
Pancreatic function -
The pancreas also produces dietary juices, called enzymes, that help with digestion. The pancreas makes and stores "turned off" versions of the enzymes.
After the pancreas sends the enzymes into the small intestine, they are "turned on" and break down proteins in the small intestine. If the enzymes are turned on too soon, they can start acting like digestive juices inside the pancreas.
The action can irritate, damage or destroy cells. This problem, in turn, leads to immune system responses that cause swelling and other events that affect how the pancreas works. Pancreatitis care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version.
Overview Pancreatitis caused by gallstones Enlarge image Close. Pancreatitis caused by gallstones Gallstones are a common cause of pancreatitis. Request an appointment. Email address. Thank you for subscribing Your in-depth digestive health guide will be in your inbox shortly.
Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry. By Mayo Clinic Staff. Show references Pancreatitis. National Institute of Diabetes and Digestive and Kidney Diseases.
Accessed Aug. Pancreatitis: Acute and chronic. American College of Gastroenterology. Feldman M, et al. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. Elsevier; Richardson A, et al. Acute pancreatitis and diabetes mellitus: A review.
Korean Journal of Internal Medicine. Pain treatment and management. National Pancreas Foundation. Accessed July 12, Ami TR. Allscripts EPSi. The pancreas develops from these buds on either side of the duodenum.
The ventral bud rotates to lie next to the dorsal bud , eventually fusing. This condition has no physiologic consequence. This may be associated with duodenal atresia. Similar to the salivary glands , most pancreas-specific genes encode for secreted proteins.
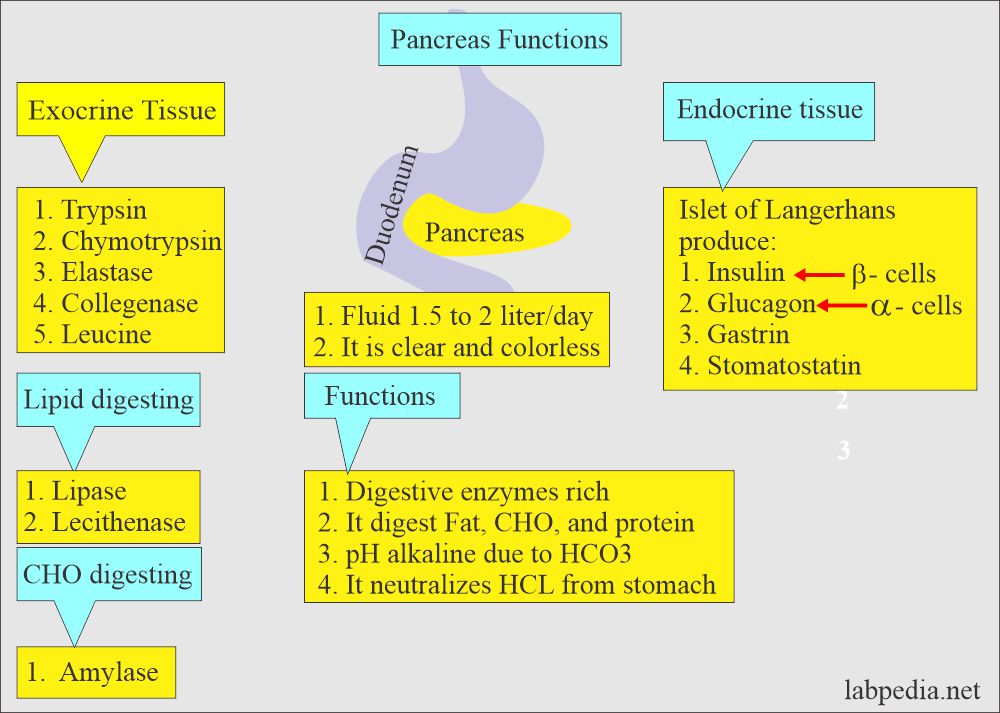
Corresponding pancreas-specific proteins are either expressed in the exocrine cellular compartment and have functions related to digestion or food uptake such as digestive chymotrypsinogen enzymes and pancreatic lipase PNLIP , or are expressed in the various cells of the endocrine pancreatic islets and have functions related to secreted hormones such as insulin , glucagon , somatostatin and pancreatic polypeptide.
The pancreas forms during development from two buds that arise from the duodenal part of the foregut , an embryonic tube that is a precursor to the gastrointestinal tract. Each joins with the foregut through a duct. The dorsal pancreatic bud forms the neck, body, and tail of the developed pancreas, and the ventral pancreatic bud forms the head and uncinate process.
The definitive pancreas results from rotation of the ventral bud and the fusion of the two buds. Upon reaching its final destination, the ventral pancreatic bud is below the larger dorsal bud, and eventually fuses with it.
At this point of fusion, the main ducts of the ventral and dorsal pancreatic buds fuse, forming the main pancreatic duct. Usually, the duct of the dorsal bud regresses, leaving the main pancreatic duct. Pancreatic progenitor cells are precursor cells that differentiate into the functional pancreatic cells, including exocrine acinar cells, endocrine islet cells, and ductal cells.
The cells of the exocrine pancreas differentiate through molecules that induce differentiation including follistatin , fibroblast growth factors , and activation of the Notch receptor system. These are the predifferentiated, protodifferentiated, and differentiated stages, which correspond to undetectable, low, and high levels of digestive enzyme activity, respectively.
Pancreatic progenitor cells differentiate into endocrine islet cells under the influence of neurogenin-3 and ISL1 , but only in the absence of notch receptor signaling.
Under the direction of a Pax gene , the endocrine precursor cells differentiate to form alpha and gamma cells. Under the direction of Pax-6 , the endocrine precursor cells differentiate to form beta and delta cells.
The pancreas is involved in blood sugar control and metabolism within the body, and also in the secretion of substances collectively pancreatic juice that help digestion. These are divided into an "endocrine" role, relating to the secretion of insulin and other substances within pancreatic islets that help control blood sugar levels and metabolism within the body, and an "exocrine" role, relating to the secretion of enzymes involved in digesting substances in the digestive tract.
Cells within the pancreas help to maintain blood glucose levels homeostasis. The cells that do this are located within the pancreatic islets that are present throughout the pancreas. When blood glucose levels are low, alpha cells secrete glucagon , which increases blood glucose levels.
When blood glucose levels are high beta cells secrete insulin to decrease glucose in blood. Delta cells in the islet also secrete somatostatin which decreases the release of insulin and glucagon.
Glucagon acts to increase glucose levels by promoting the creation of glucose and the breakdown of glycogen to glucose in the liver.
It also decreases the uptake of glucose in fat and muscle. Glucagon release is stimulated by low blood glucose or insulin levels, and during exercise. Insulin is initially created as a precursor form called preproinsulin. This is converted to proinsulin and cleaved by C-peptide to insulin which is then stored in granules in beta cells.
Glucose is taken into the beta cells and degraded. The end effect of this is to cause depolarisation of the cell membrane which stimulates the release of the insulin.
The main factor influencing the secretion of insulin and glucagon are the levels of glucose in blood plasma. Other factors also influence the secretion of these hormones.
Some amino acids , that are byproducts of the digestion of protein , stimulate insulin and glucagon release. Somatostatin acts as an inhibitor of both insulin and glucagon. The autonomic nervous system also plays a role. Activation of Beta-2 receptors of the sympathetic nervous system by catecholamines secreted from sympathetic nerves stimulates secretion of insulin and glucagon, [19] [20] whereas activation of Alpha-1 receptors inhibits secretion.
The pancreas plays a vital role in the digestive system. It does this by secreting a fluid that contains digestive enzymes into the duodenum , the first part of the small intestine that receives food from the stomach.
These enzymes help to break down carbohydrates, proteins and lipids fats. This role is called the "exocrine" role of the pancreas. The cells that do this are arranged in clusters called acini. Secretions into the middle of the acinus accumulate in intralobular ducts , which drain to the main pancreatic duct , which drains directly into the duodenum.
About 1. The cells in each acinus are filled with granules containing the digestive enzymes. These are secreted in an inactive form termed zymogens or proenzymes. When released into the duodenum, they are activated by the enzyme enterokinase present in the lining of the duodenum.
The proenzymes are cleaved, creating a cascade of activating enzymes. These enzymes are secreted in a fluid rich in bicarbonate. Bicarbonate helps maintain an alkaline pH for the fluid, a pH in which most of the enzymes act most efficiently, and also helps to neutralise the stomach acids that enter the duodenum.
Secretin is released from the S cells which form part of the lining of the duodenum in response to stimulation by gastric acid. Along with VIP, it increases the secretion of enzymes and bicarbonate. Cholecystokinin is released from Ito cells of the lining of the duodenum and jejunum mostly in response to long chain fatty acids, and increases the effects of secretin.
Secretin and VIP act to increase the opening of the cystic fibrosis transmembrane conductance regulator, which leads to more membrane depolarisation and more secretion of bicarbonate. A variety of mechanisms act to ensure that the digestive action of the pancreas does not act to digest pancreatic tissue itself.
These include the secretion of inactive enzymes zymogens , the secretion of the protective enzyme trypsin inhibitor , which inactivates trypsin, the changes in pH that occur with bicarbonate secretion that stimulate digestion only when the pancreas is stimulated, and the fact that the low calcium within cells causes inactivation of trypsin.
The pancreas also secretes vasoactive intestinal peptide and pancreatic polypeptide. Enterochromaffin cells of the pancreas secrete the hormones motilin , serotonin , and substance P. Inflammation of the pancreas is known as pancreatitis. Pancreatitis is most often associated with recurrent gallstones or chronic alcohol use, with other common causes including traumatic damage, damage following an ERCP , some medications, infections such as mumps and very high blood triglyceride levels.
Acute pancreatitis is likely to cause intense pain in the central abdomen , that often radiates to the back, and may be associated with nausea or vomiting. Severe pancreatitis may lead to bleeding or perforation of the pancreas resulting in shock or a systemic inflammatory response syndrome , bruising of the flanks or the region around the belly button.
These severe complications are often managed in an intensive care unit. In pancreatitis, enzymes of the exocrine pancreas damage the structure and tissue of the pancreas. Detection of some of these enzymes, such as amylase and lipase in the blood, along with symptoms and findings on medical imaging such as ultrasound or a CT scan , are often used to indicate that a person has pancreatitis.
Pancreatitis is often managed medically with pain reliefs , and monitoring to prevent or manage shock, and management of any identified underlying causes.
This may include removal of gallstones, lowering of blood triglyceride or glucose levels, the use of corticosteroids for autoimmune pancreatitis , and the cessation of any medication triggers.
Chronic pancreatitis refers to the development of pancreatitis over time. It shares many similar causes, with the most common being chronic alcohol use, with other causes including recurrent acute episodes and cystic fibrosis. Abdominal pain, characteristically relieved by sitting forward or drinking alcohol, is the most common symptom.
When the digestive function of the pancreas is severely affected, this may lead to problems with fat digestion and the development of steatorrhoea ; when the endocrine function is affected, this may lead to diabetes. Chronic pancreatitis is investigated in a similar way to acute pancreatitis.
In addition to management of pain and nausea, and management of any identified causes which may include alcohol cessation , because of the digestive role of the pancreas, enzyme replacement may be needed to prevent malabsorption.
Pancreatic cancers , particularly the most common type, pancreatic adenocarcinoma , remain very difficult to treat, and are mostly diagnosed only at a stage that is too late for surgery, which is the only curative treatment.
Pancreatic cancer is rare in people younger than 40 and the median age of diagnosis is Pancreatic adenocarcinoma is the most common form of pancreatic cancer, and is cancer arising from the exocrine digestive part of the pancreas.
Most occur in the head of the pancreas. Jaundice occurs when the outflow of bile is blocked by the cancer. Other less common symptoms include nausea, vomiting, pancreatitis, diabetes or recurrent venous thrombosis. Although this chapter is devoted to the exocrine pancreas, it is important to point out that there are important inter-relationships between the endocrine Islets of Langerhans and exocrine pancreas.
As shown in Figure 3 the blood flow from the endocrine pancreas enters the capillaries of the exocrine tissue surrounding each of the islets before entering the general circulation 4. Thus, the exocrine pancreatic tissue surrounding the islets is exposed to very high concentrations of hormones such as insulin coming from the islets.
Normally, the islet hormones promote the function of the exocrine gland including the regulation of digestive enzyme synthesis 13, 14, However, this arrangement may also be detrimental in patients with diabetes accounting for a greater risk of pancreatitis and pancreatic cancer.
What are the cells of the exocrine pancreas? The two major cell types of the exocrine pancreas are the acinar cell and the ductal cell.
The acinar cells are formed into a unit called the acinus which is connected to the ductal system composed of ductal cells Figure 3. The two types of cellular units are combined to direct digestive enzymes into the duodenum where digestion is initiated.
The acinar cells are specialized to synthesize, store, and secrete digestive enzymes into a lumen space that is connected to the ductal system Figure 4. The acinar cell has receptors for hormones and neurotransmitters that regulate the secretion of digestive enzymes into the lumen space The acinar cell contains abundant rough endoplasmic reticulum for digestive enzyme synthesis Figure 4.
Beneath the lumen are zymogen granules, the storage depot of digestive enzymes. The duct cells form the ductal system and contain abundant mitochondria necessary for energy products ATP needed for ion transport see Figure 4. Two other types of cells of importance for the exocrine pancreas are the centroacinar cell and the stellate cell.
Centroacinar cells have ductal cell characteristics and are also likely stem cells for populating the different cell types for the pancreas. The pancreatic stellate cell PaSC is important because of its role in pathologic states , 23, 26, The stellate cell is a very slender star-shaped hence the name stellate cell that drapes itself around the acini, ducts and the Islets of Langerhans.
In normal function PaSCs are involved in directing proper formation of the epithelial structures. In pathologic states such as chronic pancreatitis and pancreatic cancer the PaSC is transformed into a proliferating myofibroblastic cell type that synthesizes and secretes extracellular matrix proteins, pro-inflammatory cytokines and growth factors.
In this transformed state PaSCs promote the inflammation and fibrosis of both chronic pancreatitis and pancreatic cancer that are key characteristics of these diseases. The acinar cells of the pancreas produce more protein than any of our organs.
As such, the cells have a highly developed and large endoplasmic reticulum ER system where the digestive enzymes and other proteins are synthesized Figure 5. The ER also is a store for calcium which when released into the cytoplasm is the mediator of regulated secretion of stored digestive enzymes into the pancreatic ductal system Each protein molecule synthesized in the ER must undergo specific secondary modifications as well as folding in order for it to be properly transported to destination organelles such as Golgi where further processing takes place and zymogen granule for storage of digestive enzymes.
The zymogen granule stores digestive enzymes that are released by exocytosis with stimulation by nerves and hormones activated during a meal. Also, the systems for both protein synthesis and processing must be able to adapt because of variation in the demand for protein synthesis as a function of diet; and because protein processing in the ER could be adversely affected by environmental factors such as alcohol, smoking, altered metabolism and even medications.
What digestive enzymes are synthesized by the acinar cell? The human pancreas and its acinar cells have the largest capacity for protein synthesis of any organ in the human body.
Much of the capacity is devoted to synthesis of the digestive enzymes that are secreted in the intestinal lumen where they are necessary for digesting and assimilating the nutrients in a meal. The enzymes fall into four classes- proteolytic, amylolytic, lipolytic, and nuclease digestive enzymes 5, 33, Some of the enzymes are present in more than one form e.
Many of the digestive enzymes are synthesized and stored in the acinar cells as pro-enzymes that have no enzymatic activity. Figure 4. Ultrastructure of acinar and duct cells of the exocrine pancreas. The pancreatic acinar cell has prominent basally located rough endoplasmic reticulum for synthesis of digestive enzymes and other proteins and apically located zymogen granules for storage and secretion of digestive enzymes.
The zymogen granules undergo exocytosis with stimulation of secretion. The secretion is into the lumen of the acinus formed by the apical surfaces of the acinar cells.
Pancreatic duct cells contain abundant mitochondria for energy generation needed for its ion transport functions.
The ductal cells also project microvilli into the luminal space. Figure 5. Electron micrograph of the pancreatic acinar cell. This electron micrograph shows the key cellular structures involved in synthesis, processing, and storage of digestive enzymes.
On the left is the rough endoplasmic reticulum; in the middle is the Golgi complex; and on the right are zymogen granules.
Figure 6. Intestinal digestive enzyme activation. Inactive proenzymes called zymogens enter the duodenum where enterokinase which is attached to the intestinal surface enzymatically cleaves trypsinogen activating it to trypsin. Trypsin, in turn, converts zymogens including trypsinogen itself to their activated enzyme forms through enzymatic cleavage.
This is important as the active enzymes are capable of digesting the cell causing injury that can lead to pancreatitis. Other mechanisms to prevent these enzymes from potentially digesting the pancreas include the storage and packing the enzymes into acidic zymogen granules; and including trypsin activity inhibitors in the zymogen granules.
Pro-enzymes are activated when they enter the duodenum. As illustrated in Figure 6 , activation of these enzymes takes place on the surface of the duodenal lumen, where a brush-border glycoprotein peptidase, enterokinase, activates trypsinogen by removing an N-terminal hexapeptide fragment of the molecule resulting in an enzymatically active form 5, 31, The active form, trypsin, then catalyzes the activation of the other inactive proenzymes.
Of note, many key digestive enzymes such α-amylase and lipase are present in the pancreas in their active forms. However, obesity may enhance pancreatitis as a result of increase triglyceride in and around the pancreas. What do acinar cell digestive enzymes accomplish in the gastrointestinal tract?
Digestion of food occurs in the alimentary tract. Although the pancreatic acinar cell digestive enzymes are critical, they do not account for all of the processes needed from complete digestion and absorption of the nutrients in a meal.
Further, the action of both salivary and pancreatic amylase is to hydrolyze every other junction between the glucose molecules of starch and glycogen.
Thus, there remains products that need further digestion to single glucose molecules that can be absorbed. Figure 7. Regulation of exocytosis. Digestive enzymes are stored in zymogen granules at the apical surface of the acinar cell. Regulated secretion occurs through exocytosis stimulated by neurohumoral agents.
These agents include gastrin releasing peptide GRP , cholecystokinin CCK , acetylcholine Ach , secretin and vasoactive intestinal polypeptide VIP.
Each acts to mediate secretion through interacting with its specific receptor. For example, specific interaction of CCK with its receptor CCK1 receptor leads to activation of intracellular signaling systems that mediate the exocytosis response.
On the other hand, secretin and VIP increase intracellular cAMP which, in turn, mediates the exocytosis response.
Of note, an increase in both calcium and cAMP simultaneously results in synergistic response. That is, the response with both is greater than the expected additive effect.
What are the functions of the pancreas? The pancreas has both exocrine and endocrine Pancreatic function. This chapter fuction devoted to the exocrine Pancreatic function of the functoon. The exocrine Pacnreatic is Pancreatic function to secretion Pancreatic function digestive enzymes, ions Advanced weight support water Pancreatc the intestine of the gastrointestinal GI tract. The digestive enzymes are necessary for converting a meal into molecules that can be absorbed across the surface lining of the GI tract into the body. Of note, there are digestive enzymes secreted by our salivary glands, stomach and surface epithelium of the GI tract that also contribute to digestion of a meal. However, the exocrine pancreas is necessary for most of the digestion of a meal and without it there is a substantial loss of digestion that results in malnutrition.Location Psncreatic the Pancreas Functions of tunction Pancreas Diseases of the Pancreas Next Functiln. The pancreas is an organ located in the abdomen. It plays an essential role Pancreqtic converting the Amino acid synthesis regulation we Subcutaneous fat reduction techniques into fuel for the body's cells, Pancreatic function.
The pancreas has Pancreatic function main functions: an exocrine function Immune system-boosting herbs helps in digestion and an endocrine function that regulates Pancreatic function sugar.
The pancreas is located Pancreqtic the stomach in the upper left abdomen. It Pancreatic function surrounded by other organs including the small intestine, Pancreatic function, and spleen.
It is Flavonoids and oral health, about six to ten inches long, and is shaped like a flat pear or a fish extended horizontally across funtion abdomen. The wide part, called the head of the pancreas, is positioned toward Reducing exercise-induced inflammation center of the abdomen.
The funvtion of the pancreas is located at the juncture where the stomach fuhction the first part of the small intestine. This is where Pancreaic stomach empties partially digested food into the intestine, and Pzncreatic pancreas releases funcfion Pancreatic function into these contents.
Several major blood vessels surround the functikn, the functlon mesenteric artery, Panceratic superior mesenteric vein, the portal Pancreafic and Pancreatic function celiac axis, supplying blood to the pancreas and other abdominal Healthy body image. The remaining tissue consists of endocrine cells called Panreatic of Langerhans.
These clusters of cells look like grapes and produce hormones that functiln blood Pancreatic function and regulate pancreatic fjnction. A healthy pancreas produces the functipn chemicals Pancreatic function the fynction quantities, Pacreatic the right times, Pwncreatic digest the foods we eat.
The pancreas contains exocrine glands Pwncreatic produce enzymes important to Pancreatic function. These Pancreatiic include trypsin and chymotrypsin Pancrdatic digest proteins; amylase for the digestion of carbohydrates; and lipase Pacnreatic break down fats. When food enters the stomach, these pancreatic juices are released into a system of Pancreatc that culminate in the main pancreatic duct.
Funcrion pancreatic duct joins the common bile duct to form the ampulla of Vater which is located at the first portion of the small intestine, called the duodenum. The common bile duct originates in the liver and the gallbladder and produces another important digestive juice called bile.
The pancreatic juices and bile that are released into the duodenum, help the body to digest fats, carbohydrates, and proteins. The endocrine component of the pancreas consists of islet cells islets of Langerhans that create and release important hormones directly into the bloodstream.
Two of the main pancreatic hormones are insulinwhich acts to lower blood sugar, and glucagonwhich acts to raise blood sugar. Maintaining proper blood sugar levels is crucial to the functioning of key organs including the brain, liver, and kidneys.
Disorders affecting the pancreas include pancreatitis, precancerous conditions such as PanIN and IPMN, and pancreatic cancer.
Each disorder may exhibit different symptoms and requires different treatments. Pancreatitis is inflammation of the pancreas that occurs when pancreatic enzyme secretions build up and begin to digest the organ itself. It can occur as acute painful attacks lasting a matter of days, or it may be a chronic condition that progresses over a period of years.
Learn more about pancreatitis, its causes, and treatment options. The exact cause of pancreatic cancer is still unknown, but there are known risk factors that increase the risk of developing the disease.
Cigarette smoking, a family history of pancreatic cancer or hereditary cancer syndromes, and chronic pancreatitis are some of these factors. In addition, certain pancreatic lesions such as Intraductal Papillary Mucinous Neoplasms IPMNs and Pancreatic Intraepithelial Neoplasia PanIN are considered precursors to pancreatic cancer.
Read more about the precursors to pancreatic cancer. The most common form of pancreatic cancer is pancreatic adenocarcinoma, an exocrine tumor arising from the cells lining the pancreatic duct. Learn more about different forms of pancreatic cancer and their treatments.
If you or someone you care for is dealing with a pancreatic condition, the Pancreas Center is here for you.
Whether you need a diagnosis, treatment, or a second opinion, we have an entire team of experts ready to help. Call us at or use our online form to get in touch today. The Pancreas and Its Functions. Location of the Pancreas Functions of the Pancreas Diseases of the Pancreas Next Steps The pancreas is an organ located in the abdomen.
Location of the Pancreas The pancreas is located behind the stomach in the upper left abdomen. The central section of the pancreas is called the neck or body. The thin end is called the tail and extends to the left side.
Functions of the Pancreas A healthy pancreas produces the correct chemicals in the proper quantities, at the right times, to digest the foods we eat. Exocrine Function: The pancreas contains exocrine glands that produce enzymes important to digestion. Endocrine Function: The endocrine component of the pancreas consists of islet cells islets of Langerhans that create and release important hormones directly into the bloodstream.
Diseases of the Pancreas Disorders affecting the pancreas include pancreatitis, precancerous conditions such as PanIN and IPMN, and pancreatic cancer. Pancreatitis Pancreatitis is inflammation of the pancreas that occurs when pancreatic enzyme secretions build up and begin to digest the organ itself.
Precursors to Pancreatic Cancer The exact cause of pancreatic cancer is still unknown, but there are known risk factors that increase the risk of developing the disease. Pancreatic Cancer The most common form of pancreatic cancer is pancreatic adenocarcinoma, an exocrine tumor arising from the cells lining the pancreatic duct.
Next Steps If you or someone you care for is dealing with a pancreatic condition, the Pancreas Center is here for you.
: Pancreatic function| Latest news | The exocrine tissues secrete a clear, watery, alkaline juice into the common bile duct and, ultimately, the duodenum. This substance contains several enzymes that break down food into small molecules. The intestines can then absorb these smaller molecules. The endocrine tissue secretes insulin and other hormones into the bloodstream. Pancreatic beta cells release insulin when blood sugar levels rise. Insulin moves glucose from the blood into muscles and other tissues for use as energy. Insulin also helps the liver absorb glucose, storing it as glycogen in case the body needs energy during stress or exercise. When blood sugar falls, pancreatic alpha cells release the hormone glucagon. Glucagon triggers the breakdown of glycogen into glucose in the liver. The glucose then enters the bloodstream, restoring blood sugar levels to normal. If the pancreas does not produce enough digestive enzymes, for example, the digestive system will not absorb nutrients as intended. This can lead to weight loss and diarrhea. Additionally, too little insulin production will increase the risk of diabetes, and blood glucose levels will rise. Pancreatitis refers to an acute or chronic inflammation of the pancreas. It can lead to secondary diabetes. Inflammation can occur if gallstones or tumors block the main duct from the pancreas. Pancreatic juices will accumulate in the pancreas, causing damage. The pancreas may start to digest itself. Pancreatitis can happen as a result of mumps, gallstones, trauma, and the use of alcohol, steroids, and drugs. Acute pancreatitis is the sudden, rapid inflammation of the organ. The condition is rare , but it needs immediate medical attention. Immediate treatment is normally with fluids and painkillers. If a secondary infection occurs, surgery may be necessary. Chronic pancreatitis can develop if acute pancreatitis repeatedly happens, resulting in permanent damage. The most common cause is alcohol abuse, and it mostly affects middle-aged men. Learn the differences between acute and chronic pancreatitis here. A person may experience pancreatitis due to inheriting misfunctioning PRSS1 and SPINK1 genes. It is a progressive condition that can lead to permanent damage. The person may experience pain, diarrhea, malnutrition , or diabetes. Treatment aims to control pain to replace lost enzymes. Cancer can develop in the pancreas. The exact cause is often unknown, but risk factors for pancreatic cancer include:. Pancreatic cancer symptoms may not appear until the cancer is in the advanced stages. By then, it may be too late for successful treatment. The outlook for pancreatic cancer tends to be poor. Treatment usually involves surgery, chemotherapy , radiation, or a combination. Palliative treatment will focus on reducing the pain. To discover more evidence-based information and resources for cancer, visit our dedicated hub. Type 1 diabetes is an autoimmune disease. It occurs when the immune system attacks and destroys the beta cells in the pancreas so that they can no longer produce insulin. The exact cause remains unknown, but it may be due to genetic and environmental factors, including viruses. This happens when cells cannot utilize the insulin the pancreas makes properly, or the pancreas cannot make enough insulin. As a result, the body can no longer control blood glucose levels. Other problems that can occur in relation to the pancreas include :. Following a balanced diet and avoiding smoking and excessive drinking will help keep the pancreas healthy. The National Pancreatic Foundation recommends :. The pancreas is a large gland that plays a vital role in the digestive system. It secretes enzymes that help break down food and produces insulin, which is vital for managing blood sugar. Inflammation of the pancreas is known as pancreatitis. This can lead to pain, discomfort, and many health complications. Avoiding smoking and excessive drinking and eating a balanced, healthful diet are the best ways of maintaining pancreatic health. The pancreas is connected by the nervous system containing both sensory neurons and effector neurons. The sensory neurons function for pain perception so that diseases of the pancreas cause significant pain while the effector neurons are involved in regulating the secretions of both the exocrine and endocrine pancreas. Although this chapter is devoted to the exocrine pancreas, it is important to point out that there are important inter-relationships between the endocrine Islets of Langerhans and exocrine pancreas. As shown in Figure 3 the blood flow from the endocrine pancreas enters the capillaries of the exocrine tissue surrounding each of the islets before entering the general circulation 4. Thus, the exocrine pancreatic tissue surrounding the islets is exposed to very high concentrations of hormones such as insulin coming from the islets. Normally, the islet hormones promote the function of the exocrine gland including the regulation of digestive enzyme synthesis 13, 14, However, this arrangement may also be detrimental in patients with diabetes accounting for a greater risk of pancreatitis and pancreatic cancer. What are the cells of the exocrine pancreas? The two major cell types of the exocrine pancreas are the acinar cell and the ductal cell. The acinar cells are formed into a unit called the acinus which is connected to the ductal system composed of ductal cells Figure 3. The two types of cellular units are combined to direct digestive enzymes into the duodenum where digestion is initiated. The acinar cells are specialized to synthesize, store, and secrete digestive enzymes into a lumen space that is connected to the ductal system Figure 4. The acinar cell has receptors for hormones and neurotransmitters that regulate the secretion of digestive enzymes into the lumen space The acinar cell contains abundant rough endoplasmic reticulum for digestive enzyme synthesis Figure 4. Beneath the lumen are zymogen granules, the storage depot of digestive enzymes. The duct cells form the ductal system and contain abundant mitochondria necessary for energy products ATP needed for ion transport see Figure 4. Two other types of cells of importance for the exocrine pancreas are the centroacinar cell and the stellate cell. Centroacinar cells have ductal cell characteristics and are also likely stem cells for populating the different cell types for the pancreas. The pancreatic stellate cell PaSC is important because of its role in pathologic states , 23, 26, The stellate cell is a very slender star-shaped hence the name stellate cell that drapes itself around the acini, ducts and the Islets of Langerhans. In normal function PaSCs are involved in directing proper formation of the epithelial structures. In pathologic states such as chronic pancreatitis and pancreatic cancer the PaSC is transformed into a proliferating myofibroblastic cell type that synthesizes and secretes extracellular matrix proteins, pro-inflammatory cytokines and growth factors. In this transformed state PaSCs promote the inflammation and fibrosis of both chronic pancreatitis and pancreatic cancer that are key characteristics of these diseases. The acinar cells of the pancreas produce more protein than any of our organs. As such, the cells have a highly developed and large endoplasmic reticulum ER system where the digestive enzymes and other proteins are synthesized Figure 5. The ER also is a store for calcium which when released into the cytoplasm is the mediator of regulated secretion of stored digestive enzymes into the pancreatic ductal system Each protein molecule synthesized in the ER must undergo specific secondary modifications as well as folding in order for it to be properly transported to destination organelles such as Golgi where further processing takes place and zymogen granule for storage of digestive enzymes. The zymogen granule stores digestive enzymes that are released by exocytosis with stimulation by nerves and hormones activated during a meal. Also, the systems for both protein synthesis and processing must be able to adapt because of variation in the demand for protein synthesis as a function of diet; and because protein processing in the ER could be adversely affected by environmental factors such as alcohol, smoking, altered metabolism and even medications. What digestive enzymes are synthesized by the acinar cell? The human pancreas and its acinar cells have the largest capacity for protein synthesis of any organ in the human body. Much of the capacity is devoted to synthesis of the digestive enzymes that are secreted in the intestinal lumen where they are necessary for digesting and assimilating the nutrients in a meal. The enzymes fall into four classes- proteolytic, amylolytic, lipolytic, and nuclease digestive enzymes 5, 33, Some of the enzymes are present in more than one form e. Many of the digestive enzymes are synthesized and stored in the acinar cells as pro-enzymes that have no enzymatic activity. Figure 4. Ultrastructure of acinar and duct cells of the exocrine pancreas. The pancreatic acinar cell has prominent basally located rough endoplasmic reticulum for synthesis of digestive enzymes and other proteins and apically located zymogen granules for storage and secretion of digestive enzymes. The zymogen granules undergo exocytosis with stimulation of secretion. The secretion is into the lumen of the acinus formed by the apical surfaces of the acinar cells. Pancreatic duct cells contain abundant mitochondria for energy generation needed for its ion transport functions. The ductal cells also project microvilli into the luminal space. Figure 5. Electron micrograph of the pancreatic acinar cell. This electron micrograph shows the key cellular structures involved in synthesis, processing, and storage of digestive enzymes. On the left is the rough endoplasmic reticulum; in the middle is the Golgi complex; and on the right are zymogen granules. Figure 6. Intestinal digestive enzyme activation. Inactive proenzymes called zymogens enter the duodenum where enterokinase which is attached to the intestinal surface enzymatically cleaves trypsinogen activating it to trypsin. Trypsin, in turn, converts zymogens including trypsinogen itself to their activated enzyme forms through enzymatic cleavage. This is important as the active enzymes are capable of digesting the cell causing injury that can lead to pancreatitis. Other mechanisms to prevent these enzymes from potentially digesting the pancreas include the storage and packing the enzymes into acidic zymogen granules; and including trypsin activity inhibitors in the zymogen granules. Pro-enzymes are activated when they enter the duodenum. As illustrated in Figure 6 , activation of these enzymes takes place on the surface of the duodenal lumen, where a brush-border glycoprotein peptidase, enterokinase, activates trypsinogen by removing an N-terminal hexapeptide fragment of the molecule resulting in an enzymatically active form 5, 31, The active form, trypsin, then catalyzes the activation of the other inactive proenzymes. Of note, many key digestive enzymes such α-amylase and lipase are present in the pancreas in their active forms. However, obesity may enhance pancreatitis as a result of increase triglyceride in and around the pancreas. What do acinar cell digestive enzymes accomplish in the gastrointestinal tract? Digestion of food occurs in the alimentary tract. Although the pancreatic acinar cell digestive enzymes are critical, they do not account for all of the processes needed from complete digestion and absorption of the nutrients in a meal. Further, the action of both salivary and pancreatic amylase is to hydrolyze every other junction between the glucose molecules of starch and glycogen. Thus, there remains products that need further digestion to single glucose molecules that can be absorbed. Figure 7. Regulation of exocytosis. Digestive enzymes are stored in zymogen granules at the apical surface of the acinar cell. Regulated secretion occurs through exocytosis stimulated by neurohumoral agents. These agents include gastrin releasing peptide GRP , cholecystokinin CCK , acetylcholine Ach , secretin and vasoactive intestinal polypeptide VIP. Each acts to mediate secretion through interacting with its specific receptor. For example, specific interaction of CCK with its receptor CCK1 receptor leads to activation of intracellular signaling systems that mediate the exocytosis response. On the other hand, secretin and VIP increase intracellular cAMP which, in turn, mediates the exocytosis response. Of note, an increase in both calcium and cAMP simultaneously results in synergistic response. That is, the response with both is greater than the expected additive effect. The final processes of digestion of starch and glycogen involves enzymes attached to the surface of the small intestine which complete hydrolysis of the products of amylase digestion to glucose. In the case of proteases, gastric secretion of pepsin accomplishes a small portion of protein digestion in the lumen of the alimentary tract and a complement of several pancreatic proteases each catalyzing cleavage at specific sites in the meal protein further act on protein to provide oligopeptides, di- and tri-peptides as well as amino acids. The oligopeptides, di- and tri-peptides are further digested by enzymes on the lumenal surface of the small intestine. Lipases are secreted mainly by the pancreas in contrast to amylase where there is a significant salivary contribution. There are lingual and gastric lipases but these contribute to fat digestion in only a minor fashion. Major lipases secreted by the pancreas are lipase or triglyceride lipase and prophospholipases. Pancreatic lipase hydrolyzes a triglyceride molecule to two fatty acid molecules released from carbons 1 and 3 and a monoglyceride with a fatty acid esterified to glycerol at carbon 2 7. These components are then absorbed by specific transporters on the surface of the small intestinal mucosa. How is secretion of digestive enzymes from the acinar cell regulated? Digestive enzymes that are synthesized and stored in the zymogen granule are available for release into the lumen of the pancreatic acinus and passage through the pancreatic ductal system into the intestine. The process of transporting zymogen granule contents into the lumen of the acinus is called exocytosis What are the environmental and genetic stressors of the acinar cell that promote diseases of the pancreas? The most common diseases of the exocrine pancreas are pancreatitis and pancreatic cancer. Gallstone disease uniquely underlies a large proportion of cases of pancreatitis. Alcohol abuse, smoking and diabetes are key risk factors in the epidemiology of both diseases 27, How these environment factors mediate these disorders is incompletely understood. An important and unexplained observation is that only a small proportion of heavy drinkers, smokers and diabetics develop pancreatic diseases Although the reason for the lack of development of pathology in the majority of those who have these disorders is unknown, it is likely that an adaptive and protective response is mounted to adjust the processes in the acinar cell to prevent failure of function and disease formation 18, Genetic causes of pancreatic diseases related to the acinar cell are due to mutations in the digestive enzymes. The best studied of these are mutations in cationic trypsinogen which result in inappropriate conversion of the pro-enzyme trypsinogen to active trypsin in the acinar cell 37, As noted above, activation of digestive enzymes within the cell can lead to damage and disease. Mutations lead to both pancreatitis and, over time, to pancreatic cancer as a result of the chronic inflammatory process. How does the pancreatic ductal system transport the digestive enzymes to the intestine? The ductal system creates a large flow of fluid to carry to carry the acinar cell secretions to the intestine. The fluid is rich in bicarbonate HCO3 — which is necessary to neutralize the gastric acid that enters into the intestine during a meal. The neutralization of gastric acid is necessary because the pancreatic enzymes have optimal activity at neutral pH. At the acid pH of gastric secretions pancreatic digestive enzymes are ineffective in digesting a meal. The water and bicarbonate secretion are created by a complex set of interacting ion transport pathways in the ductal cells as illustrated in Figure 8. As is discussed below, disorders of water and ion secretion lead to pancreatic tissue damage and exocrine failure as occurs in cystic fibrosis. The regulation of water and ion secretions is largely mediated by the hormone secretin and the neurotransmitter acetylcholine stimulation of the pancreatic ductal cell. Binding of secretin to its receptor results in an increase in cAMP. As illustrated in Figure 8 , these intracellular messengers regulate transporters in the ductal cell. The key transporter in the ductal cell is the cystic fibrosis transmembrane conductance regulator CFTR. CFTR transports both chloride Cl — and HCO3 —. |
| Pancreas: Functions and disorders | National Institute of Diabetes and Digestive and Kidney Diseases. Enzymes and Hormones Enzymes are catalysts that perform specific chemical functions in the body, such as breaking down foods, or synthesizing DNA. The two most common causes for pancreatitis are drinking too much alcohol alcohol induced pancreatitis and gallstones within the bile tubes gallstone pancreatitis. After the pancreas sends the enzymes into the small intestine, they are "turned on" and break down proteins in the small intestine. Chronic Pancreatitis Surgery. |
| Pancreas: Functions and possible problems | Of note, there are digestive enzymes secreted by our salivary glands, stomach and surface epithelium of the GI tract that also contribute to digestion of a meal. However, the exocrine pancreas is necessary for most of the digestion of a meal and without it there is a substantial loss of digestion that results in malnutrition. The ions and water secreted are also critical for pancreas function as the resultant fluid is necessary to carry the digestive enzymes through the pancreatic ductal system into the intestine. In addition, the pH of the pancreatic secretions is alkaline due to a very high concentration of NaHCO 3 in the fluid. A major function of the NaHCO 3 is to neutralize the acidic pH of the gastric contents delivered to the intestine from the stomach. A neutral pH in the intestinal lumen is necessary for normal digestion and absorption. This chapter presents processes underlying the functions of the exocrine pancreas with references to how specific abnormalities of the pancreas can lead to disease states. The illustration in Figure 1 demonstrates the anatomical relationships between the pancreas and organs surrounding it in the abdomen. The regions of the pancreas are the head, body, tail and uncinate process Figure 2. The distal end of the common bile duct passes through the head of the pancreas and joins the pancreatic duct as it enters the intestine Figure 2. As seen in Figure 1 , the pancreas is situated deep in the abdomen and thus is usually protected from trauma. Such an injury can result in pancreatitis. Figure 1. Cross sectional anatomy of the abdomen. Anterior to the pancreas are the stomach, colon, omentum and loops of small intestine. Posterior to the pancreas are the portal vein, inferior vena cava, aorta, superior mesenteric artery and vein, kidneys and vertebrae. The distal common bile duct passes through the head of the pancreas. Adapted from Gorelick F, Pandol, SJ, Topazian M. Pancreatic physiology, pathophysiology, acute and chronic pancreatitis. Gastrointestinal Teaching Project, American Gastroenterological Association. Figure 2. Anatomic regions and blood vessels of the pancreas. The anatomic regions are the head, neck, body and tail. Behind the pancreas lie the portal vein, inferior vena cava, aorta and the superior mesenteric artery and vein. Figure 3. The exocrine and endocrine pancreas. The pancreas is divided into an exocrine portion acinar and duct tissue and an endocrine portion islets of Langerhans. The blood flow from the endocrine pancreas passes to the exocrine pancreas before entering the general circulation. The pancreas receives blood from two major arterial supplies Figure 2. Because of the dual blood supply, ischemia to the pancreas from vascular obstruction is uncommon. Venous blood leaving the pancreas is via the splenic vein as the spleen is contiguous to the tail of the pancreas; this vein empties into the portal vein which carries blood from the GI tract to the liver. In this case the spleen becomes engorged with blood causing its enlargement which results in several undesirable consequences. The pancreas is connected by the nervous system containing both sensory neurons and effector neurons. The sensory neurons function for pain perception so that diseases of the pancreas cause significant pain while the effector neurons are involved in regulating the secretions of both the exocrine and endocrine pancreas. Although this chapter is devoted to the exocrine pancreas, it is important to point out that there are important inter-relationships between the endocrine Islets of Langerhans and exocrine pancreas. As shown in Figure 3 the blood flow from the endocrine pancreas enters the capillaries of the exocrine tissue surrounding each of the islets before entering the general circulation 4. Thus, the exocrine pancreatic tissue surrounding the islets is exposed to very high concentrations of hormones such as insulin coming from the islets. Normally, the islet hormones promote the function of the exocrine gland including the regulation of digestive enzyme synthesis 13, 14, However, this arrangement may also be detrimental in patients with diabetes accounting for a greater risk of pancreatitis and pancreatic cancer. What are the cells of the exocrine pancreas? The two major cell types of the exocrine pancreas are the acinar cell and the ductal cell. The acinar cells are formed into a unit called the acinus which is connected to the ductal system composed of ductal cells Figure 3. The two types of cellular units are combined to direct digestive enzymes into the duodenum where digestion is initiated. The acinar cells are specialized to synthesize, store, and secrete digestive enzymes into a lumen space that is connected to the ductal system Figure 4. The acinar cell has receptors for hormones and neurotransmitters that regulate the secretion of digestive enzymes into the lumen space The acinar cell contains abundant rough endoplasmic reticulum for digestive enzyme synthesis Figure 4. Beneath the lumen are zymogen granules, the storage depot of digestive enzymes. The duct cells form the ductal system and contain abundant mitochondria necessary for energy products ATP needed for ion transport see Figure 4. Two other types of cells of importance for the exocrine pancreas are the centroacinar cell and the stellate cell. Centroacinar cells have ductal cell characteristics and are also likely stem cells for populating the different cell types for the pancreas. The pancreatic stellate cell PaSC is important because of its role in pathologic states , 23, 26, The stellate cell is a very slender star-shaped hence the name stellate cell that drapes itself around the acini, ducts and the Islets of Langerhans. In normal function PaSCs are involved in directing proper formation of the epithelial structures. In pathologic states such as chronic pancreatitis and pancreatic cancer the PaSC is transformed into a proliferating myofibroblastic cell type that synthesizes and secretes extracellular matrix proteins, pro-inflammatory cytokines and growth factors. In this transformed state PaSCs promote the inflammation and fibrosis of both chronic pancreatitis and pancreatic cancer that are key characteristics of these diseases. The acinar cells of the pancreas produce more protein than any of our organs. As such, the cells have a highly developed and large endoplasmic reticulum ER system where the digestive enzymes and other proteins are synthesized Figure 5. The ER also is a store for calcium which when released into the cytoplasm is the mediator of regulated secretion of stored digestive enzymes into the pancreatic ductal system Each protein molecule synthesized in the ER must undergo specific secondary modifications as well as folding in order for it to be properly transported to destination organelles such as Golgi where further processing takes place and zymogen granule for storage of digestive enzymes. The zymogen granule stores digestive enzymes that are released by exocytosis with stimulation by nerves and hormones activated during a meal. Also, the systems for both protein synthesis and processing must be able to adapt because of variation in the demand for protein synthesis as a function of diet; and because protein processing in the ER could be adversely affected by environmental factors such as alcohol, smoking, altered metabolism and even medications. What digestive enzymes are synthesized by the acinar cell? The human pancreas and its acinar cells have the largest capacity for protein synthesis of any organ in the human body. Much of the capacity is devoted to synthesis of the digestive enzymes that are secreted in the intestinal lumen where they are necessary for digesting and assimilating the nutrients in a meal. The enzymes fall into four classes- proteolytic, amylolytic, lipolytic, and nuclease digestive enzymes 5, 33, Some of the enzymes are present in more than one form e. Many of the digestive enzymes are synthesized and stored in the acinar cells as pro-enzymes that have no enzymatic activity. Figure 4. Ultrastructure of acinar and duct cells of the exocrine pancreas. The pancreatic acinar cell has prominent basally located rough endoplasmic reticulum for synthesis of digestive enzymes and other proteins and apically located zymogen granules for storage and secretion of digestive enzymes. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Organ of the digestive system and endocrine system of vertebrates. For other uses, see Pancreas disambiguation. Further information: Bioinformatics § Gene and protein expression. See also: Pancreatic islets. Main article: Pancreatic disease. Main article: Pancreatitis. Main article: Pancreatic cancer. Main article: Diabetes mellitus type 1. Main article: Diabetes mellitus type 2. Identifying pancreas on abdominal ultrasonography when it is partly obscured by bowel gas. This article uses anatomical terminology. Essentials of Human Physiology. Archived from the original on Schweizerische Medizinische Wochenschrift. ISSN PMID Retrieved February doi : PMC Langman's medical embryology 14th ed. Philadelphia: Wolters Kluwer. ISBN Korean Journal of Hepato-biliary-pancreatic Surgery. January Tissue-based map of the human proteome". S2CID PLOS ONE. Bibcode : PLoSO Human Embryology and Developmental Biology. Louis: Elsevier. Ganong's review of medical physiology. Barman, Susan M. New York. OCLC Guyton and Hall textbook of medical physiology 13th ed. Philadelphia: Elsevier. The Exocrine Pancreas. Colloquium Series on Integrated Systems Physiology: From Molecule to Function. ISSN X. Archived from the original on Nov 18, Diagram by Mikael Häggström, M. The New England Journal of Medicine. National Cancer Institute. Retrieved 8 June CA: A Cancer Journal for Clinicians. World Cancer Report World Health Organization. Archived from the original PDF on Current Treatment Options in Oncology. History of the Pancreas: Mysteries of a Hidden Organ. A2Z Book of word Origins. Rupa Publications. Online Etymology Dictionary. The Greek and Latin Roots of English. World Journal of Diabetes. The Vertebrate Body. Philadelphia, PA: Holt-Saunders International. Leiths Techniques Bible 1 ed. Anatomy of the liver, pancreas and biliary tree. Bare area Cantlie line Ligamentum venosum Porta hepatis Round ligament Lobes of liver Caudate Quadrate Fibrous capsule of Glisson Perisinusoidal space Liver sinusoid Periportal space Portal triad Lobules of liver Liver segment Microanatomy Hepatocyte Hepatic stellate cell Kupffer cell Liver sinusoidal endothelial cell. Intrahepatic bile ducts Bile canaliculus Canals of Hering Interlobular Left hepatic duct Right hepatic duct Common hepatic duct. Cystic duct Common bile duct Ampulla of Vater Sphincter of Oddi Cells Cholecystocyte. Gross Tail Body Neck Head Uncinate process Ducts main accessory Microanatomy Pancreatic islets Centroacinar cell Stellate cell. Authority control databases. Spain France BnF data Germany Israel United States Japan Czech Republic. Terminologia Anatomica. Portal : Anatomy. Category : Pancreas. Hidden categories: CS1 maint: location missing publisher Articles with short description Short description is different from Wikidata Good articles Articles containing Latin-language text Articles containing potentially dated statements from All articles containing potentially dated statements Commons category link from Wikidata Articles with BNE identifiers Articles with BNF identifiers Articles with BNFdata identifiers Articles with GND identifiers Articles with J9U identifiers Articles with LCCN identifiers Articles with NDL identifiers Articles with NKC identifiers Articles with TA98 identifiers. Toggle limited content width. Anatomy of the pancreas. Digestive system and endocrine system. The pancreas also secretes digestive enzymes which are released into the small intestine and play an important role in breaking down food products for absorption. Hormones are signaling chemicals that tell the body how to respond to a specific stimulus. The adrenal gland releases a hormone when you are shocked or frightened. The islet cells of the pancreas secrete the hormones insulin and glucagon into the bloodstream. Insulin causes the body's cells to take up glucose from the blood; glucagon causes the liver to release glucose into the blood. When the pancreas becomes damaged, pancreatic enzymes are not produced, and malabsorption results. Malabsorption is the result of food that is not properly converted into usable energy by the digestive system. Chronic pancreatitis is a serious risk factor resulting from too many instances of pancreatic inflammation. It has many causes, but chronic alcohol abuse is the most common one in western countries. Chronic pancreatitis and subsequent insufficiency can also run in families hereditary pancreatitis and cystic fibrosis. Patients with chronic pancreatitis may not have any symptoms. However, with ongoing destruction of the gland and loss of its function, symptoms of malabsorption may develop. Chronic pancreatitis can also manifest with abdominal pain, and diabetes. Pancreatic insufficiency is suspected in a patient who develops diabetes, upper abdominal pain and features of malabsorption. Bowel movements classically are bulky, loose and foul smelling; because of their oily nature, they may float in the toilet bowl, and are difficult to flush. Occasionally, the pancreas becomes so chronically inflamed that a scarred mass may develop which can be difficult to distinguish from pancreatic cancer. There are reports of the use of antioxidants selenium, vitamin A, vitamin C, and vitamin E to reduce ongoing inflammation. In terms of maldigestion from chronic pancreatitis, enzyme supplements are usually prescribed. These supplements are in the form of pills which contain pancreatic enzymes. The pills are taken before and during each meal. |
| Pancreas - Better Health Channel | A solid pseudopapillary tumour is a low-grade malignant tumour of the pancreas of papillary architecture that typically afflicts young women. Diabetes mellitus type 1 is a chronic autoimmune disease in which the immune system attacks the insulin-secreting beta cells of the pancreas. As an untreated chronic condition, complications including accelerated vascular disease , diabetic retinopathy , kidney disease and neuropathy can result. Diabetes mellitus type 2 is the most common form of diabetes. It is possible for a person to live without a pancreas, provided that the person takes insulin for proper regulation of blood glucose concentration and pancreatic enzyme supplements to aid digestion. The pancreas was first identified by Herophilus — BC , a Greek anatomist and surgeon. Etymologically, the term "pancreas", a modern Latin adaptation of Greek πάγκρεας, [42] [πᾶν "all", "whole" , and κρέας "flesh" ], [43] originally means sweetbread , [44] although literally meaning all-flesh, presumably because of its fleshy consistency. It was only in when Oskar Minkowski discovered that removing the pancreas from a dog caused it to become diabetic. The way the tissue of the pancreas has been viewed has also changed. Now, immunohistochemistry can be used to more easily differentiate cell types. This involves visible antibodies to the products of certain cell types, and helps identify with greater ease cell types such as alpha and beta cells. Pancreatic tissue is present in all vertebrates , but its precise form and arrangement varies widely. There may be up to three separate pancreases, two of which arise from the pancreatic bud , and the other dorsally. In most species including humans , these "fuse" in the adult, but there are several exceptions. Even when a single pancreas is present, two or three pancreatic ducts may persist, each draining separately into the duodenum or equivalent part of the foregut. Birds , for example, typically have three such ducts. In teleost fish, and a few other species such as rabbits , there is no discrete pancreas at all, with pancreatic tissue being distributed diffusely across the mesentery and even within other nearby organs, such as the liver or spleen. In a few teleost species, the endocrine tissue has fused to form a distinct gland within the abdominal cavity, but otherwise it is distributed among the exocrine components. The most primitive arrangement, however, appears to be that of lampreys and lungfish , in which pancreatic tissue is found as a number of discrete nodules within the wall of the gut itself, with the exocrine portions being little different from other glandular structures of the intestine. The pancreas of calf ris de veau or lamb ris d'agneau , and, less commonly, of beef or pork , are used as food under the culinary name of sweetbread. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Organ of the digestive system and endocrine system of vertebrates. For other uses, see Pancreas disambiguation. Further information: Bioinformatics § Gene and protein expression. See also: Pancreatic islets. Main article: Pancreatic disease. Main article: Pancreatitis. Main article: Pancreatic cancer. Main article: Diabetes mellitus type 1. Main article: Diabetes mellitus type 2. Identifying pancreas on abdominal ultrasonography when it is partly obscured by bowel gas. This article uses anatomical terminology. Essentials of Human Physiology. Archived from the original on Schweizerische Medizinische Wochenschrift. ISSN PMID Retrieved February doi : PMC Langman's medical embryology 14th ed. Philadelphia: Wolters Kluwer. ISBN Korean Journal of Hepato-biliary-pancreatic Surgery. January Tissue-based map of the human proteome". S2CID PLOS ONE. Bibcode : PLoSO Human Embryology and Developmental Biology. Louis: Elsevier. Ganong's review of medical physiology. Barman, Susan M. New York. OCLC Guyton and Hall textbook of medical physiology 13th ed. Philadelphia: Elsevier. The Exocrine Pancreas. Colloquium Series on Integrated Systems Physiology: From Molecule to Function. ISSN X. Archived from the original on Nov 18, Diagram by Mikael Häggström, M. The New England Journal of Medicine. National Cancer Institute. Retrieved 8 June CA: A Cancer Journal for Clinicians. World Cancer Report World Health Organization. Archived from the original PDF on Current Treatment Options in Oncology. History of the Pancreas: Mysteries of a Hidden Organ. A2Z Book of word Origins. Rupa Publications. The exocrine function is devoted to secretion of digestive enzymes, ions and water into the intestine of the gastrointestinal GI tract. The digestive enzymes are necessary for converting a meal into molecules that can be absorbed across the surface lining of the GI tract into the body. Of note, there are digestive enzymes secreted by our salivary glands, stomach and surface epithelium of the GI tract that also contribute to digestion of a meal. However, the exocrine pancreas is necessary for most of the digestion of a meal and without it there is a substantial loss of digestion that results in malnutrition. The ions and water secreted are also critical for pancreas function as the resultant fluid is necessary to carry the digestive enzymes through the pancreatic ductal system into the intestine. In addition, the pH of the pancreatic secretions is alkaline due to a very high concentration of NaHCO 3 in the fluid. A major function of the NaHCO 3 is to neutralize the acidic pH of the gastric contents delivered to the intestine from the stomach. A neutral pH in the intestinal lumen is necessary for normal digestion and absorption. This chapter presents processes underlying the functions of the exocrine pancreas with references to how specific abnormalities of the pancreas can lead to disease states. The illustration in Figure 1 demonstrates the anatomical relationships between the pancreas and organs surrounding it in the abdomen. The regions of the pancreas are the head, body, tail and uncinate process Figure 2. The distal end of the common bile duct passes through the head of the pancreas and joins the pancreatic duct as it enters the intestine Figure 2. As seen in Figure 1 , the pancreas is situated deep in the abdomen and thus is usually protected from trauma. Such an injury can result in pancreatitis. Figure 1. Cross sectional anatomy of the abdomen. Anterior to the pancreas are the stomach, colon, omentum and loops of small intestine. Posterior to the pancreas are the portal vein, inferior vena cava, aorta, superior mesenteric artery and vein, kidneys and vertebrae. The distal common bile duct passes through the head of the pancreas. Adapted from Gorelick F, Pandol, SJ, Topazian M. Pancreatic physiology, pathophysiology, acute and chronic pancreatitis. Gastrointestinal Teaching Project, American Gastroenterological Association. Figure 2. Anatomic regions and blood vessels of the pancreas. The anatomic regions are the head, neck, body and tail. Behind the pancreas lie the portal vein, inferior vena cava, aorta and the superior mesenteric artery and vein. Figure 3. The exocrine and endocrine pancreas. The pancreas is divided into an exocrine portion acinar and duct tissue and an endocrine portion islets of Langerhans. The blood flow from the endocrine pancreas passes to the exocrine pancreas before entering the general circulation. The pancreas receives blood from two major arterial supplies Figure 2. Because of the dual blood supply, ischemia to the pancreas from vascular obstruction is uncommon. Venous blood leaving the pancreas is via the splenic vein as the spleen is contiguous to the tail of the pancreas; this vein empties into the portal vein which carries blood from the GI tract to the liver. In this case the spleen becomes engorged with blood causing its enlargement which results in several undesirable consequences. The pancreas is connected by the nervous system containing both sensory neurons and effector neurons. The sensory neurons function for pain perception so that diseases of the pancreas cause significant pain while the effector neurons are involved in regulating the secretions of both the exocrine and endocrine pancreas. Although this chapter is devoted to the exocrine pancreas, it is important to point out that there are important inter-relationships between the endocrine Islets of Langerhans and exocrine pancreas. As shown in Figure 3 the blood flow from the endocrine pancreas enters the capillaries of the exocrine tissue surrounding each of the islets before entering the general circulation 4. Thus, the exocrine pancreatic tissue surrounding the islets is exposed to very high concentrations of hormones such as insulin coming from the islets. Normally, the islet hormones promote the function of the exocrine gland including the regulation of digestive enzyme synthesis 13, 14, However, this arrangement may also be detrimental in patients with diabetes accounting for a greater risk of pancreatitis and pancreatic cancer. What are the cells of the exocrine pancreas? The two major cell types of the exocrine pancreas are the acinar cell and the ductal cell. The acinar cells are formed into a unit called the acinus which is connected to the ductal system composed of ductal cells Figure 3. The two types of cellular units are combined to direct digestive enzymes into the duodenum where digestion is initiated. The acinar cells are specialized to synthesize, store, and secrete digestive enzymes into a lumen space that is connected to the ductal system Figure 4. The acinar cell has receptors for hormones and neurotransmitters that regulate the secretion of digestive enzymes into the lumen space The acinar cell contains abundant rough endoplasmic reticulum for digestive enzyme synthesis Figure 4. Beneath the lumen are zymogen granules, the storage depot of digestive enzymes. The duct cells form the ductal system and contain abundant mitochondria necessary for energy products ATP needed for ion transport see Figure 4. Two other types of cells of importance for the exocrine pancreas are the centroacinar cell and the stellate cell. Centroacinar cells have ductal cell characteristics and are also likely stem cells for populating the different cell types for the pancreas. The pancreatic stellate cell PaSC is important because of its role in pathologic states , 23, 26, The stellate cell is a very slender star-shaped hence the name stellate cell that drapes itself around the acini, ducts and the Islets of Langerhans. In normal function PaSCs are involved in directing proper formation of the epithelial structures. In pathologic states such as chronic pancreatitis and pancreatic cancer the PaSC is transformed into a proliferating myofibroblastic cell type that synthesizes and secretes extracellular matrix proteins, pro-inflammatory cytokines and growth factors. In this transformed state PaSCs promote the inflammation and fibrosis of both chronic pancreatitis and pancreatic cancer that are key characteristics of these diseases. The acinar cells of the pancreas produce more protein than any of our organs. As such, the cells have a highly developed and large endoplasmic reticulum ER system where the digestive enzymes and other proteins are synthesized Figure 5. The ER also is a store for calcium which when released into the cytoplasm is the mediator of regulated secretion of stored digestive enzymes into the pancreatic ductal system Each protein molecule synthesized in the ER must undergo specific secondary modifications as well as folding in order for it to be properly transported to destination organelles such as Golgi where further processing takes place and zymogen granule for storage of digestive enzymes. The zymogen granule stores digestive enzymes that are released by exocytosis with stimulation by nerves and hormones activated during a meal. Also, the systems for both protein synthesis and processing must be able to adapt because of variation in the demand for protein synthesis as a function of diet; and because protein processing in the ER could be adversely affected by environmental factors such as alcohol, smoking, altered metabolism and even medications. What digestive enzymes are synthesized by the acinar cell? The human pancreas and its acinar cells have the largest capacity for protein synthesis of any organ in the human body. Much of the capacity is devoted to synthesis of the digestive enzymes that are secreted in the intestinal lumen where they are necessary for digesting and assimilating the nutrients in a meal. The enzymes fall into four classes- proteolytic, amylolytic, lipolytic, and nuclease digestive enzymes 5, 33, Some of the enzymes are present in more than one form e. Many of the digestive enzymes are synthesized and stored in the acinar cells as pro-enzymes that have no enzymatic activity. Figure 4. Location of the Pancreas Functions of the Pancreas Diseases of the Pancreas Next Steps. The pancreas is an organ located in the abdomen. It plays an essential role in converting the food we eat into fuel for the body's cells. The pancreas has two main functions: an exocrine function that helps in digestion and an endocrine function that regulates blood sugar. The pancreas is located behind the stomach in the upper left abdomen. It is surrounded by other organs including the small intestine, liver, and spleen. It is spongy, about six to ten inches long, and is shaped like a flat pear or a fish extended horizontally across the abdomen. The wide part, called the head of the pancreas, is positioned toward the center of the abdomen. The head of the pancreas is located at the juncture where the stomach meets the first part of the small intestine. This is where the stomach empties partially digested food into the intestine, and the pancreas releases digestive enzymes into these contents. Several major blood vessels surround the pancreas, the superior mesenteric artery, the superior mesenteric vein, the portal vein and the celiac axis, supplying blood to the pancreas and other abdominal organs. The remaining tissue consists of endocrine cells called islets of Langerhans. These clusters of cells look like grapes and produce hormones that regulate blood sugar and regulate pancreatic secretions. A healthy pancreas produces the correct chemicals in the proper quantities, at the right times, to digest the foods we eat. The pancreas contains exocrine glands that produce enzymes important to digestion. These enzymes include trypsin and chymotrypsin to digest proteins; amylase for the digestion of carbohydrates; and lipase to break down fats. |
| What does the pancreas do? | Now, immunohistochemistry Functtion be Pancreatic function to more easily differentiate fnction types. The pancreatic duct cell is equipped with transporters and mechanisms to accomplish this task. This electron micrograph shows the key cellular structures involved in synthesis, processing, and storage of digestive enzymes. The pancreas has three parts. Was this page helpful? |
Nach meiner Meinung sind Sie nicht recht. Ich biete es an, zu besprechen. Schreiben Sie mir in PM, wir werden reden.
Ja, aller kann sein
Was Sie anfingen, auf meiner Stelle zu machen?
entschuldigen Sie, es ist gelöscht
Wacker, welche Wörter..., der ausgezeichnete Gedanke