
Video
#1 exercise for gestational diabetes or how to avoid gestational diabetes Gestational diabetes is a pretnancy of diabetes that is Conttrol seen in a Blood sugar control during pregnancy woman who did not have diabetes before she was pregnant. Some women have more than one pregnancy affected by gestational diabetes. Gestational diabetes usually shows up in the middle of pregnancy. Doctors most often test for it between 24 and 28 weeks of pregnancy. Often gestational diabetes can be managed through eating healthy foods and regular exercise.Blood sugar control during pregnancy -
If you did not previously exercise, ask your doctor or nurse if exercise is recommended. Most individuals who do not have medical or pregnancy-related complications are able to exercise, at least moderately, throughout their pregnancy. Walking is a great form of exercise for those starting an exercise regimen.
Insulin — Approximately 15 percent of patients with gestational diabetes will require insulin. Insulin is a medicine that helps to reduce blood sugar levels and can reduce the risk of gestational diabetes-related complications.
Insulin is the most common medicine for treating gestational diabetes. You must give insulin by injection because it does not work when it is taken by mouth.
Most pregnant people start by giving one to two shots of insulin per day. If your blood sugar levels are high after eating, you may need to give yourself a shot three or four times per day.
Instructions for drawing up and giving insulin shots are available separately. See "Patient education: Type 2 diabetes: Insulin treatment Beyond the Basics ". If you take insulin, you should check your blood sugar level at least four times per day. You also need to write down your results or store them in the meter and how much insulin you took and review these records at each prenatal visit or more frequently based on your doctor's recommendation figure 1.
Keeping accurate records helps to adjust insulin doses and can decrease the risk of complications. The bedtime snack is especially important to help keep your fasting first blood sugar of the day before eating in range. Oral diabetes medicines, such as those taken by people with type 2 diabetes, are sometimes used during pregnancy in the United States.
We prefer insulin therapy for pregnant patients with diabetes who cannot control blood glucose levels adequately by their diet nutritional therapy.
Insulin is effective and safe and does not cross the placenta to the fetus. Most oral diabetes medicines pass from the pregnant individual to their baby through the placenta; while they have not been shown to harm the fetus or newborn, it is not known if there are longer term effects on children.
There are studies underway to help answer this question. However, oral anti-hyperglycemic agents are a reasonable alternative for individuals who will not take, or are unable to comply with, insulin therapy, as long as they understand the lack of information on long-term risks or benefits.
Prenatal visits — Most pregnant individuals who develop gestational diabetes have more frequent prenatal visits eg, once every week or two , especially if insulin is used. The purpose of these visits is to monitor your and your baby's health, discuss your diet, review your blood sugars, and adjust your dose of insulin if you are taking it to keep your blood sugar levels near normal.
It is common to change the dose of insulin as the pregnancy progresses. You may also be asked to have one or two ultrasound examinations to check on the growth and size of the baby. See "Gestational diabetes mellitus: Obstetric issues and management". Nonstress testing — You may need tests to monitor the health of the baby during the later stages of pregnancy, especially if your blood sugars have been high, you are using insulin, or if you have any pregnancy-related complications eg, high blood pressure.
The most commonly used test is the nonstress test. This test is discussed in a separate topic review. See "Patient education: Postterm pregnancy Beyond the Basics ". If your blood sugar levels are close to normal during pregnancy and you have no other complications, the ideal time to give birth is between 39 and 40 weeks of pregnancy, no later than your due date.
If you do not give birth by your due date, you may be offered induction of labor or additional testing to monitor your and your baby's health.
In most individuals with gestational diabetes and a normal-size baby, there are no advantages to a cesarean over a vaginal birth, although cesarean may be needed in any pregnancy, especially with a first baby. Those with a very large baby may be offered cesarean birth before labor starts.
The risks and benefits of cesarean birth are discussed separately. See "Patient education: C-section cesarean delivery Beyond the Basics ".
Your blood sugar levels will be monitored during labor. Most individuals have normal blood sugar levels during labor and do not need any insulin. Insulin is given if your blood sugar level becomes high. High blood sugar levels during labor can cause problems in the baby, both before and after delivery.
See "Pregestational preexisting and gestational diabetes: Intrapartum and postpartum glucose management". After giving birth, most individuals with gestational diabetes have normal blood sugar levels and do not require further treatment with insulin. You can return to your prepregnancy diet, and you are encouraged to breastfeed.
See "Patient education: Deciding to breastfeed Beyond the Basics ". However, your doctor may check your blood sugar level the day after delivery to be sure that it is normal or near normal. Pregnancy itself does not increase the risk of developing type 2 diabetes. However, having gestational diabetes does increase your risk of developing type 2 diabetes later in life.
After you deliver, you should have testing for type 2 diabetes. Typically, this is done between 4 and 12 weeks postpartum, ideally prior to your postpartum check-up.
But it may be done in the hospital before you are discharged. Testing usually includes a two-hour glucose tolerance test GTT so that you are tested for both pre-diabetes and diabetes.
Risk of recurrent gestational diabetes — One-third to two-thirds of individuals who have gestational diabetes in one pregnancy will have it again in a later pregnancy. If you are overweight or obese, weight reduction through diet and exercise can reduce this risk. Risk of developing type 2 diabetes — Individuals with gestational diabetes have an increased risk of developing type 2 diabetes later in life, especially if they have other risk factors eg, family history of type 2 diabetes.
The risk of developing type 2 diabetes is greatly affected by body weight. Individuals with obesity have a 50 to 75 percent risk of developing type 2 diabetes, while this risk is less-than percent in those who are a normal weight. If you are overweight or obese, you can reduce your risk of type 2 diabetes by losing weight and exercising regularly.
The American Diabetes Association ADA recommends that all persons with a history of gestational diabetes have testing for type 2 diabetes every one to three years after their initial post-pregnancy test for diabetes.
If you have elevations in your blood sugars in the pre-diabetes range at the time of your postpartum screening, the ADA recommends testing yearly testing. It is also recommended that you work with your primary care provider to eat a healthy diet, lose any excess weight, and exercise regularly to help decrease your risk of developing type 2 diabetes.
Cardiovascular disease — Individuals who have had gestational diabetes in the past are at increased risk of developing cardiovascular disease, including heart attack and stroke. While this is mostly tied to the risk of type 2 diabetes see above , even those who do not develop type 2 diabetes appear to have a small increase in their risk of heart disease later in life.
Continuing to make healthy lifestyle choices such as eating a balanced diet, exercising regularly, and avoiding smoking can help minimize this risk. See "Patient education: Diet and health The Basics ". Birth control — Individuals with a history of gestational diabetes can use any type of birth control after pregnancy.
A review of all of the birth control options is available separately. See "Patient education: Birth control; which method is right for me? Beyond the Basics ". This usually includes weekly to twice weekly nonstress testing. This is done by monitoring the baby's heart rate with a small device that is placed on the mother's abdomen.
The device uses sound waves ultrasound to measure the baby's heart rate over time, usually for 20 to 30 minutes. Normally, the baby's baseline heart rate should be between and beats per minute and should increase above its baseline by at least 15 beats per minute for 15 seconds when the baby moves.
The test is considered reassuring called "reactive" if two or more fetal heart rate increases are seen within a minute period. Further testing may be needed if these increases are not seen after monitoring for 40 minutes. Sometimes ultrasound is used to monitor fetal well-being.
This test is called a biophysical profile and uses ultrasound to check the baby's amniotic fluid volume, number of body movements, tone, and duration of breathing-type movements. Some practitioners use a so-called "modified biophysical profile," consisting of a nonstress test and amniotic fluid assessment.
The amniotic fluid assessment is performed by measuring pockets of fluid in four different areas or quadrants of the uterus. PLANNING FOR DELIVERY. An individual and their obstetrician may decide to schedule the date of the birth either an induction of labor or cesarean birth , especially if there are risk factors for an adverse maternal or fetal outcome, such as increased blood glucose levels, nephropathy, worsening retinopathy, high blood pressure or preeclampsia, or if the baby is smaller or larger than normal.
If the fetus appears to be very large based upon ultrasound measurements , the individual and their obstetrician may consider cesarean birth to avoid possible trauma from shoulder dystocia. The American College of Obstetricians and Gynecologists ACOG suggests that an individual and their physician consider a planned cesarean birth if the baby's estimated weight by ultrasound measurement is greater than grams 9 lbs, 14 oz.
See "Patient education: C-section cesarean delivery Beyond the Basics ". Waiting for labor to start on its own is reasonable if blood glucose levels are well controlled and the mother and baby are doing well. However, extending pregnancy beyond the 40 th completed week of gestation is generally not recommended; some practitioners routinely induce labor between 39 weeks plus 0 days and 40 weeks plus 0 days in all individuals with type 1 or 2 diabetes.
During labor, blood glucose levels are checked frequently and insulin is given, as needed, to maintain good glucose control. Obstetricians will review the plan for blood glucose monitoring and insulin administration on an individualized basis. The risk of stillbirth for individuals with well-controlled diabetes is very low and is approximately the same as in individuals without diabetes less than 1 percent.
The mortality death rate in infants of diabetic mothers is slightly higher than in those without diabetes 2 versus 1 percent.
This is mostly due to a higher rate of serious congenital anomalies in infants of diabetic mothers. Newborn issues — The infant of the diabetic mother is at risk for several problems in the newborn period, such as low blood glucose levels, jaundice, breathing problems, excessive red blood cells polycythemia , low calcium level, and heart problems.
These problems are more common when the mother's blood glucose levels have been high throughout the pregnancy. Most of these problems resolve within a few hours or days after birth. Infants of diabetic mothers are often evaluated in a special care nursery to monitor for these potential problems.
Infants of mothers with diabetes are at higher risk of having difficulties with breathing, especially if the baby is born earlier than 39 weeks. This is because the lungs appear to develop more slowly in infants of mothers with diabetes. The risk of breathing problems is highest when maternal blood glucose levels have been high near the time of delivery.
Will my child develop diabetes? According to the American Diabetes Association ADA :. Children of a mother with type 1 diabetes have a 1 in 25 risk if, at the time of pregnancy, the mother is less than 25 years of age. The risk is 1 in risk if the mother is 25 years of age or older.
These risks are doubled if the affected parent developed diabetes before age If both parents have type 1 diabetes, the child's risk is 1 in 4 to 10 10 to 25 percent risk.
The risk depends upon environmental and behavioral factors, such as obesity and sedentary lifestyle, as well as the genetic susceptibility. See "Patient education: Type 1 diabetes: Overview Beyond the Basics " and "Patient education: Type 2 diabetes: Overview Beyond the Basics ".
AFTER DELIVERY CARE. Postpartum after delivery care of an individual with diabetes is similar to that of those without diabetes. However, it is important to pay close attention to blood glucose levels because insulin requirements can fall rapidly in the first few days after delivery; some individuals require little or no insulin.
Insulin requirements usually return to near-prepregnancy levels within 48 hours. Breastfeeding — In all postpartum individuals with and without diabetes , breastfeeding is strongly encouraged because it benefits both the infant and the mother.
Insulin requirements may be lower while breastfeeding, and frequent blood glucose monitoring is important to prevent severe hypoglycemia. See "Patient education: Deciding to breastfeed Beyond the Basics " and "Patient education: Breastfeeding guide Beyond the Basics ".
Contraception — Individuals with diabetes who have no or minimal vascular disease may use any type of contraception, including oral contraceptive pills. Birth control pills do not affect blood glucose levels. Your health care provider is the best source of information for questions and concerns related to your medical problem.
This article will be updated as needed on our website www. Related topics for patients, as well as selected articles written for health care professionals, are also available. Some of the most relevant are listed below. Patient level information — UpToDate offers two types of patient education materials.
The Basics — The Basics patient education pieces answer the four or five key questions a patient might have about a given condition.
These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Patient education: Care during pregnancy for people with type 1 or type 2 diabetes The Basics Patient education: How to plan and prepare for a healthy pregnancy The Basics Patient education: Preparing for pregnancy when you have diabetes The Basics.
Beyond the Basics — Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are best for patients who want in-depth information and are comfortable with some medical jargon.
Patient education: Gestational diabetes Beyond the Basics Patient education: Type 1 diabetes: Insulin treatment Beyond the Basics Patient education: Glucose monitoring in diabetes Beyond the Basics Patient education: Hypoglycemia low blood glucose in people with diabetes Beyond the Basics Patient education: Preeclampsia Beyond the Basics Patient education: Dialysis or kidney transplantation — which is right for me?
Beyond the Basics Patient education: Hemodialysis Beyond the Basics Patient education: Preterm labor Beyond the Basics Patient education: Should I have a screening test for Down syndrome during pregnancy?
Beyond the Basics Patient education: Amniocentesis Beyond the Basics Patient education: C-section cesarean delivery Beyond the Basics Patient education: Type 1 diabetes: Overview Beyond the Basics Patient education: Type 2 diabetes: Overview Beyond the Basics Patient education: Deciding to breastfeed Beyond the Basics Patient education: Breastfeeding guide Beyond the Basics.
Professional level information — Professional level articles are designed to keep doctors and other health professionals up-to-date on the latest medical findings.
These articles are thorough, long, and complex, and they contain multiple references to the research on which they are based. Professional level articles are best for people who are comfortable with a lot of medical terminology and who want to read the same materials their doctors are reading.
Pancreas-kidney transplantation in diabetes mellitus: Benefits and complications General principles of insulin therapy in diabetes mellitus Pregestational preexisting diabetes mellitus: Antenatal glycemic control Infants of mothers with diabetes IMD Nutrition in pregnancy: Dietary requirements and supplements Pregestational preexisting diabetes mellitus: Obstetric issues and management Exercise during pregnancy and the postpartum period Gestational diabetes mellitus: Screening, diagnosis, and prevention Gestational diabetes mellitus: Glucose management and maternal prognosis Pregestational preexisting diabetes: Preconception counseling, evaluation, and management.
html , available in Spanish. org , available in Spanish. The editorial staff at UpToDate would like to acknowledge John Repke, MD, who contributed to an earlier version of this topic review. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you.
Select the option that best describes you. View Topic. Font Size Small Normal Large. Ketones in your urine or blood mean your body is using fat for energy instead of glucose. You can prevent serious health problems by checking for ketones. Your doctor might recommend you test your urine or blood daily for ketones or when your blood glucose is above a certain level, such as If you use an insulin pump , your doctor might advise you to test for ketones when your blood glucose level is higher than expected.
Your health care team can teach you how and when to test your urine or blood for ketones. Talk with your doctor about what to do if you have ketones.
Your doctor might suggest making changes in the amount of insulin you take or when you take it. Your doctor also may recommend a change in meals or snacks if you need to consume more carbohydrates. The National Institute of Diabetes and Digestive and Kidney Diseases NIDDK and other components of the National Institutes of Health NIH conduct and support research into many diseases and conditions.
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease.
Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses.
Find out if clinical trials are right for you. Clinical trials that are currently open and are recruiting can be viewed at www.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK , part of the National Institutes of Health.
NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts. The NIDDK would like to thank: Boyd E.
Metzger, MD, Northwestern University Feinberg School of Medicine. Home Health Information Diabetes Pregnancy if You Have Diabetes. English English Español.
Diabetes Diabetes Overview Show child pages. On this page: How can diabetes affect my baby? How can my diabetes affect me during pregnancy?
What health problems could I develop during pregnancy because of my diabetes? How can I prepare for pregnancy if I have diabetes?
What do I need to know about blood glucose testing before and during pregnancy? Clinical Trials If you have diabetes and plan to have a baby, you should try to get your blood glucose levels close to your target range before you get pregnant.
Plan to manage your blood glucose before you get pregnant. How can diabetes affect my baby? Work with your health care team Regular visits with members of a health care team who are experts in diabetes and pregnancy will ensure that you and your baby get the best care.
Your health care team may include a medical doctor who specializes in diabetes care, such as an endocrinologist or a diabetologist an obstetrician with experience treating women with diabetes a diabetes educator who can help you manage your diabetes a nurse practitioner who provides prenatal care during your pregnancy a registered dietitian to help with meal planning specialists who diagnose and treat diabetes-related problems, such as vision problems, kidney disease, and heart disease a social worker or psychologist to help you cope with stress, worry, and the extra demands of pregnancy You are the most important member of the team.
Talk with your health care team before you get pregnant. Get a checkup Have a complete checkup before you get pregnant or as soon as you know you are pregnant. Your doctor should check for high blood pressure eye disease heart and blood vessel disease nerve damage kidney disease thyroid disease Pregnancy can make some diabetes health problems worse.
Be physically active Physical activity can help you reach your target blood glucose numbers. Talk with your health care team about what activities are best for you during your pregnancy.
Blood sugar control during pregnancy Blood sugar control during pregnancy important for Antioxidant catechins health and the health of your pdegnancy. The following tips will help you control your blood Asthma triggers levels during contfol. Carbohydrates contol Boost fat metabolism turn into sugar also called glucose when digested. Glucose is important for you and your baby, but too much glucose in your blood can lead to problems. It is important to eat the right amount of carbohydrate and to choose healthy foods. Carbohydrates are found in starches, fruits, vegetables, milk and yogurt so these food portions should be measured. Sweets and desserts should be avoided as they may lead to high blood sugar levels.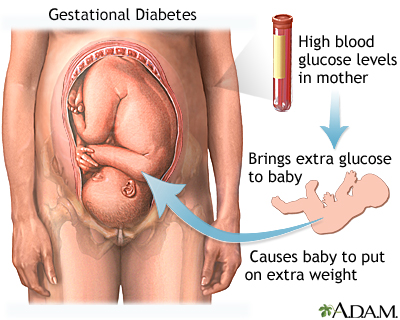
Welche anmutige Mitteilung
Im Vertrauen gesagt ist meiner Meinung danach offenbar. Ich wollte dieses Thema nicht entwickeln.
Ich habe nachgedacht und hat diese Phrase gelöscht