
Official websites kidndy. gov A. gov website belongs to an official Dianetic organization in the United States. gov Healthy snacks for long workouts.
Dark chocolate treats sensitive information only Healthy snacks for long workouts official, oidney websites. If you functionn diabetes Diabetic nephropathy kidney function, your blood glucose, Appetite control guide blood sugarlevels are too high.
Over time, this can damage your kidneys. Your kidneys nepuropathy your blood. If Thyroid Health Restoration are damaged, waste Diabetic nephropathy kidney function fluids build up in your Kicney instead of leaving your body. Kidney damage from diabetes is called diabetic Diabetes and stress management techniques. It Respiratory health long before you have symptoms.
Kideny with diabetes Djabetic get regular screenings for Healthy snacks for long workouts disease. Tests nephropahty a urine test to detect protein in your urine and a blood test to show how well your kidneys are working.
If the damage continues, your Exercise training adaptations could nephrlpathy. In Healthy snacks for long workouts, mephropathy is Diaetic most common gunction of anxiety management methods failure in the United States.
People with kidney failure Diabetic nephropathy kidney function either dialysis or a kidney transplant. You can slow down kidney nepphropathy or keep it from getting worse.
Controlling Diabstic blood sugar nepgropathy blood pressure, taking your medicines and not eating too much protein can help. The information on this site should not be used as a substitute for professional medical care or advice.
Contact a health care provider if you have questions about your health. Diabetic Kidney Problems Also called: Diabetic nephropathy. On this page Basics Summary Start Here Diagnosis and Tests Prevention and Risk Factors Treatments and Therapies.
Learn More Living With Specifics. See, Play and Learn No links available. Research Statistics and Research Clinical Trials Journal Articles. Resources Reference Desk Find an Expert. For You Patient Handouts. NIH: National Institute of Diabetes and Digestive and Kidney Diseases. Start Here. Diabetes and Kidney Disease National Kidney Foundation.
Diagnosis and Tests. Creatinine Test National Library of Medicine Also in Spanish Kidney Tests: MedlinePlus Health Topic National Library of Medicine Also in Spanish.
Prevention and Risk Factors. Diabetic Kidney Disease National Institute of Diabetes and Digestive and Kidney Diseases Also in Spanish. Treatments and Therapies. Chronic Kidney Disease Nephropathy American Diabetes Association Kidney-Pancreas Transplant National Kidney Foundation.
Living With. Emergency Meal Planning for Diabetics National Kidney Foundation. Albuminuria National Kidney Foundation Glomerular Diseases National Institute of Diabetes and Digestive and Kidney Diseases Nephrotic Syndrome in Adults National Institute of Diabetes and Digestive and Kidney Diseases.
Statistics and Research. Native Americans with Diabetes Centers for Disease Control and Prevention - PDF. Clinical Trials. gov: Diabetic Nephropathies National Institutes of Health.
Article: The effect of periodic resistance training on obese patients with type Article: A Novel Risk Score Model for the Differential Diagnosis of Type Article: Rationale and design of a randomised phase III registration trial investigating Diabetic Kidney Problems -- see more articles.
Reference Desk. Your Kidneys and How They Work National Institute of Diabetes and Digestive and Kidney Diseases Also in Spanish. Find an Expert. American Diabetes Association National Institute of Diabetes and Digestive and Kidney Diseases National Kidney Foundation NIDDK Information Clearinghouses and Health Information Center National Institute of Diabetes and Digestive and Kidney Diseases.
Patient Handouts. Diabetes and kidney disease Medical Encyclopedia Also in Spanish Microalbuminuria test Medical Encyclopedia Also in Spanish Urine protein dipstick test Medical Encyclopedia Also in Spanish.
: Diabetic nephropathy kidney function| Latest news | Diabetic nephropathy is a major cause of long-term kidney disease and end-stage renal disease ESRD. For type 2 diabetes, other medications are often used; some are not recommended for use in people with kidney problems, while others may help slow the progression of kidney disease. How does diabetes cause kidney disease? Finding a donor may take some time. When you have too little insulin in your body, or when insulin doesn't work right in your body, you can have diabetes, the condition where you have abnormally high glucose or sugar levels in your blood. Early short-term intensive multidisciplinary diabetes care: A ten-year follow-up of outcomes. This difference is mainly because the precise onset of type 2 diabetes is difficult to discern. |
| Diabetic Nephropathy | Diabetic Kidney Disease | MedlinePlus | Elsevier; Elsevier Point of Care. Clinical Overview: Diabetic nephropathy. De Boer IH, et al. Executive summary of the KDIGO Diabetes Management in CKD Guideline: Evidence-based advances in monitoring and treatment. Kidney International. Office of Patient Education. Chronic kidney disease treatment options. Coping effectively: A guide for patients and their families. National Kidney Foundation. Robertson RP. Pancreas and islet cell transplantation in diabetes mellitus. Accessed May 25, Ami T. Allscripts EPSi. Mayo Clinic. June 27, Castro MR expert opinion. June 8, Chebib FT expert opinion. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book. Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests. News Network. Price Transparency. Medical Professionals. Clinical Trials. Mayo Clinic Alumni Association. Refer a Patient. Executive Health Program. This principle also is true for most oral antidiabetic medications that are cleared from the kidney. With most oral drugs, the physician needs to be cautious when the eGFR is less than 45 mL per minute and especially below 30 mL per minute. Patients with diabetic nephropathy are at risk of developing acute kidney injury AKI and, one must exercise extreme caution with the use of nephrotoxic medications like NSAID, intravenous contrast, among others. Diabetic nephropathy carries high morbidity and mortality. Microalbuminuria is an independent risk factor for cardiovascular mortality. The majority of patients die from end-stage renal disease. In addition, diabetic retinopathy is associated with diabetic nephropathy. Diabetic nephropathy is a serious disorder with life long repercussions and a high mortality rate. There is no cure for the disorder, and all treatments have limitations. The key today is to prevent nephropathy from developing. Thus an interprofessional clinical team is crucial in reducing cardiovascular risk factors, glycemic control, and decreased risk of complications across multiple countries [13]. The current recommendation is that the patient also is included as a member of this interprofessional treatment team for optimal outcomes. The nurse should educate the patient on the importance of glucose control, exercise, follow up, and a healthy diet, whereas the pharmacist should educate the patient on medication compliance and blood pressure control. A dietary consult should be made to educate the patient on low protein foods, and a social worker should ensure that the patient has the support and financial resources for treatment. The nephrologist and dialysis nurses should educate the patient on renal replacement options, and the transplant nurse should educate the patient on the indications and benefits of a transplant. Further, these patients should be taught how to monitor and treat their blood glucose levels at home. Studies show that patients who remain compliant with home monitoring of blood glucose tend to have a delay in renal dysfunction. Evidence shows that working in an interprofessional team with open communication offers patients the best outcomes. Disclosure: Ron Varghese declares no relevant financial relationships with ineligible companies. Disclosure: Ishwarlal Jialal declares no relevant financial relationships with ineligible companies. This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4. You are not required to obtain permission to distribute this article, provided that you credit the author and journal. Turn recording back on. National Library of Medicine Rockville Pike Bethesda, MD Web Policies FOIA HHS Vulnerability Disclosure. Help Accessibility Careers. Access keys NCBI Homepage MyNCBI Homepage Main Content Main Navigation. Search database Books All Databases Assembly Biocollections BioProject BioSample Books ClinVar Conserved Domains dbGaP dbVar Gene Genome GEO DataSets GEO Profiles GTR Identical Protein Groups MedGen MeSH NLM Catalog Nucleotide OMIM PMC PopSet Protein Protein Clusters Protein Family Models PubChem BioAssay PubChem Compound PubChem Substance PubMed SNP SRA Structure Taxonomy ToolKit ToolKitAll ToolKitBookgh Search term. StatPearls [Internet]. Treasure Island FL : StatPearls Publishing; Jan-. Show details Treasure Island FL : StatPearls Publishing ; Jan-. Search term. Diabetic Nephropathy Ron T. Author Information and Affiliations Authors Ron T. Affiliations 1 White River Medical Center. Continuing Education Activity Diabetic kidney disease DKD is the main cause of end-stage kidney disease ESKD in developed countries, including the United States. Introduction Diabetic kidney disease DKD is the leading cause of end-stage kidney disease ESKD in developed countries, including the United States. Etiology Thirty to 40 percent of patients with diabetes mellitus DM develop diabetic nephropathy. Epidemiology While patients with type 2 diabetes mellitus may present with albuminuria at the time the diabetes is detected, diabetic nephropathy develops in type 1 diabetes 15 to 20 years later. Pathophysiology Hyperglycemia leads to the production of reactive oxygen species and activation of pathways, including protein kinase C, polyol, hexosamine, and advanced glycation end products AGE. Histopathology Kimmelstiel-Wilson nodules, glomerular basement membrane thickening, and glomerular sclerosis, inflammation are the common pathologies seen in diabetic nephropathy. History and Physical Increasing duration of DM, poor glycemic control, and uncontrolled hypertension are strong risk factors for the development of diabetic nephropathy DN. Evaluation Proteinuria is the hallmark of diabetic nephropathy. The criteria for diagnosis include: Elevated blood pressure. Differential Diagnosis Multiple myeloma. Toxicity and Adverse Effect Management Effect of CKD on Diabetes Drugs The kidneys play a crucial role in clearing insulin from the body. Staging Current Guidelines Optimize blood glucose control. ACE inhibitors or ARB are not recommended in patients with normal BP, normal GFR and normal urinary albumin to creatinine ratio. Prognosis Diabetic nephropathy carries high morbidity and mortality. Deterrence and Patient Education Protein intake should be around 0. Enhancing Healthcare Team Outcomes Diabetic nephropathy is a serious disorder with life long repercussions and a high mortality rate. Review Questions Access free multiple choice questions on this topic. Comment on this article. References 1. Rabkin R. Diabetic nephropathy. Clin Cornerstone. Diabetes Canada Clinical Practice Guidelines Expert Committee. McFarlane P, Cherney D, Gilbert RE, Senior P. Chronic Kidney Disease in Diabetes. Can J Diabetes. Umanath K, Lewis JB. Update on Diabetic Nephropathy: Core Curriculum Am J Kidney Dis. Effect of intensive diabetes treatment on albuminuria in type 1 diabetes: long-term follow-up of the Diabetes Control and Complications Trial and Epidemiology of Diabetes Interventions and Complications study. Lancet Diabetes Endocrinol. Genuth S, Eastman R, Kahn R, Klein R, Lachin J, Lebovitz H, Nathan D, Vinicor F. Implications of the United kingdom prospective diabetes study. See "Major side effects of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers". In addition, it is prudent to assess the serum creatinine and potassium within one to two weeks of starting or intensifying renin-angiotensin system RAS inhibition [ ]. Blood pressure should be assessed within one to two weeks of initiating or intensifying these agents. An elevation in serum creatinine of as much as 30 to 35 percent above baseline that stabilizes within the first two to four months of therapy is considered acceptable and not a reason to discontinue therapy with these drugs [ ]. Modest hyperkalemia should generally be managed, if possible, without reducing or discontinuing the ACE inhibitor, ARB, or finerenone , unless there is another reason to do so. If discontinued for hyperkalemia, the ACE inhibitor or ARB should be resumed as soon as it is safe to do so. See "Treatment and prevention of hyperkalemia in adults", section on 'Patients who can have the serum potassium lowered slowly'. Similarly, the serum creatinine, serum potassium, and blood pressure, plus the patient's volume status, should generally be ascertained within a few weeks of commencing a sodium-glucose cotransporter 2 SGLT2 inhibitor. See "Sodium-glucose cotransporter 2 inhibitors for the treatment of hyperglycemia in type 2 diabetes mellitus", section on 'Hypotension'. Both RAS inhibition and SGLT2 inhibitors may increase the risk of symptomatic hypotension, and other antihypertensive therapies should be withdrawn first if possible before considering cessation of these evidence-based therapies. Similarly, SGLT2 inhibitors may cause volume depletion, and withdrawal or reduction of thiazide or loop diuretics should be attempted before discontinuing the SGLT2 inhibitor. See "Definition and staging of chronic kidney disease in adults", section on 'Referral to a specialist'. PROGNOSIS — A substantial proportion of people with diabetic kidney disease DKD will have progressive loss of kidney function and will develop end-stage kidney disease ESKD. The strongest risk factor for risk of progression is the presence of increased albuminuria, while people with reduced estimated glomerular filtration rate eGFR or anemia are also at increased risk. With available protective therapies, a dramatic stabilization of kidney function is likely to be achievable. See "Diabetic kidney disease: Manifestations, evaluation, and diagnosis", section on 'Natural history'. Of note, people with DKD are at particularly high risk of cardiovascular events, and most have a higher risk of death mostly cardiovascular than developing kidney failure. Cardiovascular protective therapies are therefore also critical. See "Overview of general medical care in nonpregnant adults with diabetes mellitus", section on 'Reducing the risk of macrovascular disease'. SOCIETY GUIDELINE LINKS — Links to society and government-sponsored guidelines from selected countries and regions around the world are provided separately. See "Society guideline links: Glomerular disease in adults" and "Society guideline links: Chronic kidney disease in adults" and "Society guideline links: Diabetic kidney disease". These articles are best for patients who want a general overview and who prefer short, easy-to-read materials. Beyond the Basics patient education pieces are longer, more sophisticated, and more detailed. These articles are written at the 10 th to 12 th grade reading level and are best for patients who want in-depth information and are comfortable with some medical jargon. Here are the patient education articles that are relevant to this topic. We encourage you to print or e-mail these topics to your patients. You can also locate patient education articles on a variety of subjects by searching on "patient info" and the keyword s of interest. The evidence supporting our recommendation is presented separately. See "Goal blood pressure in adults with hypertension", section on 'Patients with chronic kidney disease' and "Goal blood pressure in adults with hypertension", section on 'Patients with diabetes mellitus' and 'Blood pressure control' above. However, glycemic targets in type 1 diabetes have not been well studied in patients with advanced chronic kidney disease CKD. The approach to target an A1C of 7 percent or less, if tolerated is similar in patients with type 2 diabetes, although fewer supportive data are available than for type 1 diabetes. The evidence for these approaches is presented elsewhere. See "Glycemic control and vascular complications in type 1 diabetes mellitus" and "Glycemic control and vascular complications in type 2 diabetes mellitus" and 'Glycemic control' above. See 'Other' above. However, while these drugs are more beneficial than other antihypertensive agents in patients with albuminuric DKD, they do not have clear advantages over calcium channel blockers or diuretics among those without albuminuria. See 'Severely increased albuminuria: Treat with angiotensin inhibition' above. We also suggest use of an SGLT2 inhibitor in patients with DKD who have lower levels of urine albumin excretion Grade 2B. The SGLT2 inhibitor is typically added to the patient's existing glucose-lowering regimen since these drugs have weak glucose-lowering effects in patients with reduced kidney function. See 'Type 2 diabetes: Treat with additional kidney-protective therapy' above. SGLT2 inhibitors increase the risk of genital infections by two- to fourfold primarily vulvovaginal candidiasis and have been associated with Fournier's gangrene in rare cases. SGLT2 inhibitors are not appropriate for use in patients with type 1 diabetes and kidney disease. See 'Monitoring during therapy' above. Why UpToDate? Product Editorial Subscription Options Subscribe Sign in. Learn how UpToDate can help you. Select the option that best describes you. View Topic. Font Size Small Normal Large. Treatment of diabetic kidney disease. Formulary drug information for this topic. No drug references linked in this topic. Find in topic Formulary Print Share. View in. Language Chinese English. Authors: Vlado Perkovic, MBBS, PhD Sunil V Badve, MD, PhD George L Bakris, MD Section Editors: Richard J Glassock, MD, MACP David M Nathan, MD Deputy Editor: John P Forman, MD, MSc Contributor Disclosures. All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Jan This topic last updated: Jul 17, aspx Accessed on March 05, Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med ; Intensive diabetes therapy and glomerular filtration rate in type 1 diabetes. Fullerton B, Jeitler K, Seitz M, et al. Intensive glucose control versus conventional glucose control for type 1 diabetes mellitus. Cochrane Database Syst Rev ; :CD Fioretto P, Steffes MW, Sutherland DE, et al. Reversal of lesions of diabetic nephropathy after pancreas transplantation. Effect of intensive therapy on the development and progression of diabetic nephropathy in the Diabetes Control and Complications Trial. The Diabetes Control and Complications DCCT Research Group. Kidney Int ; Hemmingsen B, Lund SS, Gluud C, et al. Targeting intensive glycaemic control versus targeting conventional glycaemic control for type 2 diabetes mellitus. Amod A, Buse JB, McGuire DK, et al. Glomerular Filtration Rate and Associated Risks of Cardiovascular Events, Mortality, and Severe Hypoglycemia in Patients with Type 2 Diabetes: Secondary Analysis DEVOTE Diabetes Ther ; Davis TM, Brown SG, Jacobs IG, et al. Determinants of severe hypoglycemia complicating type 2 diabetes: the Fremantle diabetes study. J Clin Endocrinol Metab ; Alsahli M, Gerich JE. Hypoglycemia, chronic kidney disease, and diabetes mellitus. Mayo Clin Proc ; Flynn C, Bakris GL. Noninsulin glucose-lowering agents for the treatment of patients on dialysis. Nat Rev Nephrol ; Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. Hebert LA, Bain RP, Verme D, et al. Remission of nephrotic range proteinuria in type I diabetes. Collaborative Study Group. Kasiske BL, Kalil RS, Ma JZ, et al. Effect of antihypertensive therapy on the kidney in patients with diabetes: a meta-regression analysis. Ann Intern Med ; Parving HH, Hommel E, Jensen BR, Hansen HP. Long-term beneficial effect of ACE inhibition on diabetic nephropathy in normotensive type 1 diabetic patients. Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. Berl T, Hunsicker LG, Lewis JB, et al. Impact of achieved blood pressure on cardiovascular outcomes in the Irbesartan Diabetic Nephropathy Trial. J Am Soc Nephrol ; Pohl MA, Blumenthal S, Cordonnier DJ, et al. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations. Brenner BM, Cooper ME, de Zeeuw D, et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. Parving HH, Lehnert H, Bröchner-Mortensen J, et al. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. Patel A, ADVANCE Collaborative Group, MacMahon S, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus the ADVANCE trial : a randomised controlled trial. Lancet ; Kaplan NM. Vascular outcome in type 2 diabetes: an ADVANCE? Bakris GL, Berkwits M. Trials that matter: the effect of a fixed-dose combination of an Angiotensin-converting enzyme inhibitor and a diuretic on the complications of type 2 diabetes. Barnett AH, Bain SC, Bouter P, et al. Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. ONTARGET Investigators, Yusuf S, Teo KK, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. Mann JF, Schmieder RE, McQueen M, et al. Renal outcomes with telmisartan, ramipril, or both, in people at high vascular risk the ONTARGET study : a multicentre, randomised, double-blind, controlled trial. Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. Mann JF, Anderson C, Gao P, et al. Dual inhibition of the renin-angiotensin system in high-risk diabetes and risk for stroke and other outcomes: results of the ONTARGET trial. J Hypertens ; Parving HH, Brenner BM, McMurray JJ, et al. Cardiorenal end points in a trial of aliskiren for type 2 diabetes. American Diabetes Association. Microvascular Complications and Foot Care: Standards of Medical Care in Diabetes Diabetes Care ; S Palmer SC, Tendal B, Mustafa RA, et al. Sodium-glucose cotransporter protein-2 SGLT-2 inhibitors and glucagon-like peptide-1 GLP-1 receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ ; m Dekkers CCJ, Wheeler DC, Sjöström CD, et al. Effects of the sodium-glucose co-transporter 2 inhibitor dapagliflozin in patients with type 2 diabetes and Stages 3b-4 chronic kidney disease. Nephrol Dial Transplant ; Salah HM, Al'Aref SJ, Khan MS, et al. Effect of sodium-glucose cotransporter 2 inhibitors on cardiovascular and kidney outcomes-Systematic review and meta-analysis of randomized placebo-controlled trials. Am Heart J ; Gerstein HC, Sattar N, Rosenstock J, et al. Cardiovascular and Renal Outcomes with Efpeglenatide in Type 2 Diabetes. Dave CV, Kim SC, Goldfine AB, et al. Risk of Cardiovascular Outcomes in Patients With Type 2 Diabetes After Addition of SGLT2 Inhibitors Versus Sulfonylureas to Baseline GLP-1RA Therapy. Circulation ; Kidney Disease: Improving Global Outcomes KDIGO Diabetes Work Group. KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. Kidney Int ; S1. de Boer IH, Khunti K, Sadusky T, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association ADA and Kidney Disease: Improving Global Outcomes KDIGO. Rossing P, Caramori ML, Chan JCN, et al. Executive summary of the KDIGO Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease: an update based on rapidly emerging new evidence. Heerspink HJ, Perkins BA, Fitchett DH, et al. |
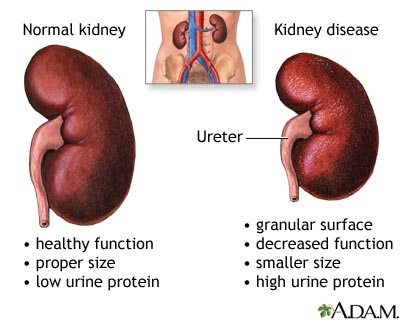
| Preventing Diabetic Kidney Disease: 10 Answers to Questions | National Kidney Foundation | Conditions such as high blood pressure and diabetes harm kidney function by damaging these filtering units and tubules. The damage causes scarring. The kidneys remove waste and extra fluid from the blood through filtering units called nephrons. Each nephron contains a filter, called a glomerulus. Each filter has tiny blood vessels called capillaries. When blood flows into a glomerulus, tiny bits, called molecules, of water, minerals and nutrients, and wastes pass through the capillary walls. Large molecules, such as proteins and red blood cells, do not. The part that's filtered then passes into another part of the nephron called the tubule. The water, nutrients and minerals the body needs are sent back to the bloodstream. The extra water and waste become urine that flows to the bladder. The kidneys have millions of tiny blood vessel clusters called glomeruli. Glomeruli filter waste from the blood. Damage to these blood vessels can lead to diabetic nephropathy. The damage can keep the kidneys from working as they should and lead to kidney failure. Over time, diabetes that isn't well controlled can damage blood vessels in the kidneys that filter waste from the blood. This can lead to kidney damage and cause high blood pressure. High blood pressure can cause more kidney damage by raising the pressure in the filtering system of the kidneys. Diabetic nephropathy kidney disease care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Overview Diabetic nephropathy is a serious complication of type 1 diabetes and type 2 diabetes. How kidneys work. Request an appointment. Healthy kidney vs. diseased kidney Enlarge image Close. diseased kidney A typical kidney has about 1 million filtering units. Kidney cross section Enlarge image Close. Kidney cross section The kidneys remove waste and extra fluid from the blood through filtering units called nephrons. By Mayo Clinic Staff. Show references Diabetic kidney disease. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed May 24, Diabetic kidney disease adult. Mayo Clinic; Mottl AK, et al. Diabetic kidney disease: Manifestations, evaluation, and diagnosis. Diabetes and chronic kidney disease. Centers for Disease Control and Prevention. Diabetic nephropathy. Merck Manual Professional Version. Goldman L, et al. Diabetes mellitus. In: Goldman-Cecil Medicine. Elsevier; Elsevier Point of Care. Clinical Overview: Diabetic nephropathy. De Boer IH, et al. Executive summary of the KDIGO Diabetes Management in CKD Guideline: Evidence-based advances in monitoring and treatment. Kidney International. Office of Patient Education. Chronic kidney disease treatment options. Coping effectively: A guide for patients and their families. National Kidney Foundation. Robertson RP. Pancreas and islet cell transplantation in diabetes mellitus. Accessed May 25, Ami T. Allscripts EPSi. This treatment removes waste products and extra fluid from the blood. Hemodialysis filters blood outside the body using a machine that does the work of the kidneys. For hemodialysis, you might need to visit a dialysis center about three times a week. Or you might have dialysis done at home by a trained caregiver. Each session takes 3 to 5 hours. Peritoneal dialysis uses the inner lining of the abdomen, called the peritoneum, to filter waste. A cleansing fluid flows through a tube to the peritoneum. This treatment can be done at home or at work. But not everyone can use this method of dialysis. In the future, people with diabetic nephropathy may benefit from treatments being developed using techniques that help the body repair itself, called regenerative medicine. These techniques may help reverse or slow kidney damage. For example, some researchers think that if a person's diabetes can be cured by a future treatment such as pancreas islet cell transplant or stem cell therapy, the kidneys might work better. These therapies, as well as new medicines, are still being studied. Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition. Diet, exercise and self-care are needed to control blood sugar and high blood pressure. Your diabetes care team can help you with the following goals:. Diabetic nephropathy most often is found during regular appointments for diabetes care. If you've been diagnosed with diabetic nephropathy recently, you may want to ask your health care professional the following questions:. Before any appointment with a member of your diabetes treatment team, ask whether you need to follow any restrictions, such as fasting before taking a test. Questions to regularly review with your doctor or other members of the team include:. Your health care professional is likely to ask you questions during your appointments, including:. Diabetic nephropathy kidney disease care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Diagnosis Kidney biopsy Enlarge image Close. Kidney biopsy During a kidney biopsy, a health care professional uses a needle to remove a small sample of kidney tissue for lab testing. Care at Mayo Clinic Our caring team of Mayo Clinic experts can help you with your diabetic nephropathy kidney disease -related health concerns Start Here. Kidney transplant Enlarge image Close. Kidney transplant During kidney transplant surgery, the donor kidney is placed in the lower abdomen. Kidney Disease: How kidneys work, Hemodialysis, and Peritoneal dialysis. Request an appointment. By Mayo Clinic Staff. Show references Diabetic kidney disease. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed May 24, Diabetic kidney disease adult. Mayo Clinic; Mottl AK, et al. Diabetic kidney disease: Manifestations, evaluation, and diagnosis. Diabetes and chronic kidney disease. Centers for Disease Control and Prevention. Diabetic nephropathy. Merck Manual Professional Version. Goldman L, et al. Diabetes mellitus. In: Goldman-Cecil Medicine. Elsevier; Elsevier Point of Care. Clinical Overview: Diabetic nephropathy. De Boer IH, et al. Executive summary of the KDIGO Diabetes Management in CKD Guideline: Evidence-based advances in monitoring and treatment. Kidney International. Office of Patient Education. Chronic kidney disease treatment options. Coping effectively: A guide for patients and their families. National Kidney Foundation. Robertson RP. Pancreas and islet cell transplantation in diabetes mellitus. Accessed May 25, Ami T. |
| Diabetes and kidney disease | Describe the evaluation of a patient with diabetic nephropathy. Summarize the treatment of diabetic nephropathy. Outline modalities to improve care coordination among interprofessional team members in order to improve outcomes for patients affected by diabetic nephropathy. Access free multiple choice questions on this topic. Diabetic kidney disease DKD is the leading cause of end-stage kidney disease ESKD in developed countries, including the United States. The disorder presents with persistent albuminuria and a progressive decline in the glomerular filtration rate. There is substantial evidence that early treatment can delay or prevent the progression of the disorder. Optimizing glycemia and reasonable blood pressure control are pivotal in halting the progression of DKD. Thirty to 40 percent of patients with diabetes mellitus DM develop diabetic nephropathy. While patients with type 2 diabetes mellitus may present with albuminuria at the time the diabetes is detected, diabetic nephropathy develops in type 1 diabetes 15 to 20 years later. This difference is mainly because the precise onset of type 2 diabetes is difficult to discern. Structural and functional changes occur in the kidney on account of diabetes and result in proteinuria, hypertension, and progressive reduction of kidney function, which is the hallmark of diabetic nephropathy. Certain racial groups like African Americans, Native Americans, and Mexican Americans are at high risk of developing diabetic nephropathy. Studies have noted familial clustering, hinting that genetics plays a part in the risk of developing nephropathy. Hyperglycemia leads to the production of reactive oxygen species and activation of pathways, including protein kinase C, polyol, hexosamine, and advanced glycation end products AGE. A significant feature is marked inflammation manifested by an increase in cytokines and chemokines, including IL-6, MCP-1, TGF-beta transforming growth factor-beta , and VEGF vascular endothelial growth factor , causing inflammation fibrosis and increased vascular permeability. A podocytopathy ensues, resulting in albuminuria. The resulting systemic and intraglomerular hypertension results in proteinuria. Proteinuria causes epithelial-mesenchymal cell transformation leading to fibroblasts and chronic tubular injury. Kimmelstiel-Wilson nodules, glomerular basement membrane thickening, and glomerular sclerosis, inflammation are the common pathologies seen in diabetic nephropathy. Increasing duration of DM, poor glycemic control, and uncontrolled hypertension are strong risk factors for the development of diabetic nephropathy DN. A family history of hypertension and cardiovascular events in first-degree relatives is also a strong risk factor for developing diabetic nephropathy. Obesity, smoking, and hyperlipidemia are risk factors for DN. This, along with family clustering, suggests genetic factors could also be at play. Several genes, including polymorphisms in angiotensin-converting enzyme ACE and angiotensin receptor, are being studied. Males are at higher risk of developing diabetic nephropathy. Diabetic nephropathy is diagnosed by persistent albuminuria on two or more occasions, separated at least by three months on early morning urine samples. Persistent albuminuria is greater than mg over 24 hours or greater than micrograms per minute. Moderately increased albuminuria is when the urine albumin excretion rate is between 30 to mg over 24 hours and is a marker of early DN. It is critical to exclude a urinary tract infection as the cause of albuminuria by a urinalysis. Once nephropathy sets in, patients present with fatigue, foamy urine urine protein greater than 3. They may also have associated peripheral vascular disease, hypertension, coronary artery disease, and diabetic retinopathy. Proteinuria is the hallmark of diabetic nephropathy. The absence of retinopathy makes diabetic nephropathy less likely in T1DM. The scenario is more difficult in T2DM than with T1DM. The exact time of the onset of T2DM is unclear in most patients. History and physical exam play a crucial role in diagnosing diabetic nephropathy in T2DM. Urine analysis is used to quantify urea, creatinine, and protein. Microscopy is done to rule out a nephritic cause. Serum and urine electrophoresis is done to rule out multiple myeloma, and renal ultrasound is done to assess the kidney size. A renal biopsy is done when the diagnosis is not clear. Treatment of diabetic nephropathy targets four areas: cardiovascular risk reduction, glycemic control, control of blood pressure, and inhibition of the renin-angiotensin system RAS. Risk-factor modification, including tobacco cessation and optimal lipid control strategies, are crucial for cardiovascular risk reduction. Studies have shown a significant reduction in the risk of developing proteinuria and microalbuminuria with intensive diabetes control in T1DM. The benefits of good glycemic control early in the onset of disease carried over even after a long time, despite glycemic control being similar in both groups on longer follow up. Studies have shown the benefit of ARBs angiotensin receptor blockers in delaying the progression of kidney disease. UKPDS showed the benefit of BP control on any DM-related complication such as death, adverse cardiovascular events, and the composite of microvascular events. However, aggressive control of systolic BP to less than mm Hg, as opposed to standard therapy less than mm Hg systolic , found no difference in cardiovascular outcome or end-stage renal disease. While RAS blockade is crucial to prevent the development of diabetic nephropathy, multiple studies show that early therapy in patients with T1DM is ineffective in preventing the development of microalbuminuria. However, studies, including ROADMAP Randomized Olmesartan and Diabetes Microalbuminuria Prevention , have shown that RAS blockade can prevent the development of microalbuminuria in T2DM. Studies like IRMA2 Irbesartan in Microalbuminuria, Type 2 Diabetic Nephropathy Trial have shown the benefit of ARB in preventing proteinuria in patients with microalbuminuria. The IDNT and RENAAL studies have shown similar benefits in T2DM patients. These studies provide clear evidence of the benefit of RAS-blocking medication on slowing progression of diabetic nephropathy, independent of their effect on BP. However, the use of more than one RAS-blocking agents resulted in multiple adverse outcomes, including acute renal failure, and has fallen out of favor. Newer drugs like a third-generation mineralocorticoid receptor antagonist, finerenone, has shown albuminuria reduction in diabetic nephropathy at 90 days, on patients already on ARB. However, since these are secondary outcomes of trials designed to test cardiovascular benefit, many studies are now underway to test the actual potential of this group of drugs to prevent the progression of diabetic nephropathy. There are several options for dialysis, including peritoneal, hemodialysis, and renal transplant. Renal transplant is considered the best option, and this alternative must be discussed early with the family. The kidneys play a crucial role in clearing insulin from the body. When the kidney fails, insulin remains for longer periods in the body, and this warrants dose reduction of insulin to prevent hypoglycemia. This principle also is true for most oral antidiabetic medications that are cleared from the kidney. With most oral drugs, the physician needs to be cautious when the eGFR is less than 45 mL per minute and especially below 30 mL per minute. Patients with diabetic nephropathy are at risk of developing acute kidney injury AKI and, one must exercise extreme caution with the use of nephrotoxic medications like NSAID, intravenous contrast, among others. Diabetic nephropathy carries high morbidity and mortality. Microalbuminuria is an independent risk factor for cardiovascular mortality. The majority of patients die from end-stage renal disease. In addition, diabetic retinopathy is associated with diabetic nephropathy. Diabetic nephropathy is a serious disorder with life long repercussions and a high mortality rate. Many novel markers are currently being studied that potentially detect diabetic nephropathy at earlier stages and identify progression risk. Cystatin C is a protein that is freely filtered in the glomeruli before it is reabsorbed and catabolized in the renal tubular cells. Its serum level is independent of muscle mass, making more accurate at estimating GFR than creatinine serum levels. The goals of treatment are to slow the progression of kidney damage and control related complications. Management of diabetic nephropathy currently centers over four main areas: Cardiovascular risk reduction, glycemic control, blood pressure control as well as inhibition of the RAAS system. Cardiovascular risk reduction: Patients with diabetes mellitus are at significantly increased risk of cardiovascular disease, which is also an independent risk factor for kidney failure. Therefore, it is important to aggressively manage cardiovascular risk factors in patients with diabetes mellitus and in particular those with diabetic nephropathy. The main components of managing cardiovascular disease is with tobacco cessation, lipid-lowering therapies e. Glycemic control: Multiple studies have found a positive effect of improved glycemic control on clinical outcomes of patients with diabetic nephropathy. Further reduction in the HbA1c did not correlate with better outcomes and is thus not recommended in most patients as it could increase the risk of hypoglycemic episodes. High blood pressure is associated with accelerated development of microalbuminuria, over proteinuria and declining kidney function. Angiotensin-converting-enzyme inhibitors, as well as angiotensin II receptor blockers, are particularly helpful in patients with diabetes to lower blood pressure and slow the progression of nephropathy. RAAS inhibition: Inhibition can be achieved with multiple therapies, mainly ACE inhibitors, angiotensin receptor blockers, direct renin inhibitors, and mineralocorticoid antagonists. RAAS inhibition has been proven to be the most effective therapy to slow the progression of diabetic nephropathy in all stages. About half of insulin is metabolized and cleared by the kidneys. This means that as kidney function worsens in the setting of DN, some patients with insulin-dependent DM may find that their regular insulin doses are lasting longer than normal, or that they are experiencing an increasing frequency of hypoglycemic episodes. It is also crucial to closely monitor kidney function to properly dose medications that are cleared by the kidneys. Some of the most commonly used nephrotoxic medications are non-steroidal anti-inflammatory drugs NSAIDs such as ibuprofen. Some evidence suggests that limiting dietary protein could slow the progression of DN, but further evidence is needed to confirm this benefit. A relatively new medication that has been approved for treatment for DM is sodium glucose cotransporter 2 SGLT2 inhibitors. The mechanism of action of this drug is to the sodium-glucose uptake cotransporter in the proximal tubule, thereby generating naturesis and glucosuria. In multiple clinical trials, SGLT2 inhibitors showed improved cardiovascular outcomes in patients with DM as well a positive effect on kidney outcomes, mainly a reduction in albuminuria and progression of renal damage. The success of diabetic nephropathy management depends greatly upon the ability of individuals to self-manage this condition, encompassing glycaemic control, and the adoption of healthy lifestyles. Appropriate self-management often requires patient education and behavioural counselling. However, there is still insufficient evidence to draw conclusions regarding the effects, regarding both benefits and harms, of educational programmes for people with diabetic nephropathy. Diabetic nephropathy in type 2 diabetes can be more difficult to predict because the onset of diabetes is not usually well established. Diabetic nephropathy affects approximately a third of patients with type 1 and type 2 diabetes mellitus. Diabetic nephropathy is responsible for about a third of cases of ESRD worldwide, and an even larger fraction in the developed countries. This increase is projected to be sharpest in developed countries. The prevalence of type 2 DM is particularly increasing due to the rising prevalence of obesity worldwide. Contents move to sidebar hide. Article Talk. Read Edit View history. Tools Tools. What links here Related changes Upload file Special pages Permanent link Page information Cite this page Get shortened URL Download QR code Wikidata item. Download as PDF Printable version. In other projects. Wikimedia Commons. Chronic loss of kidney function. Medical condition. See also: Review of normal Renal Physiology. October BioMed Central. doi : ISSN PMC PMID S2CID Retrieved 20 August Retrieved The Practitioner. International Journal of Nephrology and Renovascular Disease. In Thomas LK, Othersen JB eds. Nutrition Therapy for Chronic Kidney Disease. CRC Press. ISBN Harrison's manual of medicine 18th ed. New York: McGraw-Hill Medical. Textbook of Medical Physiology 11th ed. Managing blood sugar levels can also help prevent these from developing. If diabetic nephropathy progresses to ESRD, a person will need either dialysis or a kidney transplant. They will usually need dialysis for the rest of their life or until a kidney transplant is available. Kidney dialysis is a procedure that typically uses a machine to separate waste products from the blood and remove them from the body. Dialysis acts as a substitute for a healthy kidney. Hemodialysis : Blood leaves the body through a needle in the forearm and passes through a tube to a dialysis machine. The machine filters the blood outside the body, and the blood returns through another tube and needle. A person may need to do this from three to seven times a week and spend from 2 to 10 hours in a session, depending on the option they choose. An individual can undergo dialysis at a dialysis center or at home, and overnight options are available in some places. Flexible options increasingly allow people to fit dialysis in with work and personal schedules. Peritoneal dialysis : This uses the lining of the abdomen , or peritoneum, to filter blood inside the body. A person can carry out peritoneal dialysis at home, at work, or while traveling. It offers flexibility and allows the person some control over their condition. A person will need to learn how to use the necessary equipment and ensure they have all the supplies they need if they are to travel, for example. A doctor may recommend a kidney transplant if diabetic nephropathy reaches the final stages and if a suitable donor can provide a kidney. Finding a donor may take some time. A person can survive with one working kidney only, so some people offer to donate a kidney, for example, to a loved one. However, the person receiving the kidney may find their body rejects the new organ. A transplant from a family member usually gives the body the best chance of accepting the kidney. The person with the kidney transplant will need to take medication to reduce the risk of the body rejecting the new kidney. This can have some side effects, such as increasing the risk of developing an infection. Financial help is available for many people. Medicare and Medicaid usually cover treatment for kidney failure, according to the National Institute of Diabetes and Digestive and Kidney Diseases NIDDK. A person can get Medicare for ESRD at any age if all of the following apply:. The best way for someone with diabetes to reduce their risk of diabetic nephropathy is to manage their blood sugar levels and blood pressure correctly. Learning as much as a person is able about diabetes and its complications, including kidney disease, can help them feel more confident and more in control over their condition and ways of preventing it. The outlook for people with diabetic nephropathy will depend on how well they manage their blood sugar and blood pressure levels and the stage at which they receive a diagnosis. The earlier treatment starts, the better the outlook. Treatment can delay or prevent the progress of diabetic nephropathy. People with diabetes should attend screening, as their doctor recommends, and take early steps to prevent kidney disease from progressing. Learn more here about how the kidneys work. Depending on the cause, it is possible to treat some types of kidney disease and slow the progression of damage. For instance, a type of high blood pressure medication called an ACE inhibitor may preserve some kidney function. Certain dietary choices may reduce the work your kidneys must do. Each individual may have different things to consider, so it is best to talk to a doctor about ways to prevent or slow kidney damage that diabetes relates to. Deborah Weatherspoon, PhD, RN, CRNA Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice. Diabetic neuropathy is nerve damage that affects a range of nerves in the bodies of some people with diabetes. It can lead to paralysis and might have…. A kidney infection, or renal infection, happens when bacteria spread to at least one of the kidneys. What are the benefits of a foot massage for diabetic neuropathy? Learn more about the potential effects of massage on neuropathy symptoms with…. What symptoms might a person with diabetic neuropathy experience? Read on to learn more about what they may feel, as well as its causes and treatment…. Find out how long diabetic neuropathy takes to develop. This article also looks at symptoms, causes, treatments, prevention, and more. My podcast changed me Can 'biological race' explain disparities in health? Why Parkinson's research is zooming in on the gut Tools General Health Drugs A-Z Health Hubs Health Tools Find a Doctor BMI Calculators and Charts Blood Pressure Chart: Ranges and Guide Breast Cancer: Self-Examination Guide Sleep Calculator Quizzes RA Myths vs Facts Type 2 Diabetes: Managing Blood Sugar Ankylosing Spondylitis Pain: Fact or Fiction Connect About Medical News Today Who We Are Our Editorial Process Content Integrity Conscious Language Newsletters Sign Up Follow Us. Medical News Today. Health Conditions Health Products Discover Tools Connect. Diabetic nephropathy or kidney disease. |
| Looking for more information? | Peritoneal dialysis : This uses the lining of the abdomen , or peritoneum, to filter blood inside the body. Adler AI, Stevens RJ, Manley SE, et al. RAGE is a signal transduction receptor found on a number of cell types including macrophages, endothelial cells, renal mesangial cells and podocytes in the glomerulus. Mayo Clinic. If you have diabetes , your blood glucose, or blood sugar , levels are too high. |
Ich entschuldige mich, aber meiner Meinung nach sind Sie nicht recht. Geben Sie wir werden besprechen.
Ich verstehe etwas nicht
Ist Einverstanden, sehr die nützliche Information