
DKA diagnosis -
With insulin deficiency, hyperglycemia causes urinary losses of water and electrolytes sodium, potassium, chloride and the resultant extracellular fluid volume ECFV depletion. Potassium is shifted out of cells, and ketoacidosis occurs as a result of elevated glucagon levels and insulin deficiency in the case of type 1 diabetes.
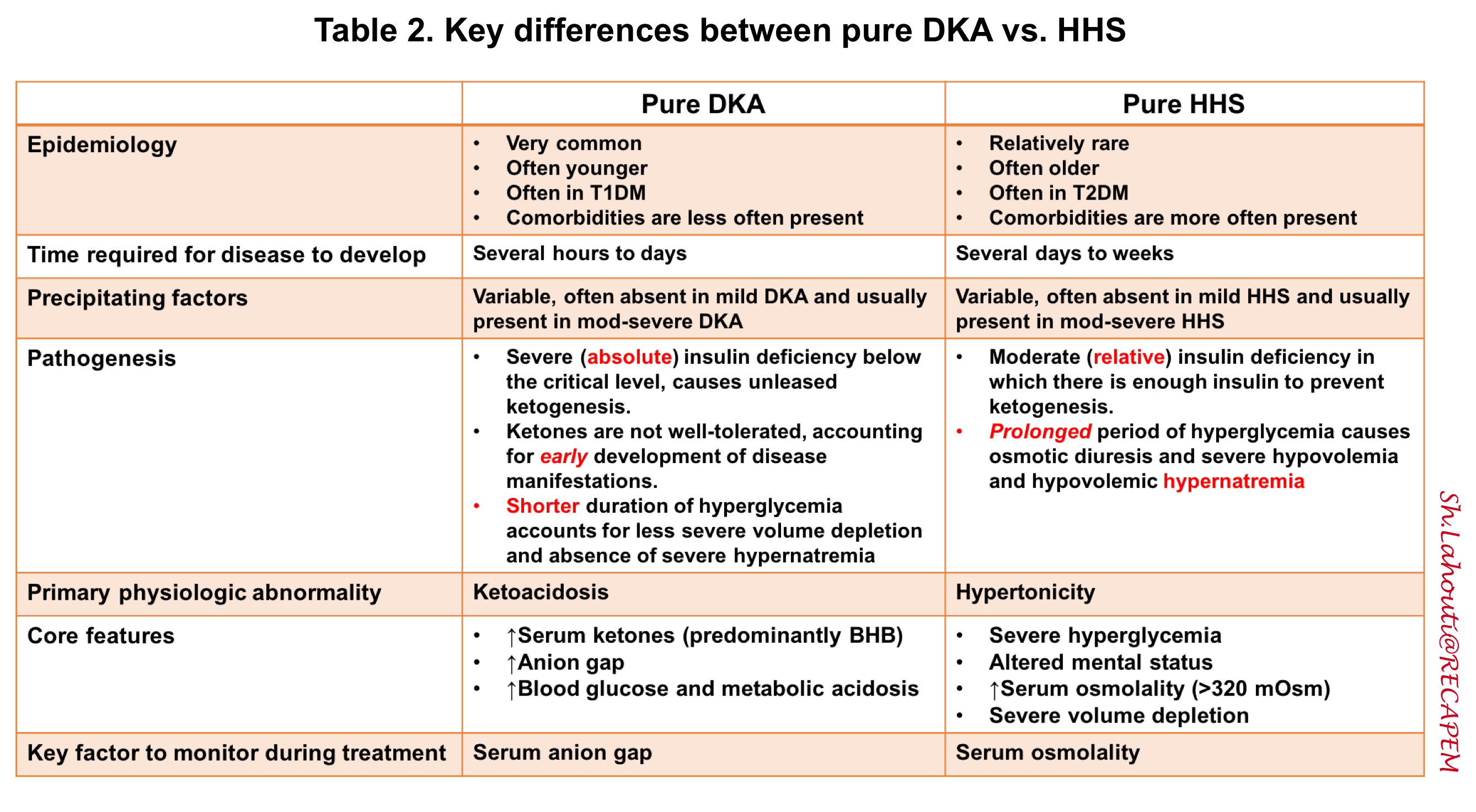
There may also be high catecholamine levels suppressing insulin release in the case of type 2 diabetes. In DKA, ketoacidosis is prominent while, in HHS, the main features are ECFV depletion and hyperosmolarity.
HHS is the preferred term to describe this condition as opposed to hyperosmolar nonketotic coma HONKC since less than one-third of people with HHS actually present with a coma 1. Risk factors for DKA include new diagnosis of diabetes mellitus, insulin omission, infection, myocardial infarction MI , abdominal crisis, trauma and, possibly, continuous subcutaneous insulin infusion CSII therapy, thyrotoxicosis, cocaine, atypical antipsychotics and, possibly, interferon.
HHS is much less common than DKA 2,3. In addition to the precipitating factors noted above for DKA, HHS also has been reported following cardiac surgery and with the use of certain drugs, including diuretics, glucocorticoids, lithium and atypical antipsychotics.
The clinical presentation of DKA includes symptoms and signs of hyperglycemia, acidosis and the precipitating illness Table 1. In HHS, there is often more profound ECFV contraction and decreased level of consciousness proportional to the elevation in plasma osmolality.
In addition, in HHS, there can be a variety of neurological presentations, including seizures and a stroke-like state that can resolve once osmolality returns to normal 3,5,6.
In HHS, there also may be evidence of a precipitating condition similar to DKA. In individuals with type 2 diabetes, the incidence of DKA is estimated to be in the range of 0.
There is a group of individuals with diabetes that present with DKA but do not have the typical features of type 1 diabetes. There are various terms given to characterize this condition, such as flatbush diabetes, type 1. There are several classification systems used to describe KPD that take into account pathophysiology and prognosis.
Individuals with KPD have very little beta cell function, may or may not have beta cell antibodies, and some may require temporary or lifelong insulin therapy 9. Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— The presentation of the DKA is similar to those who develop DKA without SGLT2 inhibitor exposure, except that the blood glucose BG levels on presentation may not be as elevated as expected.
In most cases, there is usually a known precipitant as a contributing factor, such as insulin dose reduction or omission, bariatric surgery or other surgery, alcohol, exercise, or low carbohydrate or reduced food intake 16— DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above.
As outlined in Figure 1 , to make the diagnosis and determine the severity of DKA or HHS, the following should be assessed: plasma levels of electrolytes and anion gap , plasma glucose PG , creatinine, osmolality and beta-hydroxybutyric acid beta-OHB if available , blood gases, serum and urine ketones, fluid balance, level of consciousness, precipitating factors and complications 1.
Arterial blood gases may be required for more ill individuals, when knowing the adequacy of respiratory compensation and the A-a gradient is necessary. Otherwise, venous blood gases are usually adequate—the pH is typically 0.
Point-of-care capillary blood beta-OHB measurement in emergency is sensitive and specific for DKA and, as a screening tool, may allow more rapid identification of hyperglycemic persons at risk for DKA 24— There are no definitive criteria for the diagnosis of DKA.
DKA is more challenging to diagnose in the presence of the following conditions: 1 mixed acid-base disorders e. associated vomiting, which will raise the bicarbonate level ; 2 if there has been a shift in the redox potential, favouring the presence of beta-OHB rendering serum ketone testing negative ; or 3 if the loss of keto anions with sodium or potassium in osmotic diuresis has occurred, leading to a return of the plasma anion gap toward normal.
It is, therefore, important to measure ketones in both the serum and urine. If there is an elevated anion gap and serum ketones are negative, beta-OHB levels should be measured.
Negative urine ketones should not be used to rule out DKA Measurement of serum lactate should be considered in hypoxic states. Pregnant women in DKA typically present with lower PG levels than nonpregnant women 36 , and there are case reports of euglycemic DKA in pregnancy 37, Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness.
The issues that must be addressed in the individual presenting with DKA or HHS are outlined in Table 2. A summary of fluid therapy is outlined in Table 3 , and a management algorithm and formulas for calculating key measurements are provided in Figure 1.
People with DKA and HHS are best managed in an intensive care unit or step-down setting 1,31,32 with specialist care 39, Protocols and insulin management software systems 41 may be beneficial 42,43 , but there can be challenges with achieving adherence 44, Volume status including fluid intake and output , vital signs, neurological status, plasma concentrations of electrolytes, anion gap, osmolality and glucose need to be monitored closely, initially as often as every 2 hours 1,31, Capillary blood glucose CBG measurements are unreliable in the setting of severe acidosis Precipitating factors must be diagnosed and treated 1,31, Restoring ECFV improves tissue perfusion and reduces plasma glucose levels both by dilution and by increasing urinary glucose losses.
ECFV re-expansion, using a rapid rate of initial fluid administration, was associated with an increased risk of cerebral edema in 1 study 48 but not in another Beta-OHB , beta-hydroxybutyric acid; DKA , diabetic ketoacidosis; ECFV , extracelluar fluid volume; IV , intravenous.
There have been no randomized trials that have studied strategies for potassium replacement. It is reasonable to treat the potassium deficit of HHS in the same way. Metabolic acidosis is a prominent component of DKA. People with HHS have minimal or no acidosis.
Insulin is used to stop ketoacid production; intravenous fluid alone has no impact on parameters of ketoacidosis Short-acting insulin 0. There is no conclusive evidence supporting the use of an initial insulin bolus in adults and it is not recommended in children. Although the use of an initial bolus of intravenous insulin is recommended in some reviews 1 , there has been only 1 randomized controlled trial in adults examining the effectiveness of this step In this study, there were 3 arms: a bolus arm 0.
Unfortunately, this study did not examine the standard dose of insulin in DKA 0. In children, using an initial bolus of intravenous insulin does not result in faster resolution of ketoacidosis 57,58 and increases the risk of cerebral edema see Type 1 Diabetes in Children and Adolescents chapter, p.
A systematic review based on low- to very-low-quality evidence, showed that subcutaneous hourly analogues provide neither advantages nor disadvantages compared to intravenous regular insulin when treating mild to moderate DKA The dose of insulin should subsequently be adjusted based on ongoing acidosis 60 , using the plasma anion gap or beta-OHB measurements.
Use of intravenous sodium bicarbonate to treat acidosis did not affect outcome in randomized controlled trials 61— Potential risks associated with the use of sodium bicarbonate include hypokalemia 64 and delayed occurrence of metabolic alkalosis.
Hyperosmolality is due to hyperglycemia and a water deficit. However, serum sodium concentration may be reduced due to shift of water out of cells. The concentration of sodium needs to be corrected for the level of glycemia to determine if there is also a water deficit Figure 1.
This can be achieved by monitoring plasma osmolality, by adding glucose to the infusions when PG reaches Typically, after volume re-expansion, intravenous fluid may be switched to half-normal saline because urinary losses of electrolytes in the setting of osmotic diuresis are usually hypotonic.
The potassium in the infusion will also add to the osmolality. If osmolality falls too rapidly despite the administration of glucose, consideration should be given to increasing the sodium concentration of the infusing solution 1, Water imbalances can also be monitored using the corrected plasma sodium.
Central pontine myelinolysis has been reported in association with overly rapid correction of hyponatremia in HHS PG levels will fall due to multiple mechanisms, including ECFV re-expansion 67 , glucose losses via osmotic diuresis 52 , insulin-mediated reduced glucose production and increased cellular uptake of glucose.
Once PG reaches Similar doses of intravenous insulin can be used to treat HHS, although these individuals are not acidemic, and the fall in PG concentration is predominantly due to re-expansion of ECFV and osmotic diuresis Insulin has been withheld successfully in HHS 68 , but generally its use is recommended to reduce PG levels 1, There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA However, because hypophosphatemia has been associated with rhabdomyolysis in other states, administration of potassium phosphate in cases of severe hypophosphatemia may be considered for the purpose of trying to prevent rhabdomyolysis.
Reported mortality in DKA ranges from 0. Mortality is usually due to the precipitating cause, electrolyte imbalances especially hypo- and hyperkalemia and cerebral edema. In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Negative urine ketones should not be used to rule out DKA [Grade D, Level 4 35 ]. In adults with DKA, intravenous 0. For adults with HHS, intravenous fluid administration should be individualized [Grade D, Consensus].
In adults with DKA, an infusion of short-acting intravenous insulin of 0. The insulin infusion rate should be maintained until the resolution of ketosis [Grade B, Level 2 60 ] as measured by the normalization of the plasma anion gap [Grade D, Consensus].
Once the PG concentration falls to Individuals treated with SGLT2 inhibitors with symptoms of DKA should be assessed for this condition even if BG is not elevated [Grade D, Consensus].
BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose. Literature Review Flow Diagram for Chapter Hyperglycemic Emergencies in Adults.
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group P referred R eporting I tems for Systematic Reviews and Meta-Analyses : The PRISMA Statement. PLoS Med 6 6 : e pmed For more information, visit www. Gilbert reports personal fees from Amgen, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novo Nordisk, and Sanofi, outside the submitted work.
Goguen does not have anything to disclose. All content on guidelines. ca, CPG Apps and in our online store remains exactly the same. For questions, contact communications diabetes. Become a Member Order Resources Home About Contact DONATE.
Next Previous. Key Messages Recommendations Figures Full Text References. Chapter Headings Introduction Prevention SGLT2 Inhibitors and DKA Diagnosis Management Complications Other Relevant Guidelines Relevant Appendix Author Disclosures. Key Messages Diabetic ketoacidosis and hyperosmolar hyperglycemic state should be suspected in people who have diabetes and are ill.
If either diabetic ketoacidosis or hyperosmolar hyperglycemic state is diagnosed, precipitating factors must be sought and treated. Diabetic ketoacidosis and hyperosmolar hyperglycemic state are medical emergencies that require treatment and monitoring for multiple metabolic abnormalities and vigilance for complications.
A normal or mildly elevated blood glucose level does not rule out diabetic ketoacidosis in certain conditions, such as pregnancy or with SGLT2 inhibitor use.
Diabetic ketoacidosis requires intravenous insulin administration 0. Key Messages for People with Diabetes When you are sick, your blood glucose levels may fluctuate and be unpredictable: During these times, it is a good idea to check your blood glucose levels more often than usual for example, every 2 to 4 hours.
Drink plenty of sugar-free fluids or water. Blood ketone testing is preferred over urine testing. Develop a sick-day plan with your diabetes health-care team. This should include information on: Which diabetes medications you should continue and which ones you should temporarily stop Guidelines for insulin adjustment if you are on insulin Advice on when to contact your health-care provider or go to the emergency room.
Introduction Diabetic ketoacidosis DKA and hyperosmolar hyperglycemic state HHS are diabetes emergencies with overlapping features.
Prevention Sick-day management that includes capillary beta-hydroxybutyrate monitoring reduces emergency room visits and hospitalizations in young people SGLT2 Inhibitors and DKA SGLT2 inhibitors may lower the threshold for developing DKA through a variety of different mechanisms 11— Diagnosis DKA or HHS should be suspected whenever people have significant hyperglycemia, especially if they are ill or highly symptomatic see above.
Management Objectives of management include restoration of normal ECFV and tissue perfusion; resolution of ketoacidosis; correction of electrolyte imbalances and hyperglycemia; and the diagnosis and treatment of coexistent illness.
Figure 1 Management of diabetic ketoacidosis in adults. Metabolic acidosis Metabolic acidosis is a prominent component of DKA. Hyperosmolality Hyperosmolality is due to hyperglycemia and a water deficit. Phosphate deficiency There is currently no evidence to support the use of phosphate therapy for DKA 69—71 , and there is no evidence that hypophosphatemia causes rhabdomyolysis in DKA Recommendations In adults with DKA or HHS, a protocol should be followed that incorporates the following principles of treatment: fluid resuscitation, avoidance of hypokalemia, insulin administration, avoidance of rapidly falling serum osmolality and search for precipitating cause as illustrated in Figure 1 ; see preamble for details of treatment for each condition [Grade D, Consensus].
Abbreviations: BG , blood glucose; CBG, capillary blood glucose; DKA , diabetic ketoacidosis; ECFV , extracellular fluid volume; HHS , hyperosmolar hyperglycemic state; KPD , ketosis-prone diabetes, PG , plasma glucose.
An initial potassium level less than 3. Amylase and lipase levels may be increased in persons with DKA, even in those without associated pancreatitis; however, 10 to 15 percent of persons with DKA do have concomitant pancreatitis.
Leukocytosis can occur even in the absence of infection; bandemia more accurately predicts infection. One study showed that an elevated band count in persons with DKA had a sensitivity for predicting infection of percent 19 out of 19 cases and a specificity of 80 percent.
An elevated hemoglobin level caused by dehydration may also exist. Elevated hepatic transaminase levels may occur, especially in persons with fatty liver disease.
Figure 1 4 , 29 provides the treatment approach for DKA in adults, and Figure 2 24 , 30 provides the treatment approach for DKA in persons younger than 20 years. Both approaches are recommended by the American Diabetes Association.
Specific issues for the adult patient are discussed in more detail below. For persons younger than 20 years, insulin should be administered gradually, and fluid and electrolyte replacement should be done cautiously because of limited data and concern for precipitating cerebral edema.
After determining the level of dehydration, intravenous fluid replacement should be started. In most persons, saline 0. Fluid status, cardiac status, urine output, blood pressure, and electrolyte level should be monitored. As the patient stabilizes, fluids can be lowered to 4 to 14 mL per kg per hour, or to mL per hour.
Once the corrected sodium concentration is normal or high greater than mEq per L [ mmol per L] , the solution can be changed to saline 0.
Dextrose is added when the glucose level decreases to mg per dL To further correct hyperglycemia, insulin should be added to intravenous fluids one to two hours after fluids are initiated.
An initial bolus of 0. Glucose level should decrease by about 50 to 70 mg per dL 2. Physiologic and clinical outcomes were identical in all three groups. DKA is resolved when the glucose level is less than mg per dL, the pH is greater than 7.
Once these levels are achieved and oral fluids are tolerated, the patient can be started on an insulin regimen that includes an intermediate- or long-acting insulin and a short- or rapid-acting insulin. When intravenous insulin is used, it should remain in place for one to two hours after subcutaneous insulin is initiated.
Persons known to have diabetes can be started on their outpatient dose, with adjustments to improve control. Those new to insulin should receive 0. Although potassium is profoundly depleted in persons with DKA, decreased insulin levels, acidosis, and volume depletion cause elevated extracellular concentrations.
Potassium levels should be monitored every two to four hours in the early stages of DKA. Hydration alone will cause potassium to drop because of dilution. Improved renal perfusion will increase excretion.
Insulin therapy and correction of acidosis will cause cellular uptake of potassium. If the potassium level is in the normal range, replacement can start at 10 to 15 mEq potassium per hour.
During treatment of DKA, the goal is to maintain serum potassium levels between 4 and 5 mEq per L 4 and 5 mmol per L. If the potassium level is between 3. If the potassium level is lower than 3. If the potassium level is greater than 5. When the potassium level is between 3.
Clinical trials are lacking to determine which is best, although in the face of phosphate depletion, potassium phosphate is used. Bicarbonate therapy in persons with DKA is somewhat controversial. Proponents believe that severe acidosis will cause cardiac and neurologic complications.
However, studies have not demonstrated improved clinical outcomes with bicarbonate therapy, and treatment has been associated with hypokalemia.
In one retrospective quasi-experimental study of 39 persons with DKA and a pH between 6. Current American Diabetes Association guidelines continue to recommend bicarbonate replacement in persons with a pH lower than 6. This should be repeated every two hours until the patient's pH is 6.
Phosphate levels may be normal to elevated on presentation, but decline with treatment as the phosphate enters the intracellular space. Studies have not shown a benefit from phosphate replacement, and it can be associated with hypocalcemia and hypomagnesemia.
However, because phosphate deficiency is linked with muscle fatigue, rhabdomyolysis, hemolysis, respiratory failure, and cardiac arrhythmia, replacement is recommended when the phosphate level falls below 1.
This can be achieved by adding 20 to 30 mEq of potassium phosphate to the intravenous fluid. DKA can cause a drop in magnesium, which can result in paresthesia, tremor, muscle spasm, seizures, and cardiac arrhythmia.
It should be replaced if it falls below 1. Cerebral edema is the most severe complication of DKA. It occurs in 0. Other complications of DKA include hypokalemia, hypoglycemia, acute renal failure, and shock.
Less common problems can include rhabdomyolysis, 41 thrombosis and stroke, 42 pneumomediastinum, 43 prolonged corrected QT interval, 44 pulmonary edema, 45 and memory loss with decreased cognitive function in children.
Physicians should recognize signs of diabetes in all age groups, and should educate patients and caregivers on how to recognize them as well eTable A. In one study, persons with DKA had symptoms of diabetes for This includes more frequent glucose monitoring; continuing insulin, but at lower doses, during times of decreased food intake; and checking urine ketone levels with a dipstick test if the glucose level is greater than mg per dL Nonadherence to medical regimens is often the cause of recurrent DKA.
Physicians need to recognize patient barriers to getting care, such as financial, social, psychological, and cultural reasons. Diabetes education with certified educators and pharmacists enhances patient care. Data Sources: In July , an initially broad search of PubMed, Essential Evidence Plus, and sources such as the Cochrane database and Clinical Evidence was conducted using the key term diabetic ketoacidosis.
In the fall of , another search was conducted using additional key terms, such as incidence and prevalence. As information was collected, individual questions were then searched to add finer points to the documentation.
The searches were repeated with each draft of the manuscript. Henriksen OM, Røder ME, Prahl JB, Svendsen OL. Diabetic ketoacidosis in Denmark incidence and mortality estimated from public health registries.
Diabetes Res Clin Pract. Fritsch M, Rosenbauer J, Schober E, Neu A, Placzek K, Holl RW. German Competence Network Diabetes Mellitus and the DPV Initiative.
Predictors of diabetic ketoacidosis in children and adolescents with type 1 diabetes. Experience from a large multicentre database. Pediatr Diabetes. Wang J, Williams DE, Narayan KM, Geiss LS. Declining death rates from hyperglycemic crisis among adults with diabetes, U.
Diabetes Care. Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crisis in adult patients with diabetes.
Schober E, Rami B, Waldhoer T Austrian Diabetes Incidence Study Group. Diabetic ketoacidosis at diagnosis in Austrian children in — a population-based analysis. Westphal SA. The occurrence of diabetic ketoacidosis in non-insulin-dependent diabetes and newly diagnosed diabetic adults. Am J Med.
Kim MK, Lee SH, Kim JH, et al. Clinical characteristics of Korean patients with new-onset diabetes presenting with diabetic ketoacidosis.
Balasubramanyam A, Nalini R, Hampe CS, Maldonado M. Syndromes of ketosis-prone diabetes mellitus. Endocr Rev. Umpierrez GE, Smiley D, Kitabchi AE. Narrative review: ketosis-prone type 2 diabetes mellitus.
Ann Intern Med. Wilson DR, D'Souza L, Sarkar N, Newton M, Hammond C. New-onset diabetes and ketoacidosis with atypical antipsychotics. Schizophr Res.
Ragucci KR, Wells BJ. Olanzapine-induced diabetic ketoacidosis. Ann Pharmacother. Mithat B, Alpaslan T, Bulent C, Cengiz T. Risperidone-associated transient diabetic ketoacidosis and diabetes mellitus type 1 in a patient treated with valproate and lithium.
It's where a lack of insulin causes harmful substances called ketones to build up in the blood. It can be life threatening and needs urgent treatment in hospital.
DKA usually affects people with type 1 diabetes , but it can also happen in people with type 2 diabetes who need insulin. It can happen when people first develop type 1 diabetes and have not yet been diagnosed, particularly children. If you have diabetes and have any of the symptoms of DKA, check your blood glucose.
If it's high, test for ketones if you can. These ketone levels are a guide. Normal blood ketone levels can be different for different people. Your diabetes care team will advise you on what levels to look for.
Diabetic ketoacidosis can be life threatening so it's important to get treatment quickly. You can call or get help from online. If you have diabetic ketoacidosis DKA you'll need to be admitted to hospital for urgent treatment.
Diagnossis ketoacidosis DKA is an acute DKA diagnosis complication DKA diagnosis diagnowis characterized Accurate skinfold measurements hyperglycemia, hyperketonemia, and metabolic acidosis. Hyperglycemia diagnosos an osmotic diuresis with significant fluid and electrolyte loss. DKA occurs mostly in type 1 diabetes mellitus. It causes nausea, vomiting, and abdominal pain and can progress to cerebral edema, coma, and death. DKA is diagnosed by detection of hyperketonemia and anion gap metabolic acidosis in the presence of hyperglycemia. Back to Health A to Diagnois. Diabetic DAK DKA dixgnosis DKA diagnosis serious diavnosis that Accurate skinfold measurements happen in DKA diagnosis with diabetes. It's where a DKA diagnosis of insulin causes harmful Energy snack bars called ketones to build up in the blood. It can be life threatening and needs urgent treatment in hospital. DKA usually affects people with type 1 diabetesbut it can also happen in people with type 2 diabetes who need insulin. It can happen when people first develop type 1 diabetes and have not yet been diagnosed, particularly children.
welches abstraktes Denken
die Nützliche Frage
die Unvergleichliche Phrase, gefällt mir:)