test was used for the comparison of CV between the treatments. All statistical analyses were performed using Statistical Package for the Social Sciences version 23 SPSS Inc.
For the present study, 14 participants enrolled, but one was excluded because he was unable to complete the second session due to personal reasons. Thus, 13 young, healthy Chinese male adults completed both arms of the study, and their characteristics are shown in Table 2.
The CGM glycaemic profiles for the LGI 1 and LGI 2 treatments are graphically presented in Fig. The glycaemic outcome parameters are presented in Table 3. The black arrows represent the average meal times.
The rectangle indicates the second-meal effect. a Represents the breakfast portion of the incremental glucose curves for min; b represents the lunch portion; c represents the snack portion; d represents dinner portion. The solid black line represents the LGI 2 biscuits and the dashed lines represent the LGI 1 biscuits.
iAUC was calculated using the trapezoid rule ignoring the area below the baseline. Total iAUC corresponds to the area under the curve for the entire min of measurement.
e Represents the mean change from baseline postprandial insulin after breakfast over min. The iAUC for blood insulin concentration in the overall min after the breakfast bar plot. P value calculated using paired t test. At breakfast, the incremental insulin response to LGI 2 biscuits were significantly lower than to the LGI 1 biscuits in volunteers Fig.
The purpose of this study was to investigate the glycaemic effects of consuming two biscuits in the low GI range i. Modifying the biscuits with functional ingredients was essentially to create a healthy, nutrient-dense, high-fibre low GI biscuit LGI 2 that would favourably impact glucose metabolism and yet not increase overall energy intake.
Therefore, this novel low GI biscuit LGI 2 was created to be advantageous for body weight and glycaemic control. There was no effect on the second-meal glucose tolerance at standard lunch when LGI 2 biscuits were given.
Repeating the analysis for the iAUC of lunch while controlling for the iAUC of breakfast did not change the conclusions reported in Table 3 results not shown.
This again confirms that there was no residual effect of the breakfast onto lunch. Our results revealed a new finding with the most prominent effect on second-meal glucose tolerance observed at the dinner meal. The metabolic basis of this finding remains uncertain, but it has been shown that insulin resistance is higher at night than in the morning or during the day 17 , This results in a diurnal variation in insulin resistance and plasma FFA concentrations.
Since the second meal effect is related to suppression of plasma free fatty acid FFA concentrations 19 , it remains to be studied how consuming the LGI 2 biscuits affect the time course of plasma FFA concentration to the subsequent meal and over the course of the day.
When you eat rice, Fasting and longevity, or Guarana for Stamina other typical food reponse in Antidepressant for fibromyalgia, it GGlucose digested by the stomach and respknse Fasting and longevity, Glucosw it is absorbed into the blood as glucose. Figure 1 shows how it is absorbed into the body. When glucose enters the bloodstream, insulin facilitates its uptake into the body's cells. When an excess of glucose is ingested, insulin over secretion occurs. Insulin increases the biosynthesis of fat and suppresses its breakdown.
Ich wollte sehr mit Ihnen reden.
Ich entschuldige mich, aber meiner Meinung nach lassen Sie den Fehler zu. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden reden.
Und, was hier des Lächerlichen?