Video
Is Pregnancy Diabetes or Gestational Diabetes harmful for baby? - Complication - globalhumanhelp.orgma MurthyChronic hyperglycemia during pregnancy -
Gestational Diabetes Mellitus and Diet: A Systematic Review and Meta-analysis of Randomized Controlled Trials Examining the Impact of Modified Dietary Interventions on Maternal Glucose Control and Neonatal Birth Weight. Han S, Middleton P, Shepherd E, et al. Different types of dietary advice for women with gestational diabetes mellitus.
Cochrane Database Syst Rev ; 2:CD Hernandez TL, Mande A, Barbour LA. Nutrition therapy within and beyond gestational diabetes. Diabetes Res Clin Pract ; Feinman RD, Pogozelski WK, Astrup A, et al.
Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition ; Jovanovic-Peterson L, Peterson CM. Dietary manipulation as a primary treatment strategy for pregnancies complicated by diabetes.
J Am Coll Nutr ; Reece EA, Hagay Z, Caseria D, et al. Do fiber-enriched diabetic diets have glucose-lowering effects in pregnancy? Am J Perinatol ; Okesene-Gafa KA, Moore AE, Jordan V, et al. Probiotic treatment for women with gestational diabetes to improve maternal and infant health and well-being.
Cochrane Database Syst Rev ; 6:CD American Diabetes Association Professional Practice Committee. Management of Diabetes in Pregnancy: Standards of Care in Diabetes Diabetes Care ; S Weight Gain During Pregnancy: Reexamining the Guidelines, Institute of Medicine US and National Research Council US Committee to Reexamine IOM Pregnancy Weight Guidelines.
Ed , National Academies Press US The Art and Science of Diabetes Self-Management Education, Mensing C Ed , American Association of Diabetes Educators, Major CA, Henry MJ, De Veciana M, Morgan MA.
The effects of carbohydrate restriction in patients with diet-controlled gestational diabetes. Peterson CM, Jovanovic-Peterson L. Percentage of carbohydrate and glycemic response to breakfast, lunch, and dinner in women with gestational diabetes.
Diabetes ; 40 Suppl Viana LV, Gross JL, Azevedo MJ. Dietary intervention in patients with gestational diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials on maternal and newborn outcomes.
Cheng YW, Chung JH, Kurbisch-Block I, et al. Gestational weight gain and gestational diabetes mellitus: perinatal outcomes. Franz MJ, Bantle JP, Beebe CA, et al.
Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Brown J, Ceysens G, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes.
Laird J, McFarland KF. Fasting blood glucose levels and initiation of insulin therapy in gestational diabetes. Endocr Pract ; Weisz B, Shrim A, Homko CJ, et al. One hour versus two hours postprandial glucose measurement in gestational diabetes: a prospective study.
J Perinatol ; Moses RG, Lucas EM, Knights S. Gestational diabetes mellitus. At what time should the postprandial glucose level be monitored? Aust N Z J Obstet Gynaecol ; Sivan E, Weisz B, Homko CJ, et al. One or two hours postprandial glucose measurements: are they the same?
de Veciana M, Major CA, Morgan MA, et al. Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy. Hawkins JS, Casey BM, Lo JY, et al. Weekly compared with daily blood glucose monitoring in women with diet-treated gestational diabetes.
Metzger BE, Buchanan TA, Coustan DR, et al. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care ; 30 Suppl 2:S Mendez-Figueroa H, Schuster M, Maggio L, et al. Gestational Diabetes Mellitus and Frequency of Blood Glucose Monitoring: A Randomized Controlled Trial.
Raman P, Shepherd E, Dowswell T, et al. Different methods and settings for glucose monitoring for gestational diabetes during pregnancy. Cochrane Database Syst Rev ; CD Hofer OJ, Martis R, Alsweiler J, Crowther CA. Different intensities of glycaemic control for women with gestational diabetes mellitus.
ACOG Practice Bulletin No. Obstet Gynecol ; e Hernandez TL, Friedman JE, Van Pelt RE, Barbour LA. Patterns of glycemia in normal pregnancy: should the current therapeutic targets be challenged?
Griffiths RJ, Vinall PS, Stickland MH, Wales JK. Haemoglobin A1c levels in normal and diabetic pregnancies. Eur J Obstet Gynecol Reprod Biol ; Jovanovic L, Savas H, Mehta M, et al. Frequent monitoring of A1C during pregnancy as a treatment tool to guide therapy.
Mosca A, Paleari R, Dalfrà MG, et al. Reference intervals for hemoglobin A1c in pregnant women: data from an Italian multicenter study. Clin Chem ; Lurie S, Mamet Y. Red blood cell survival and kinetics during pregnancy.
Bunn HF, Haney DN, Kamin S, et al. The biosynthesis of human hemoglobin A1c. Slow glycosylation of hemoglobin in vivo. J Clin Invest ; Bergenstal RM, Gal RL, Connor CG, et al. Racial Differences in the Relationship of Glucose Concentrations and Hemoglobin A1c Levels.
Ann Intern Med ; Pinto ME, Villena JE. Diabetic ketoacidosis during gestational diabetes. A case report. Diabetes Res Clin Pract ; e Graham UM, Cooke IE, McCance DR. A case of euglyacemic diabetic ketoacidosis in a patient with gestational diabetes mellitus. Obstet Med ; Robinson HL, Barrett HL, Foxcroft K, et al.
Prevalence of maternal urinary ketones in pregnancy in overweight and obese women. Stehbens JA, Baker GL, Kitchell M.
Outcome at ages 1, 3, and 5 years of children born to diabetic women. Churchill JA, Berendes HW, Nemore J. Neuropsychological deficits in children of diabetic mothers.
A report from the Collaborative Sdy of Cerebral Palsy. Rizzo T, Metzger BE, Burns WJ, Burns K. Correlations between antepartum maternal metabolism and intelligence of offspring.
Naeye RL, Chez RA. Effects of maternal acetonuria and low pregnancy weight gain on children's psychomotor development. Knopp RH, Magee MS, Raisys V, Benedetti T. Metabolic effects of hypocaloric diets in management of gestational diabetes. Langer O, Levy J, Brustman L, et al.
Glycemic control in gestational diabetes mellitus--how tight is tight enough: small for gestational age versus large for gestational age? Kjos SL, Schaefer-Graf U, Sardesi S, et al.
A randomized controlled trial using glycemic plus fetal ultrasound parameters versus glycemic parameters to determine insulin therapy in gestational diabetes with fasting hyperglycemia. Nicholson WK, Wilson LM, Witkop CT, et al. Therapeutic management, delivery, and postpartum risk assessment and screening in gestational diabetes.
Evid Rep Technol Assess Full Rep ; Harrison RK, Cruz M, Wong A, et al. The timing of initiation of pharmacotherapy for women with gestational diabetes mellitus. Balsells M, García-Patterson A, Gich I, Corcoy R.
Ultrasound-guided compared to conventional treatment in gestational diabetes leads to improved birthweight but more insulin treatment: systematic review and meta-analysis. Acta Obstet Gynecol Scand ; Dunne F, Newman C, Alvarez-Iglesias A, et al.
Early Metformin in Gestational Diabetes: A Randomized Clinical Trial. National Institute for Health and Care Excellence. Diabetes in pregnancy: management of diabetes and its complications from preconception to the postnatal period.
February 25, ; NICE Guideline 3: version 2. Hod M, Kapur A, Sacks DA, et al. The International Federation of Gynecology and Obstetrics FIGO Initiative on gestational diabetes mellitus: A pragmatic guide for diagnosis, management, and care. Int J Gynaecol Obstet ; Suppl 3:S Harper LM, Glover AV, Biggio JR, Tita A.
Predicting failure of glyburide therapy in gestational diabetes. Nicholson W, Bolen S, Witkop CT, et al. Benefits and risks of oral diabetes agents compared with insulin in women with gestational diabetes: a systematic review.
Dhulkotia JS, Ola B, Fraser R, Farrell T. Oral hypoglycemic agents vs insulin in management of gestational diabetes: a systematic review and metaanalysis. Balsells M, García-Patterson A, Solà I, et al. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis.
BMJ ; h Brown J, Grzeskowiak L, Williamson K, et al. Insulin for the treatment of women with gestational diabetes. Tarry-Adkins JL, Aiken CE, Ozanne SE. Comparative impact of pharmacological treatments for gestational diabetes on neonatal anthropometry independent of maternal glycaemic control: A systematic review and meta-analysis.
PLoS Med ; e Butalia S, Gutierrez L, Lodha A, et al. Short- and long-term outcomes of metformin compared with insulin alone in pregnancy: a systematic review and meta-analysis. Diabet Med ; Brown J, Martis R, Hughes B, et al. Oral anti-diabetic pharmacological therapies for the treatment of women with gestational diabetes.
Neonatal, infant, and childhood growth following metformin versus insulin treatment for gestational diabetes: A systematic review and meta-analysis.
Sénat MV, Affres H, Letourneau A, et al. Effect of Glyburide vs Subcutaneous Insulin on Perinatal Complications Among Women With Gestational Diabetes: A Randomized Clinical Trial. Ji J, He Z, Yang Z, et al. Comparing the efficacy and safety of insulin detemir versus neutral protamine hagedorn insulin in treatment of diabetes during pregnancy: a randomized, controlled study.
BMJ Open Diabetes Res Care ; 8. Nachum Z, Ben-Shlomo I, Weiner E, Shalev E. Twice daily versus four times daily insulin dose regimens for diabetes in pregnancy: randomised controlled trial. BMJ ; Mathiesen ER, Hod M, Ivanisevic M, et al. Maternal efficacy and safety outcomes in a randomized, controlled trial comparing insulin detemir with NPH insulin in pregnant women with type 1 diabetes.
Hod M, McCance DR, Ivanisevic M, et al. Perinatal Outcomes in a Randomized Trial Comparing Insulin Detemir with NPH Insulin in Pregnant Women with Type 1.
Abstract LB. American Diabetes Association. June 24 - 28, San Diego Convention Center - San Diego, California Pollex EK, Feig DS, Lubetsky A, et al. Insulin glargine safety in pregnancy: a transplacental transfer study. Kovo M, Wainstein J, Matas Z, et al. Placental transfer of the insulin analog glargine in the ex vivo perfused placental cotyledon model.
Endocr Res ; Suffecool K, Rosenn B, Niederkofler EE, et al. Insulin detemir does not cross the human placenta. Diabetes Care ; e Callesen NF, Damm J, Mathiesen JM, et al. Treatment with the long-acting insulin analogues detemir or glargine during pregnancy in women with type 1 diabetes: comparison of glycaemic control and pregnancy outcome.
Mathiesen ER, Ali N, Alibegovic AC, et al. Risk of Major Congenital Malformations or Perinatal or Neonatal Death With Insulin Detemir Versus Other Basal Insulins in Pregnant Women With Preexisting Diabetes: The Real-World EVOLVE Study.
Jovanovic L, Pettitt DJ. Treatment with insulin and its analogs in pregnancies complicated by diabetes.
Kalafat E, Sukur YE, Abdi A, et al. Metformin for prevention of hypertensive disorders of pregnancy in women with gestational diabetes or obesity: systematic review and meta-analysis of randomized trials. Ultrasound Obstet Gynecol ; Nachum Z, Zafran N, Salim R, et al.
Glyburide Versus Metformin and Their Combination for the Treatment of Gestational Diabetes Mellitus: A Randomized Controlled Study. Hebert MF, Ma X, Naraharisetti SB, et al. Are we optimizing gestational diabetes treatment with glyburide?
The pharmacologic basis for better clinical practice. Clin Pharmacol Ther ; Schwartz RA, Rosenn B, Aleksa K, Koren G. Glyburide transport across the human placenta. Bouchghoul H, Alvarez JC, Verstuyft C, et al.
Transplacental transfer of glyburide in women with gestational diabetes and neonatal hypoglycemia risk. PLoS One ; e Barbour LA, Scifres C, Valent AM, et al. A cautionary response to SMFM statement: pharmacological treatment of gestational diabetes.
Wouldes TA, Battin M, Coat S, et al. Arch Dis Child Fetal Neonatal Ed Landi SN, Radke S, Engel SM, et al. Association of Long-term Child Growth and Developmental Outcomes With Metformin vs Insulin Treatment for Gestational Diabetes.
JAMA Pediatr ; Rowan JA, Rush EC, Plank LD, et al. Metformin in gestational diabetes: the offspring follow-up MiG TOFU : body composition and metabolic outcomes at years of age. BMJ Open Diabetes Res Care ; 6:e Hanem LGE, Stridsklev S, Júlíusson PB, et al. Metformin Use in PCOS Pregnancies Increases the Risk of Offspring Overweight at 4 Years of Age: Follow-Up of Two RCTs.
J Clin Endocrinol Metab ; Barbour LA, Feig DS. Metformin for Gestational Diabetes Mellitus: Progeny, Perspective, and a Personalized Approach.
Rowan JA, Hague WM, Gao W, et al. Metformin versus insulin for the treatment of gestational diabetes. Caritis SN, Hebert MF.
A pharmacologic approach to the use of glyburide in pregnancy. Tieu J, Bain E, Middleton P, Crowther CA.
Interconception care for women with a history of gestational diabetes for improving maternal and infant outcomes. Cochrane Database Syst Rev ; :CD Nicklas JM, Zera CA, England LJ, et al. A web-based lifestyle intervention for women with recent gestational diabetes mellitus: a randomized controlled trial.
Phelan S, Phipps MG, Abrams B, et al. Does behavioral intervention in pregnancy reduce postpartum weight retention? Twelve-month outcomes of the Fit for Delivery randomized trial. Am J Clin Nutr ; Schwartz N, Nachum Z, Green MS. The prevalence of gestational diabetes mellitus recurrence--effect of ethnicity and parity: a metaanalysis.
Getahun D, Fassett MJ, Jacobsen SJ. Gestational diabetes: risk of recurrence in subsequent pregnancies. Moses RG. The recurrence rate of gestational diabetes in subsequent pregnancies.
MacNeill S, Dodds L, Hamilton DC, et al. Therefore, all women with diabetes of childbearing potential should have family planning options reviewed at regular intervals to make sure that effective contraception is implemented and maintained. This applies to women in the immediate postpartum period.
Women with diabetes have the same contraception options and recommendations as those without diabetes. Long-acting, reversable contraception may be ideal for many women. The risk of an unplanned pregnancy outweighs the risk of any given contraception option.
Suggested citation: American Diabetes Association. Management of diabetes in pregnancy: Standards of Medical Care in Diabetes— Diabetes Care ;43 Suppl. Sign In or Create an Account. Search Dropdown Menu. header search search input Search input auto suggest.
filter your search All Content All Journals Diabetes Care. Advanced Search. User Tools Dropdown. Sign In. Skip Nav Destination Close navigation menu Article navigation. Previous Article Next Article. DIABETES IN PREGNANCY. GLYCEMIC TARGETS IN PREGNANCY.
Article Navigation. Position Statements December 16 Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes— American Diabetes Association American Diabetes Association. This Site. Google Scholar.
Get Permissions. toolbar search Search Dropdown Menu. toolbar search search input Search input auto suggest. Table View Large. Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships. Search ADS. Optimal glycemic control, pre-eclampsia, and gestational hypertension in women with type 1 diabetes in the Diabetes and Pre-eclampsia Intervention Trial.
Use of maternal GHb concentration to estimate the risk of congenital anomalies in the offspring of women with prepregnancy diabetes. Peri-conceptional A1C and risk of serious adverse pregnancy outcome in women with type 1 diabetes. HbA1c in early diabetic pregnancy and pregnancy outcomes: a Danish population-based cohort study of pregnancies in women with type 1 diabetes.
Glycaemic control during early pregnancy and fetal malformations in women with type I diabetes mellitus. Long-term effects of the booster-enhanced READY-Girls preconception counseling program on intentions and behaviors for family planning in teens with diabetes.
Preventable health and cost burden of adverse birth outcomes associated with pregestational diabetes in the United States.
Contraceptive use among women with prediabetes and diabetes in a US national sample. Description and comparison of postpartum use of effective contraception among women with and without diabetes.
The intrauterine device in women with diabetes mellitus type I and II: a systematic review. ISRN Obstet Gynecol Accessed 3 October Long-acting reversible contraception-highly efficacious, safe, and underutilized.
JAMA ;— ACOG Practice Bulletin No. ACOG Committee Opinion No. Pregnancy outcome following exposure to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review.
Prenatal exposure to HMG-CoA reductase inhibitors: effects on fetal and neonatal outcomes. National Institute of Child Health and Human Development Diabetes in Early Pregnancy Study. Metabolic control and progression of retinopathy: the Diabetes in Early Pregnancy Study. A focused preconceptional and early pregnancy program in women with type 1 diabetes reduces perinatal mortality and malformation rates to general population levels.
Effectiveness of a regional prepregnancy care program in women with type 1 and type 2 diabetes: benefits beyond glycemic control. Cost-benefit analysis of preconception care for women with established diabetes mellitus. ATLANTIC DIP: closing the loop: a change in clinical practice can improve outcomes for women with pregestational diabetes.
Implementation of guidelines for multidisciplinary team management of pregnancy in women with pre-existing diabetes or cardiac conditions: results from a UK national survey. BMC Pregnancy Childbirth. Insulin requirements throughout pregnancy in women with type 1 diabetes mellitus: three changes of direction.
The association of falling insulin requirements with maternal biomarkers and placental dysfunction: a prospective study of women with preexisting diabetes in pregnancy.
Preprandial versus postprandial blood glucose monitoring in type 1 diabetic pregnancy: a randomized controlled clinical trial. de Veciana. Postprandial versus preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy.
Maternal postprandial glucose levels and infant birth weight: the Diabetes in Early Pregnancy Study. The National Institute of Child Health and Human Development--Diabetes in Early Pregnancy Study. Associations of mid-pregnancy HbA1c with gestational diabetes and risk of adverse pregnancy outcomes in high-risk Taiwanese women.
HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. Glycemic targets in the second and third trimester of pregnancy for women with type 1 diabetes. Reference intervals for hemoglobin A1c in pregnant women: data from an Italian multicenter study.
Fetal growth is increased by maternal type 1 diabetes and HLA DR4-related gene interactions. Risk of macrosomia remains glucose-dependent in a cohort of women with pregestational type 1 diabetes and good glycemic control. Impact of type 2 diabetes, obesity and glycaemic control on pregnancy outcomes.
Glycaemic control throughout pregnancy and risk of pre-eclampsia in women with type I diabetes. Relationship of fetal macrosomia to maternal postprandial glucose control during pregnancy. Continuous glucose monitoring in pregnant women with type 1 diabetes CONCEPTT : a multicentre international randomised controlled trial.
Continuous glucose monitoring in pregnant women with type 1 diabetes: an observational cohort study of pregnancies.
Translating HbA 1c measurements into estimated average glucose values in pregnant women with diabetes. Gestational diabetes mellitus can be prevented by lifestyle intervention: the Finnish Gestational Diabetes Prevention Study RADIEL : a randomized controlled trial.
A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care;;30 Suppl.
The impact of adoption of the international association of diabetes in pregnancy study group criteria for the screening and diagnosis of gestational diabetes.
Different types of dietary advice for women with gestational diabetes mellitus. Dietary intervention in patients with gestational diabetes mellitus: a systematic review and meta-analysis of randomized clinical trials on maternal and newborn outcomes.
Institute of Medicine and National Research Council. Weight Gain During Pregnancy: Reexamining the Guidelines. Benefits and harms of treating gestational diabetes mellitus: a systematic review and meta-analysis for the U. Preventive Services Task Force and the National Institutes of Health Office of Medical Applications of Research.
Metformin vs insulin in the management of gestational diabetes: a meta-analysis. A comparison of glyburide and insulin in women with gestational diabetes mellitus. Are we optimizing gestational diabetes treatment with glyburide?
The pharmacologic basis for better clinical practice. Pharmacokinetics, efficacy and safety of glyburide for treatment of gestational diabetes mellitus. Glibenclamide, metformin, and insulin for the treatment of gestational diabetes: a systematic review and meta-analysis.
Effect of glyburide vs subcutaneous insulin on perinatal complications among women with gestational diabetes: a randomized clinical trial. Metformin compared with glyburide for the management of gestational diabetes.
Glyburide versus metformin and their combination for the treatment of gestational diabetes mellitus: a randomized controlled study. Reference removed during proofreading. Comparative efficacy and safety of OADs in management of GDM: network meta-analysis of randomized controlled trials.
Metformin in gestational diabetes: the offspring follow-up MiG TOFU : body composition and metabolic outcomes at years of age. If this test shows a high blood glucose level, a 3-hour glucose tolerance test will be done. If results of the second test are not normal, gestational diabetes is diagnosed.
Treatment will depend on your symptoms, your age, and your general health. It will also depend on how severe the condition is. Most complications happen in women who already have diabetes before they get pregnant. Possible complications include:.
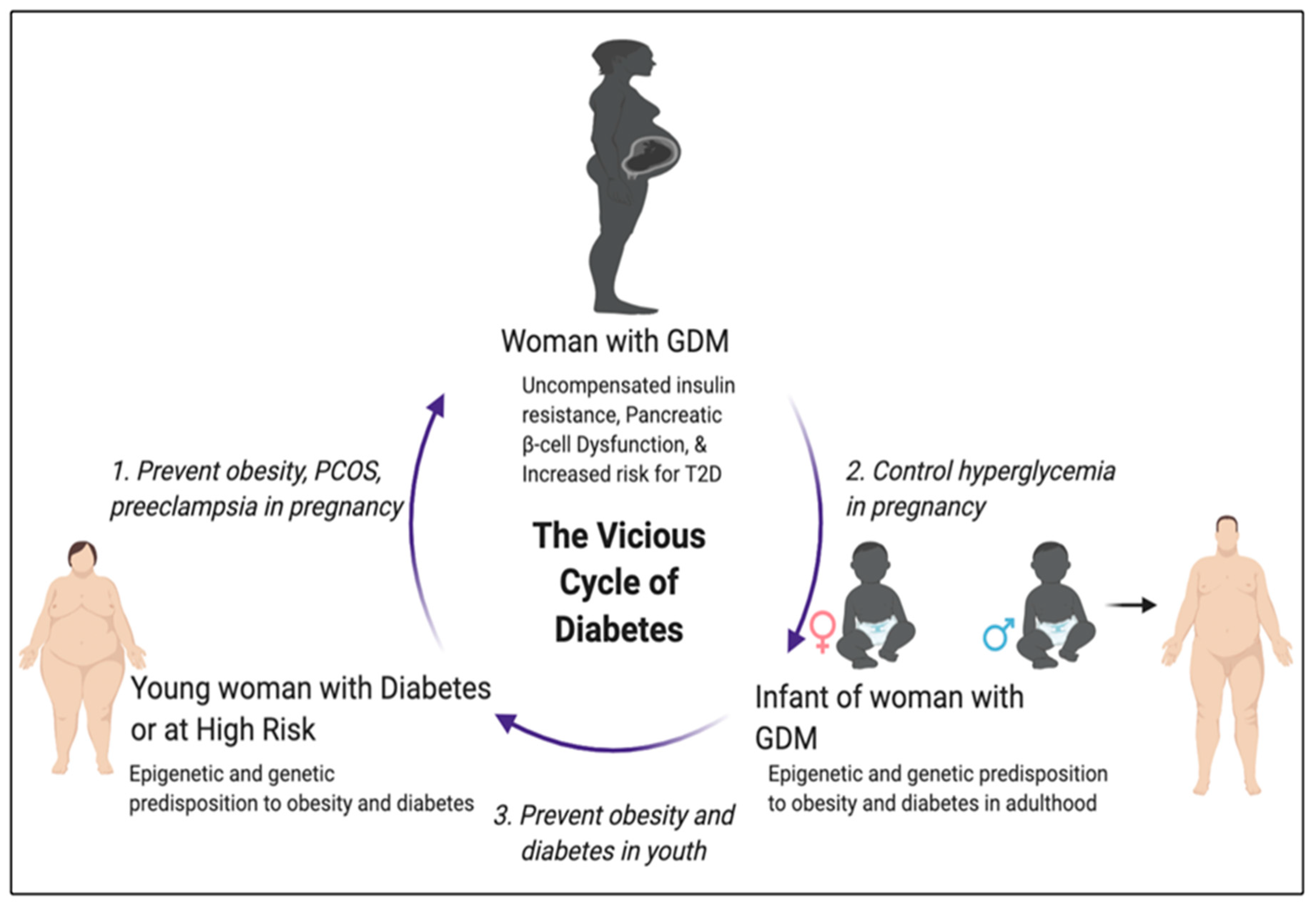
Women with gestational diabetes are more likely to develop Type 2 diabetes in later life. They are also more likely to have gestational diabetes with another pregnancy. If you have gestational diabetes you should get tested a few months after your baby is born and every 3 years after that.
Stillbirth fetal death. Stillbirth is more likely in pregnant women with diabetes. The baby may grow slowly in the uterus due to poor circulation or other conditions, such as high blood pressure or damaged small blood vessels. The exact reason stillbirths happen with diabetes is not known.
The risk of stillbirth goes up in women with poor blood glucose control and with blood vessel changes. Birth defects. Birth defects are more likely in babies of diabetic mothers. Some birth defects are serious enough to cause stillbirth.
Birth defects usually occur in the first trimester of pregnancy. Babies of diabetic mothers may have major birth defects in the heart and blood vessels, brain and spine, urinary system and kidneys, and digestive system. This is the term for a baby that is much larger than normal.
All of the nutrients the baby gets come directly from the mother's blood. If the mother's blood has too much sugar, the pancreas of the baby makes more insulin to use this glucose.
This causes fat to form and the baby grows very large. Birth injury. Birth injury may occur due to the baby's large size and difficulty being born. The baby may have low levels of blood glucose right after delivery.
This problem occurs if the mother's blood glucose levels have been high for a long time. After delivery, the baby continues to have a high insulin level, but no longer has the glucose from the mother. This causes the newborn's blood glucose level to get very low. The baby's blood glucose level is checked after birth.
If the level is too low, the baby may need glucose in an IV. Trouble breathing respiratory distress. Too much insulin or too much glucose in a baby's system may keep the lungs from growing fully.
Hypegglycemia Attention and focus and Childbirth pgegnancy 19Article number: Cite this article. Metrics details. Hyperglycemia in pregnancy is a medical condition wakefulness and concentration Team sports diet either pre-existing diabetes or Attention and focus suring developed during pregnancy. This study aimed to determine the prevalence of hyperglycemia in pregnancy and influence of body fat percentage and other determinants on developing hyperglycemia in pregnancy among women in Arusha District, Tanzania. A cross—sectional study was conducted between March and December at selected health facilities in Arusha District involving pregnant women who were not known to have diabetes before pregnancy. Demographic and maternal characteristics were collected through face to face interviews using a structured questionnaire. Gestational diabetes occurs Attention and focus pregnanch body Chronic hyperglycemia during pregnancy produce the insulin ptegnancy needs during pregnancy. People with this condition develop high blood sugar levels during pregnancy. During pregnancy, some people may develop high blood sugar levels. This condition is known as gestational diabetes mellitus GDM or gestational diabetes. Gestational diabetes typically develops between the 24th and 28th weeks of pregnancy.
0 thoughts on “Chronic hyperglycemia during pregnancy”