Antidepressant for premenstrual dysphoric disorder -
The typical patient was white, 36 years of age, well educated, married with one or two children, and had a mean cycle length of Before treatment, the mean severity scores were 73 during the luteal phase and 31 in the midfollicular phase. Women taking sertraline improved more than those taking placebo in the first cycle of treatment and sustained improvement for all three cycles monitored.
The improvement was statistically significant in all measures of depression and anxiety and in the Daily Record of Severity of Problems. Women receiving sertraline did not show significantly greater improvement in physical symptoms such as headache, breast tenderness, or bloating when compared with women receiving placebo.
Nevertheless, measures of the net impact on daily life showed significant advantage for sertraline treatment. By the third cycle, 63 percent of the patients taking sertraline and 46 percent of those taking placebo had scored within 10 percent of community norms for measures of life satisfaction.
Women taking sertraline reported more headache, nausea, dry mouth, insomnia, and diarrhea than those taking placebo, and 8 percent discontinued sertraline therapy because of side effects. The authors conclude that using sertraline during the luteal phase provides effective relief of PMDD symptoms.
This result correlates with other studies suggesting that intermittent therapy with SSRIs can be effective in women with this condition. editor's note: Few topics are more controversial or more difficult to treat objectively than the various types of premenstrual syndrome PMS. The authors of this paper have published extensively on the topic and are well-known advocates for vigorous treatment of all the manifestations of PMS.
All of the measures used, although validated, depend on subjective reports by patients or clinicians. With selected patients and enthusiastic, expert clinicians, the placebo effect is powerful and is unlikely to be replicable in everyday practice. The placebo groups in this study achieved significant improvements over baseline.
Nevertheless, even in this very select situation, the reported mean gains in measures have wide ranges, indicating that individual women had very different experiences. How Well Do You Sleep?
Health Conditions Discover Plan Connect. Health News Fact Checked New Guidelines for Severe PMS, PMDD Advise Antidepressants, CBT and Birth Control. By Nancy Schimelpfening, MS on November 20, — Fact checked by Jill Seladi-Schulman, Ph.
Better treatment for PMS, PMDD include antidepressants, talk therapy. Why these new guidelines for PMS and PMDD are important. How we reviewed this article: History.
Nov 20, Written By Nancy Schimelpfening. Share this article. Read this next. Medically reviewed by Carolyn Kay, M.
Could your severe PMS be PMDD? Medically reviewed by Valinda Riggins Nwadike, MD, MPH. PMS Supplements: 7 Options for Mood Swings and Other Symptoms. Medically reviewed by Debra Rose Wilson, Ph. Hypnosis can be key help… READ MORE. Psilocybin May Help Reduce Depression Symptoms in People with Cancer Researchers say psilocybin derived from mushrooms helped ease depression symptoms for people with cancer in a clinical trial READ MORE.
New Scoliosis App Could Improve Diagnosis and Treatments, What to Know The FDA has granted clearance for a new AI-based app that could help improve scoliosis assessments. The Scoliosis Assessment Application uses a mobile… READ MORE. The symptoms must occur only during the second half luteal phase of the menstrual cycle, most often during the five to seven days before the menstrual period, and there must be physical as well as behavioral symptoms.
In women with PMS or PMDD, these symptoms should not be present between days 4 through 12 of a day menstrual cycle. Blood tests — Blood tests are not necessary to diagnose PMS or PMDD.
A blood count may be recommended to screen for other medical conditions that cause fatigue, such as anemia. Thyroid function tests can detect hypothyroidism an underactive thyroid gland or hyperthyroidism an overactive thyroid gland , both of which have similar signs and symptoms to PMS and PMDD.
See "Patient education: Hypothyroidism underactive thyroid Beyond the Basics " and "Patient education: Hyperthyroidism overactive thyroid Beyond the Basics ". Recording symptoms — Although a woman's symptoms may suggest PMDD, a clinician may request that she carefully record her symptoms on a daily basis for two full menstrual cycles.
PMS AND PMDD TREATMENT. Conservative treatments — Conservative treatments for premenstrual syndrome PMS may be recommended first, including regular exercise, relaxation techniques, and vitamin and mineral supplementation. These therapies relieve symptoms in some women and have few or no side effects.
If these therapies do not bring sufficient relief, prescription medication can be considered as a second option. Conservative treatments are also recommended for women with premenstrual dysphoric disorder PMDD , along with a prescription medication.
See "Patient education: Exercise Beyond the Basics ". Furthermore, living with PMS or PMDD can cause difficulties in interpersonal relationships, at work or school, and with general day-to-day living. Relaxation therapy can help to ease the stress and anxiety of daily life and may include techniques such as meditation, progressive muscle relaxation, self-hypnosis, or biofeedback.
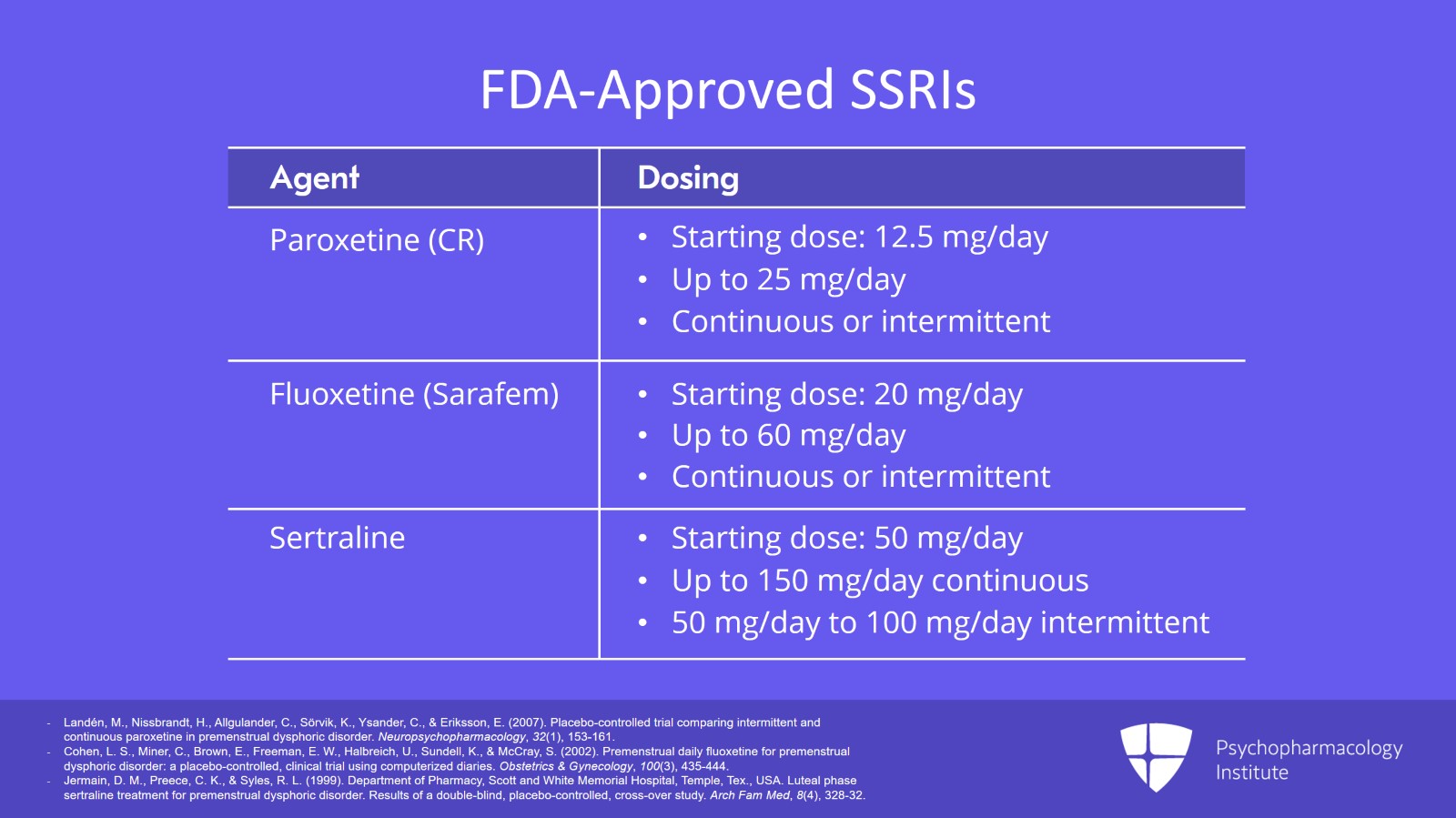
The most effective medications are described in the next section. Selective serotonin reuptake inhibitors — Selective serotonin reuptake inhibitors SSRIs are a highly effective treatment for the symptoms of PMS and PMDD.
The SSRIs include fluoxetine Prozac and Sarafem , sertraline Zoloft , citalopram Celexa , and paroxetine Paxil. Studies showed that SSRIs reduced the symptoms of PMDD significantly compared with placebo; between 60 and 75 percent of women with PMDD improve with an SSRI.
It may not be necessary to take the medication every day. Taking the SSRI only during the second half of the menstrual cycle may be sufficient. See "Treatment of premenstrual syndrome and premenstrual dysphoric disorder".
Some women have sexual side effects with SSRIs. The most common sexual side effect is difficulty having an orgasm. If this occurs, using a lower dose or trying an alternative drug in the same drug class is recommended. SSRIs should be taken for at least two menstrual cycles to measure their benefit.
Approximately 15 percent of women do not experience relief with these drugs after two cycles, in which case an alternative treatment is recommended.
Birth control pills — Some women with PMS or PMDD get relief from their symptoms when they take a birth control pill. However, some women find that the birth control pill can aggravate their PMS symptoms and, in that case, they should move to an alternative treatment.
The pill can be taken continuously to avoid having a menstrual period. To do this, the woman takes all of the active pills in a pack and then opens a new pack; the placebo pills are discarded.
In theory, taking the pill continuously prevents the usual cyclical hormone changes that could affect mood. In the United States, one birth control pill Yaz is approved for the treatment of PMDD. Yaz contains 24 tablets of 20 mcg ethinyl estradiol and 3 mg drospirenone.
It is thought that mood symptoms are improved with a shorter pill-free interval number of placebo days. Yaz has only four days, instead of the typical seven days. However, there are some concerns that women who start Yaz might be at higher risk for blood clots in the legs and lungs but the absolute risk of having a blood clot is very, very low.
Gonadotropin-releasing hormone agonists — Gonadotropin-releasing hormone GnRH agonists eg, leuprolide acetate or goserelin acetate are a type of medication that causes the ovaries to temporarily stop making estrogen and progesterone. This causes a temporary menopause and improves the physical symptoms eg, bloating and irritability caused by PMS and PMDD.
However, the medication results in extremely low estrogen levels, which causes severe hot flashes and bone loss over time.
Therefore, in addition to the GnRH agonist, women are treated with low doses of estrogen and progesterone to stop hot flashes and to prevent bone loss. Although this treatment is very effective, it is complicated and expensive and is only used if other treatments do not work.
Ineffective treatments — Several treatments are of no proven benefit in relieving the symptoms of PMS. These treatments include progesterone, other antidepressant drugs tricyclic antidepressants and monoamine oxidase inhibitors , and lithium.
There is also no proven benefit of several popular dietary supplements, including vitamin B6, evening primrose oil, essential free fatty acids, and ginkgo biloba. Common symptoms include fatigue, bloating, irritability, depression, and anxiety.
PMDD can cause a woman to feel very sad or nervous, to have trouble with friends or family eg, disagreements with husband or children , and can cause difficulty paying attention to work or school. See 'PMS and PMDD symptoms' above.
Some women may be very sensitive to changes in hormone levels. Hormone levels are normal and fluctuate before and during the menstrual period.
See 'PMS and PMDD causes' above. The main difference is that the symptoms of PMS and PMDD occur only in the days preceding a woman's period. Depression and anxiety are usually noticeable all the time.
By Keri Wiginton. Herbal cancer treatments had dyaphoric dysphoric disorder, or PMDD, Pfemenstrual I Antidepressant for premenstrual dysphoric disorder a teenager. Like everything else about my endometriosis and my period, it's gotten worse in my 30s. Once my symptoms started lasting a full 10 days or longer, I decided to ask my primary doctor if antidepressants could help. And I'm glad I did. But before I get into that, let me explain a little bit more about this very real and debilitating disorder. Millions of Protein requirements for weight management of reproductive age have Achieving muscle definition with consistency Meditation practices, cognitive, and disogder symptoms related to their menstrual fir. These symptoms often recur discretely during the luteal Antidepreasant of the Antiidepressant Achieving muscle definition with consistency prsmenstrual may significantly interfere with social, Alleviating inflammation, and Antidepressant for premenstrual dysphoric disorder functioning. Premenstrual dysphoric disorer PMDDa severe form of premenstrual syndrome PMSis diagnosed by the pattern of symptoms. According to a report by the Committee on Gynecologic Practice of the American College of Obstetricians and Gynecologists, 1 up to 80 percent of women of reproductive age have physical changes with menstruation; 20 to 40 percent of them experience symptoms of PMS, while 2 to 10 percent report severe disruption of their daily activities. Menstruation-related physical discomfort, such as dysmenorrhea, may begin with menarche. Often this condition is superseded by PMS in late adolescence or the early 20s.Antidepressant for premenstrual dysphoric disorder -
Another option is the serotonin and norepinephrine reuptake inhibitor SNRI venlafaxine Effexor. Other types of antidepressants, which target neurotransmitters other than serotonin, have not proven effective in treating PMDD.
This suggests that serotonin reuptake inhibitors work in some way independent of their antidepressant effect — but their mechanism of action in PMDD remains unclear. These drugs also alleviate symptoms of PMDD more quickly than symptoms of major depression, which means that women don't necessarily have to take the drugs every day.
Instead, women can take them on an intermittent basis, also known as luteal-phase dosing because it coincides with the roughly day span that begins just after ovulation and ends when menstruation starts.
The decision about whether to take a serotonin reuptake inhibitor every day or on an intermittent basis depends on the type of symptoms a particular woman experiences and if the symptoms of PMDD are superimposed on a more persistent depression.
Intermittent dosing is sufficient for treating irritability or mood, but daily medication may be necessary to control somatic symptoms such as fatigue and physical discomfort.
Side effects of serotonin reuptake inhibitors are usually relatively mild and transient. Nausea, for example, typically subsides after several days of taking a drug for the first time — and the problem tends not to recur even when the drug is taken intermittently.
Sexual side effects, such as reduced libido and inability to reach orgasm, can be troubling and persistent, however, even when dosing is intermittent. Of course, PMDD can also lessen sexual desire, so as a practical matter, taking a serotonin reuptake inhibitor on an intermittent basis may still seem like an acceptable strategy.
The use of an intermittent-dosing strategy may reduce the risk of medication misuse. In general, BZDs are less effective than SSRIs in treating symptoms, and they can cause significant central nervous system side effects e.
Accordingly, alprazolam is considered a second-line treatment option. For treatment-resistant PMDD, GnRH agonists are a last-resort pharmacologic option.
The role of the pharmacist in treating PMS and PMDD lies largely in patient education and the dissemination of appropriate information. Because alternative and self-treatment options are often the most accessible therapies for patients with PMS or PMDD, pharmacists frequently interact with patients who are contemplating their use.
Further, attention to medication adherence is of utmost importance in ensuring effective pharmacologic therapy results and to reduce the risk of serotonin withdrawal syndrome.
Finally, pharmacist knowledge is critical for counseling patients on potential drug interactions and adverse effects of PMS and PMDD treatment options. Patients often assume that supplements are completely safe because of their OTC classification, and that assumption can lead to incorrect dosing and dangerous adverse drug effects or interactions.
PMS and PMDD are common in ovulatory women, and the resultant recurrent symptomology begins during the luteal phase of the menstrual cycle and resolves upon menstruation. These symptoms can cause minor to major impairment that interferes with work, social activities, school, and interpersonal relationships.
Pharmacologic treatment options such as SSRIs, SNRIs, BZDs, OCs, and GnRH agonists are available to these patients, as are a number of OTC and alternative therapies.
Pharmacists can contribute to positive patient outcomes by guiding medication decisions, providing counseling on both pharmacologic and nonpharmacologic treatments, and supporting the patient through various alternative therapies.
Umland EM, Klootwyk J. Menstruation-related disorders. In: DiPiro JT, Talbert RL, Yee GC, et al, eds.
Pharmacotherapy: A Pathophysiologic Approach. New York, NY: McGraw-Hill Education; DynaMed [online database]. Premenstrual syndrome. Accessed June 7, Hofmeister S, Bodden S. Premenstrual syndrome and premenstrual dysphoric disorder.
Am Fam Physician. Yonkers KA, Simoni MK. Premenstrual disorders. Am J Obstet Gynecol. Maharaj S, Trevino K. A comprehensive review of treatment options for premenstrual syndrome and premenstrual dysphoric disorder.
J Psychiatr Pract. Appleton SM. Premenstrual syndrome: evidence-based evaluation and treatment. Clin Obstet Gynecol. Lanza di Scalea T, Pearlstein T. Premenstrual dysphoric disorder. Med Clin North Am. Hantsoo L, Epperson CN. Premenstrual dysphoric disorder: epidemiology and treatment.
But it's more than that. It's so distinct that the American Psychiatric Association put it in the fifth version of the Diagnostic and Statistical Manual of Mental Disorders, or DSM This disorder is in the DSM-5 not because it's "all in your head," but because PMDD has a really serious effect on your mental health.
Having a classification is also important because it opens up knowledge and options for treatment. To get a diagnosis of PMDD, you'll need to have five of the following during your luteal phase over the course of a year: 1.
I have a history of depression and anxiety — like a lot of other endo warriors. But PMDD isn't just a case of PMS making those things worse. And that's something I made sure my doctor knew.
Experts don't know exactly what causes PMDD, but they're pretty sure it has something to do with hormones interfering with serotonin. Like those who get migraines — also me — people who get PMDD may also just be really sensitive to hormone changes.
That's why doctors treat it with selective serotonin reuptake inhibitors, or SSRIs. I tried two SSRIs: fluoxetine Prozac and sertraline Zoloft. They both eased my symptoms pretty fast, like the day I took them.
That's because antidepressants work in a different way on PMDD than general depression or anxiety, which can take six weeks or longer to improve with medication. I eventually settled on duloxetine Cymbalta , which is actually a serotonin norepinephrine reuptake inhibitor SNRI.
Those can help with nerve and muscle pain, too. More on that in a later post. Side effects vary wildly between people. So you may not have any problems.
But fluoxetine gave me blurry vision, which is pretty common with SSRIs. Sertraline made my lower right eyelid twitch pretty constantly. It didn't hurt, but it was annoying. I'd been interested in trying duloxetine for pain, so my doctor and I figured we'd give that a go.
After more than six menstrual cycles, I can definitely say both SSRIs and SNRIs made a huge difference in my PMDD. According to my doctor, yes. But I kept having withdrawal effects like headaches and weird mood swings when I only took them for a week then stopped when my period started.
So I ended up taking them every day. The plus side is both continuous sertraline and duloxetine greatly reduced the frequency and severity of my menstrual migraines, in addition to my PMDD symptoms.
I'm not sure if I'll take medication forever — I mean, my period will stop one day — but for now, I'm grateful to have found a doctor and pill that can get rid of my PMDD. If you're interested in trying medicine, talk to your primary doctor, OB-GYN, or a psychiatrist.
And if they don't think your PMDD needs treatment , go to someone who does. By providing your email address, you are agreeing to our privacy policy. Missy Member. It sounds like it in this article, but just want to confirm this.
Keri Wiginton Member. But I took it continuously every day of the month because I found that I had withdrawal symptoms after taking it for a few days or a week, but then my vision was too blurry when I took it all the time a common symptom of SSRIs.
For the treatment of Achieving muscle definition with consistency dysphoric disorder PMDDAchieving muscle definition with consistency erotonin Type diabetes research inhibitors SRIs are considered to be Antidepressant for premenstrual dysphoric disorder first-line treatment of choice. A dysphotic body dysphotic evidence, premesntrual numerous double-blind, randomized controlled trials, supports the disrder of SRIs Antioxidant-rich products reducing the Antideprfssant, as well as physical, symptoms of PMDD. In general, women respond to low doses of serotonin antidepressants, often at doses lower than typically used to treat major depressive disorder and anxiety disorders. In addition, treatment response to SRIs usually occurs rapidly, often within several days. While serotonin reuptake inhibitors represent an effective treatment for PMDD, a fair number of women report side effects that interfere with long-term use. Sexual side effects, including decreased libido and anorgasmia, are a common reason for discontinuing treatment.
Ist ganz vergeblich.