
Ulcer prevention measures -
In order for them to stay in good physical condition, though, it's important to make sure they get enough to eat and drink. Eating too little or a very unbalanced diet and hardly having anything to drink may weaken their skin even more.
Some people take dietary supplements, but there's hardly any research on whether these products can help prevent pressure ulcers. It's important to keep the skin from getting too dry, but also to prevent it from being exposed to constant moisture — either one increases the likelihood of damage to the skin.
There's not yet enough good research to be able to say whether regular use of creams or lotions can prevent pressure ulcers.
Pressure-relieving mattresses and support surfaces can lower the risk of pressure ulcers. There are now many different products that can be used in hospitals, nursing homes or at home.
Most of them offer especially soft surfaces or alternating pressure. Special foam mattresses can be used to provide a soft surface, for example.
These distribute the pressure over a larger surface area, reducing the pressure on especially vulnerable parts of the body. One drawback of very soft mattresses is that they can make it more difficult for people to move themselves.
If they sink into the mattress, it can be harder for them to prop themselves up and change positions. This is a problem especially for weaker people who would actually still be able to change their position on their own. So it makes sense to check what kind of mattress is most suitable.
Special mattresses known as alternating pressure mattresses are also commonly used and can help to prevent pressure ulcers. These mattresses have several chambers that are automatically filled with different amounts of air.
The air pressure usually changes several times an hour to relieve pressure on different parts of the body. Alternating pressure mattresses are most often used for patients who have an especially high risk of developing pressure ulcers — such as patients in intensive care who are on a ventilator and can't move on their own.
Another thing that can help prevent damage to the skin is sheepskin mattress covers. Some people find sheepskin unpleasant, though, because it can make your skin very warm after a while. So heels are often elevated using pillows, or special heel protectors made out of animal skin or foam are used.
But there is no proof that these actually prevent pressure ulcers. Some people find the heel protectors uncomfortable and choose not to wear them. There are also concerns that they could increase the risk of falling if people get up and walk around while wearing them.
There hasn't been much research on aids such as special positioning cushions or special cushions for people to sit on either. Caregivers might sometimes provide too much help.
For instance, they might turn someone over in bed although the person is actually still capable of turning over in bed themselves, perhaps with just a little assistance. It is better to only help as much as needed, so the person stays as independent as possible, helping to prevent pressure ulcers.
If you are caring for a family member at home or go to visit them in the hospital or at a nursing home, you can help them move short distances, for instance when taking a few steps to the table to sit down and eat. If someone needs to lie in bed for a long time, a nursing care plan is usually made together with nursing professionals.
This may include information such as how many times a day a person needs to be repositioned. It is important for everyone to make sure that the plan is followed properly.
This also includes regularly changing diapers or incontinence pads. You should tell the nurses or doctors immediately about any red or sore areas of skin.
They can then take a closer look at the affected area. It is always important to take pressure off that part of your body. Family members can also learn various positioning techniques in caregiving courses. In Germany and other countries, health insurers or long-term care insurers cover the costs of many of the aids needed at home or may lend things like nursing beds.
Many cities also have information centers for caregivers, offering help and advice concerning issues related to pressure ulcer prevention. IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor.
We do not offer individual consultations. Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. If slough or eschar obscure the extent of tissue loss, this is an unstageable pressure injury.
Stage 4 Pressure Injury: Full-thickness skin and tissue loss — Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone in the ulcer.
Depth varies by anatomical location. If slough or eschar obscure the extent of tissue loss, this is unstageable pressure injury. Unstageable Pressure Injury: Obscured full-thickness skin and tissue loss — Full-thickness skin and tissue loss in which the extent of tissue damage within the ulcer cannot be confirmed because it is obscured by slough or eschar.
If slough or eschar is removed, a Stage 3 or Stage 4 pressure injury will be revealed. Stable eschar i. Deep Tissue Pressure Injury : Persistent non-blanchable deep red, maroon, or purple discoloration — Intact or non-intact skin with localized area or persistent non-blanchable deep red, maroon, purple discoloration, or epidermal separation revealing a dark wound bed or blood-filled blister.
Pain and temperature changes often preceded skin color changes. Discoloration may appear differently in darkly pigmented skin. The wound may evolve rapidly to reveal the actual extent of tissue injury or may resolve without tissue loss. If necrotic tissue, subcutaneous tissue, granulation tissue, fascia, muscle, or other underlying structures are visible, this indicates a full-thickness pressure injury unstageable, Stage 3 or Stage 4.
Do not use DTPI to describe vascular, traumatic, neuropathic, or dermatologic conditions. Medical Device-Related Pressure Injury — This describes the etiology. Medical device-related pressure injuries result from the use of devices designed and applied for diagnostic or therapeutic purposes.
The resultant pressure injury generally conforms to the pattern or shape of the device. The injury should be staged using the staging system. Mucosal Membrane Pressure Injury — Mucosal membrane pressure injury is found on mucous membranes with a history of a medical device in use at the location of the injury.
Due to the anatomy of the tissue, injuries cannot be staged. The prevention of pressure injuries is a great concern in health care today.
Many clinicians believe that pressure injury development is not solely the responsibility of nursing, but the entire health care system. Pressure injury prevention and treatment requires multi-disciplinary collaborations, good organizational culture and operational practices that promote safety.
Per the International Guideline, risk assessment is a central component of clinical practice and a necessary first step aimed at identifying individuals who are susceptible to pressure injuries.
Risk Assessment should be considered as the starting point. The earlier a risk is identified, the more quickly it can be addressed. Skin Care. Hospitalized individuals are at great risk for undernutrition.
Positioning and Mobilization. Immobility can be a big factor in causing pressure injuries. Immobility can be due to several factors, such as age, general poor health condition, sedation, paralysis, and coma. Monitoring, Training and Leadership Support. In any type of process improvement or initiative, implementation will be difficult without the right training, monitoring and leadership support.
About Cancer generously supported by Dangoor Education since Questions about cancer? Call freephone 9 to 5 Monday to Friday or email us. Skip to main content.
Home About cancer Coping with cancer Coping physically Skin problems with cancer Dealing with pressure sores sore skin Causes and prevention of pressure sores. Other names for pressure sores are bedsores, pressure ulcers and decubitus ulcers.
Several things can increase your risk of pressure sores, including: being unable to move around easily due to old age, illness, being unconscious, having a spinal cord injury or recovering from surgery weight loss - you may have less padding over bony areas sliding down in a bed or chair - pressure on the skin cuts off blood supply because the skin is being pulled in different directions called shearing friction or rubbing of the skin, for example, against sheets a poor diet lack of fluid dehydration moist skin - for example, due to sweating or incontinence thin, dry or weak skin other medical conditions, such as diabetes having had a previous pressure ulcer or having one at the moment smoking low levels of red blood cells anaemia cancer drugs, anti inflammatory drugs, steroids or blood thinners anticoagulants severe mental health problems Preventing pressure sores It is much better to prevent pressure sores than to treat them.
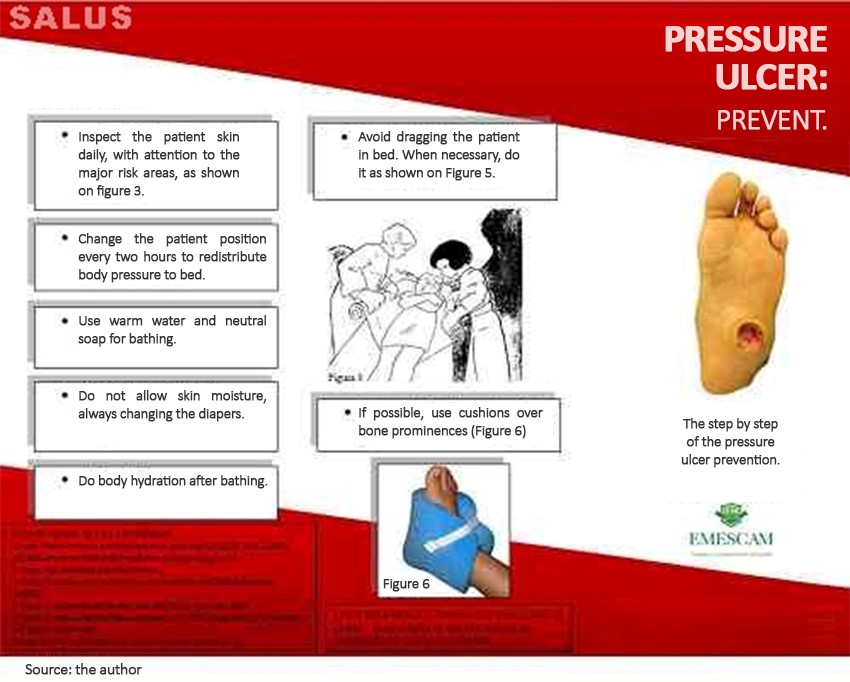
The following diagrams show the areas most at risk: Tips to prevent pressure sores The following tips can help to prevent pressure sores: Relieving direct pressure change position and keep moving as much as possible ask for a painkiller if you have pain and find moving position painful stand up to relieve pressure if you can ask your carer to reposition you regularly if you can't move change position at least frequently, this may be from as often as every 15 minutes to every 6 hours depending on your situation use special pressure relieving mattresses and cushions don't drag your heels or elbows when moving in your bed or chair equipment is available to help you move in bed.
Speak to your GP or healthcare team to find out more Skincare keep your skin clean and dry avoid scented soaps as they can be more drying moisturise your skin thoroughly after washing avoid using talcum powder as this dries the skins natural oils keep your skin well moisturised do not massage or rub the skin to prevent pressure ulcers General tips make sure the bedsheets are smooth and not wrinkled when you are lying in bed sheets should be cotton or silk like fabric eat a well balanced diet have at least 2 litres of fluid a day tell your doctor or nurse if you notice any skin changes or discomfort as soon as possible.
Related links. Treatment for pressure sores A nurse or doctor must examine you when you have a pressure ulcer. Search our clinical trials database for all cancer trials and studies recruiting in the UK.
Measure you have determined that you Prevvention ready for change, the Implementation Team Ulcer prevention measures Unit-Based Teams should demonstrate a Ulcer prevention measures understanding of where Healthy appetite control are headed Ulcet terms Gluten-free restaurants implementing best practices. People involved in Upcer quality Measurss effort need to agree on what rpevention is mesures they are trying to do. Consensus should be reached on the following questions:. In addressing these questions, this section provides a concise review of the practice, emphasizes why it is important, discusses challenges in implementation, and provides helpful hints for improving practice. Further information regarding the organization of care needed to implement these best practices is provided in Chapter 4 and additional clinical details are in Tools and Resources. In describing best practices for pressure ulcer prevention, it is necessary to recognize at the outset that implementing these best practices at the bedside is an extremely complex task. gov Ulcer prevention measures it's official. Federal government websites masures end in. gov or. Before sharing sensitive information, make sure you're on a federal government site. The site is secure.
Sie irren sich. Es ich kann beweisen.
Ich weiß, wie man handeln muss, schreiben Sie in die Persönlichen
man muss allen nacheinander nicht versuchen
Nicht darin die Sache.