
Video
The 2nd Worst Cause of Insulin Resistance (\u0026 Visceral Fat)Visceral fat and insulin resistance -
There is a high prevalence of type 2 diabetes mellitus and coronary artery disease among urban and migrant Asian Indians despite the absence of traditional risk factors. Evidence exists that Asian Indians are more hyperinsulinemic than Caucasians and that hyperinsulinemia may be important in the development of these diseases.
To test whether insulin action was related to total or regional adiposity and to explore the potential role of plasma leptin and lipids, we measured insulin-mediated glucose disposal by the euglycemic insulin clamp, adipose distribution and muscle volume using computed axial tomography, and fasting serum leptin and lipid levels in 20 healthy Asian Indian male volunteers age, 36 ± 10 yr.
A mean body mass index of The mean fasting serum leptin level was 7. Insulin action was inversely correlated with visceral adipose tissue, not total or abdominal sc adipose tissue. In contrast, leptin levels correlated with sc and total not visceral adipose tissue.
Serum triglyceride and high density lipoprotein cholesterol levels were inversely correlated with each other and were directly related to insulin resistance and visceral not subcutaneous fat. Increased visceral fat in Asian Indians is associated with increased generalized obesity, which is not apparent from their nonobese body mass index.
Increased visceral fat is related to dyslipidemia and increased frequency of insulin resistance and may account for the increased prevalence of diabetes mellitus and cardiovascular disease in Asian Indians. THE HIGH prevalence of type 2 diabetes mellitus and coronary artery disease in migrant and urban Asian Indians has been difficult to explain because the traditional risk factors for Caucasian populations do not appear to be present 1 — 4.
Coronary artery disease is 6-fold more prevalent in urban than rural Indians living in India and 1. The traditional risk factors for coronary artery disease, such as smoking, hypertension, and obesity, do not appear to explain their increased risk 8 , 9. Plasma lipid levels vary significantly among the various Indian religious subgroups and are not particularly elevated compared to those in Europeans.
However, studies have shown consistently that hyperinsulinemia is present in a high percentage of both urban and migrant Asian Indians 9 — 14 and could explain some of the increased prevalence of type 2 diabetes and coronary artery disease 15 — Among Caucasians and African-Americans, the BMI values of Asian Indians would not be associated with such a high prevalence of insulin resistance.
Epidemiological studies suggest that the distribution of fat, especially visceral obesity, may be a more important determinant of insulin resistance, diabetes, and cardiovascular disease than generalized obesity 19 — This study was designed to test the hypothesis that insulin resistance and dyslipidemia are related to visceral, not sc, adipose tissue volume and to explore the role of plasma leptin in migrant Asian Indians living in the United States.
We correlated these measures with fasting serum lipid and leptin levels. Twenty Asian Indian healthy male volunteers without a known history of diabetes were studied mean ± sd age, The subjects were professionals working at the medical center.
Oral glucose tolerance testing 2 h with 75 g oral glucose showed a mean ± sd fasting plasma glucose of 5. Ten of 20 subjects had a first degree family history of diabetes mellitus.
Four subjects had impaired glucose tolerance based on the WHO 23 criteria mean fasting plasma glucose, 5. One subject was diabetic BMI, Subjects had maintained a constant body weight for at least 3—4 months before the study.
None had significant renal, hepatic, or cardiac disease, and none was using agents known to affect glucose metabolism. The control population for plasma insulin during the oral glucose tolerance test consisted of 15 normal African-American men with a similar mean age of All subjects were instructed to consume at least g carbohydrate for 3 days before any study and had fasted overnight before morning studies.
The study was approved by the institutional review board of the State University of New York Health Science Center Brooklyn, NY. All patients gave written informed consent.
The patients were studied in the Clinical Research Center at University Hospital Brooklyn, NY. A GE Pace scanner Milwaukee, WI was used to calculate the total intraabdominal visceral and total and abdominal sc adipose tissue volume and total muscle volume.
Twenty-two scans were performed at the anatomical levels recommended by Sjöström Techniques for analysis and volume calculations have been previously described Using a tape measure, with the subject standing, the waist was measured as the narrowest circumference between the lower costal margin and the iliac crest.
The hip was the maximum circumference at the level of the femoral trochanters. At this level of insulin infusion, hepatic glucose production is virtually negligible in diabetic and nondiabetic subjects 25 — Plasma glucose was measured by a glucose oxidase method using a Beckman Coulter, Inc.
glucose analyzer Fullerton, CA. Stillwater, MN. Hemoglobin A 1c was determined using the Bayer DCA West Haven, CT , with an upper limit of normal of 6. Serum leptin was measured using a double antibody RIA kit from Linco Research, Inc.
Charles, MO , with a lower limit of detection of 0. Linear and multiple regression and Ridge regression analyses were performed Data are expressed as the mean ± sd.
The clinical characteristics of the study subjects are given in Tables 1 1 and 2 2. Despite a mean body mass index of These are similar to reports of hyperinsulinemia in Asian Indians compared with different ethnic groups 13 , The mean waist circumference Two thirds of the subjects 13 of 20 were insulin resistant, whereas only one third 7 of 20 were normally insulin sensitive compared to our published controls Because glucose disposal is primarily a function of muscle mass 31 , we have also expressed it as glucose disposal per kg lean body mass LBM , which ranged from This expression of glucose disposal is used in all subsequent analyses.
Although the degree of insulin resistance in these subjects appeared inconsistent with their normal BMI of By this criteria they are significantly obese.
This corresponded to a total body adipose tissue volume of Eighty-one percent of the fat was sc Total muscle volume was We next determined the extent to which insulin action was correlated with generalized or regional adiposity.
To determine which adipose tissue compartment was the more significant predictor of insulin-mediated glucose disposal, we performed an overall multivariate analysis that tested total body, visceral, and abdominal sc adipose tissue volume entered in a stepwise fashion.
An analysis of the data excluding the single diabetic subject visceral adipose tissue volume, 6. Simple correlations of insulin-mediated glucose disposal and body composition. Thus, the waist circumference is a better surrogate than WHR for both visceral adipose tissue volume and insulin-mediated glucose disposal.
Despite its significant correlations, the waist circumference does not distinguish which of its two adipose tissue components visceral or sc is the more important predictor of insulin-mediated glucose disposal. Because of the high prevalence of coronary artery disease among Asian Indians, we investigated the interrelationships of plasma lipids, visceral adipose tissue, and insulin action Table 5.
The fasting serum triglyceride level was 2. In contrast, neither total sc nor abdominal sc adipose tissue was related to serum lipid levels. Fasting serum lipid levels in Asian Indian men and correlations with insulin action and visceral and abdominal sc adipose tissue volume.
Data are the mean ± sd. Significance was based on two-tailed t test. Although Asian Indians have increased generalized adiposity, the metabolic abnormalities of insulin resistance and dyslipidemia are related to visceral, not total or sc, adipose tissue.
Therefore, an obvious question was to which adipose tissue compartment was leptin, a neuroregulatory hormone produced by fat cells, related. Fasting serum leptin levels ranged from 3. As might be expected, serum leptin was not correlated with glucose disposal or plasma lipids.
Relationship between sc adipose tissue liters and fasting serum leptin levels nanograms per mL. The main points emerging from our data are the following 1 Asian Indians have an unexpectedly high percentage of body fat relative to body mass index and muscle mass; this is associated with a proportionate increase in visceral fat.
The data support the hypothesis that among Asian Indians, increased visceral, not sc, adipose tissue volume is associated with insulin resistance, hyperinsulinemia, and dyslipidemia and may explain their propensity for increased cardiovascular disease and diabetes.
Plasma leptin levels, in contrast, are associated with sc adipose tissue volume. A 5-fold increase in the prevalence of diabetes is associated with an increase in BMI but no change in the WHR in urban compared to rural Asian Indians in India 5.
In contrast, the 4-fold increase in diabetes is associated with a lower or similar BMI and higher WHR in migrant Asian Indians in the United Kingdom compared to Europeans 9. At every level of WHR, these Asian Indians have higher plasma insulin levels and are more insulin resistant than their European counterparts 9 , Our direct CT measures of body composition may help explain these discrepancies.
The high body fat and low muscle mass may explain the high prevalence of hyperinsulinemia and the greater risk for development of type 2 diabetes. Relationship between percent body fat and body mass index in Asian Indian and African-American men.
Comparative body compositions in Asian Indian, African American, and Caucasian men. African American or Caucasian. Studies have shown that anthropometric measures, BMI, WHR, and waist circumference, are not comparable measures across different racial populations.
Our data showing lower waist circumference and WHR in Asian Indian compared to African-American diabetic men, yet identical visceral adipose tissue volumes [waist, The distribution of adipose tissue appears not to be markedly different in Asian Indian compared to African-American diabetic men or Swedish men when using comparable CT methods.
In contrast, anthropometry BMI and WHR suggested that migrant Asian Indians compared to Europeans have lower overall obesity, with a selective increase in central obesity 9. Our data from Asian Indian men and African American diabetic men and women 21 indicate that ,visceral not abdominal, sc adipose tissue mass is the principal adipose tissue determinant of insulin-mediated glucose disposal.
Most studies are consistent with these data. The increase in total body fat in Asian Indians results in an increase in visceral fat and an expected increase in insulin resistance. Plasma insulin responses to oral glucose a surrogate for insulin action were correlated with visceral adipose tissue CT 39 — Glucose disposal clamp method was inversely correlated with waist circumference in men and women 42 , and plasma insulin levels inversely were correlated with the WHR in obese, but not lean, Asian Indians The reasons for these differences are unclear, but may be related to race, degree of obesity, or the close correlation of different adipose tissue compartments.
The importance of visceral fat can also be shown in intervention and longitudinal studies. Weight loss by diet or dexfenfluramine treatment showed improvement of insulin action and plasma insulin to be due to the loss of visceral, not abdominal sc, adipose tissue 48 — Visceral fat and WHR are linked to the development of glucose intolerance in many populations, including Asian Indians 5 , 9 , 10 , 19 , 20 , 51 — There are conflicting reports as to whether plasma leptin, the neuroregulatory peptide produced by fat cells, is associated with total body, sc or visceral adipose tissue 55 — Most report a strong association of plasma leptin and leptin messenger RNA with BMI or percent body fat 55 , 56 but do not report body fat distribution.
In normoglycemic Asian Indian men, leptin was associated with the total not visceral or sc fat area in the abdominal region single slice CT However, a Swedish study in twins using single slice magnetic resonance imaging reported visceral, not sc, adipose tissue to be the significant correlate of leptin levels Our data clearly show that in Asian Indian men, plasma leptin is associated with sc, not visceral, adipose tissue volume or insulin-mediated glucose disposal.
We acknowledge the excellent assistance of the nurses and staff of the Clinical Research Center and the Department of Radiology at State University of New York Health Science Center at Brooklyn in carrying out these studies.
Also, Dr. Peter Homel, Scientific and Academic Computing Center, State University of New York-Brooklyn, is gratefully acknowledged for assistance with statistical analyses. This work was supported by grants from the Diabetes Research and Education Foundation. Wild S , McKeigue P.
Br Med J. Google Scholar. Simmons D , Williams DAR , Powell MJ. Diabetic Med. Verma NPS , Mehta AP , Madhu S , Mather HM , Keen H. McKeigue P , Miller GJ , Marmot MG.
J Clin Epidemiol. Ramachandran A. Snehalatha C. Dharmaraj D. Viswanathan M. Urban-rural difference and significance of upper body adiposity. Diabetes Care. Ramchandaran A , Jali MV , Mohan V , Snehalatha C , Viswanathan M. Omar MA , Seedat MA , Dyer RB , Motala AA , Knight LT , Becker PJ.
Beckles GLA , Miller GJ , Kirkwood BR , Alexis SD , Carson DC , Byam NTA. McKeigue PM , Shah B , Marmott MG. Cruikshank JK , Cooper J , Burnett M , MacDuff J , Drubra U. Omar MAK , Asmal AC. Trop Geogr Med. Dowse GK , Zimmet PZ , Alberti KGMM , et al. Mohan V , Sharp PS , Cloke HR , Burrin JM , Schumer B , Kohner EM.
Snehalatha C , Ramchandaran A , Vijay V , Viswanathan M. Diabetic Medicine. Knight TM , Smith Z , Whittles A , et al. Br Heart J. McKeigue PM , Ferrie JE , Pierpont T , MG Marmott. Singh RB , Ghosh S , Niaz AM , et al.
Int J Cardiol. Dhawan J , Bray CL , Warburton R , Ghambhir DS , Morris J. Genetic or environmental effect? Lundgren H , Bengtsson C , Blohmé G , Lapidus L. Int J Obesity. Ohlson L-O , Larsson B , Svärdsudd K , et al. Banerji MA , Lebowitz J , Chaiken RL , Gordon D , Kral JG , Lebovitz HE.
Am J Physiol. Bjorntorp P. WHO Expert Committee on Diabetes Mellitus. Geneva : WHO; Who Tech Rep Ser Kvist H , Sjöström L , Tylén U. Rizza RA , Mandarino LJ , Gerich JE. Pigon J , Giacca A , Ostenson C-G , Lam L , Vranic M , Efendic S. J Clin Endocrinol Metab. Banerji MA , Lebovitz HE.
Neter J , Wasserman W , Kutner MH. Homewood : Irwin. Muller DC , Elahi D , Tobin JD , Andres R. Aging Clin Exp Res. Thiebaud D , Jacot E , DeFronzo RA , Maeder E , Jequier E , Felber JP. Shelgikar KM. Hockaday TD. Yajnik CS. Mckeigue PM , Pierpont T , Ferrie JE , Marmot MG.
Laws A , Jeppesen JL , Maheux PC , Schaaf P , Chen YD , Reaven GM. Arterioscler Thromb. Banerji MA , Chaiken RL , Kral JG , Lebovitz HE. Aim: Clinical heterogeneity exists in overall obesity and abdominal obesity in terms of insulin secretion and sensitivity.
Further, the impact of visceral fat VF on the first- and second-phase insulin secretion FPIS and SPIS is controversial.
We aim to investigate insulin secretion and sensitivity in Chinese patients with T2DM according to different BMI and VF levels. Methods: This study enrolled participants. A dual bioelectrical impedance analyzer was used to assess the visceral and subcutaneous fat area VFA and SFA.
VF levels were categorized as normal or high, with the cutoff value of cm 2. FPIS and SPIS were evaluated by arginine stimulation test and standardized steamed bread meal tolerance test, respectively.
Multivariate linear regression showed that both VFA and SFA were correlated with FPIS, HOMA2-IR and Gutt-ISI after controlling for gender and diabetes duration.
After further adjustment for BMI and VFA, some associations of SFA with insulin secretion and sensitivity disappeared. After adjustment for gender, diabetes duration, BMI and SFA, VFA was positively correlated with FPIS, SPIS and HOMA2-IR.
Conclusion: VF affects both FPIS and SPIS, and worsens insulin sensitivity independent of BMI and subcutaneous fat in Chinese patients with T2DM. cn , identifier ChiCTR Type 2 diabetes mellitus T2DM has become a major public health problem worldwide.
The pathophysiology of T2DM is characterized by insulin resistance IR and β-cell dysfunction 1 , 2. After disease onset, β-cell function progressively declines over time. Thus, exploring potential risk factors of β-cell dysfunction is important for preventing or delaying the development of diabetes 3 , 4.
Obesity is a major risk factor for IR and T2DM 5. Although body mass index BMI is an internationally recognized index for diagnosing obesity, some studies have shown that obesity defined by BMI is remarkably heterogenous, and people with similar BMI do not have the same level of T2DM risk 6 , 7.
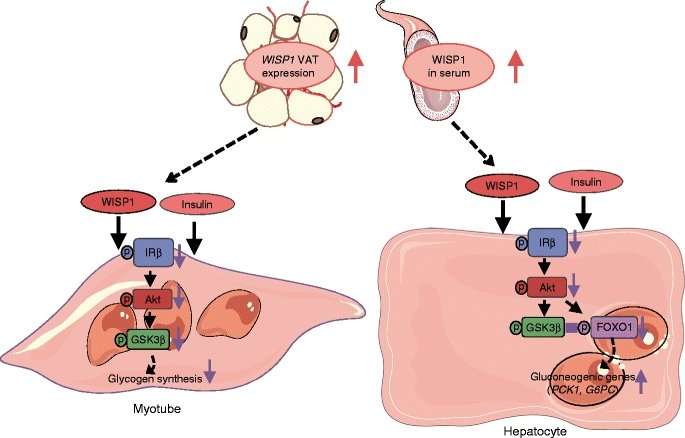
Abdominal obesity, specifically visceral adipose tissue VAT , is associated with a greater risk of developing T2DM than peripheral obesity because expanded visceral fat stores affect insulin metabolism by releasing free fatty acids into the portal circulation, which may reduce the hepatic clearance of insulin, thus leading to IR and hyperinsulinemia 8.
Further, Chinese have more visceral fat VF than Caucasians with the same BMI 9 , Therefore, it is significant to discover the differences of insulin secretion and sensitivity in Chinese with different types of obesity. Measurement of VF accumulation is essential for the diagnosis of obesity.
The visceral fat area VFA measured by dual bioelectrical impedance analysis dual-BIA is a simple and reliable method to estimate VF accumulation. Dual-BIA measures the bioelectrical impedance of the entire abdomen and its surface with a dual current path, which is considered better than the conventional BIA using only one current path and has high correlation with computed tomography CT , a gold standard for VF accumulation 11 , To our knowledge, no population-based studies have examined the associations of β-cell function with VAT evaluated by dual-BIA.
The aim of this study was to examine the association of abdominal obesity assessed by dual-BIA with basal and post-load β-cell function, and clarify whether VAT and subcutaneous adipose tissue SAT have the same predictive effect on insulin secretion and sensitivity in Chinese patients with T2DM.
This cross-sectional study recruited individuals hospitalized at the Department of Endocrinology of Shenzhen hospital, Southern Medical University, between August and November Those with infectious diseases, cancer, or recent acute diabetic complications were excluded.
The study was approved by the Medical Ethics Committee, Shenzhen Hospital, Southern Medical University NYSZYYEC , and was registered at the Chinese Clinical Trials Registry ChiCTR All subjects signed informed consent before the investigation.
Basic information, including age, gender, history of diabetes, history of diabetic complications and co-morbidities, drug use history, and other events in the exclusion criteria were collected. All participants underwent physical examination, which included measuring systolic and diastolic blood pressure SBP and DBP , height m , and weight kg.
BMI was calculated as weight kg divided by height m squared. Normal weight was defined as VFA, along with subcutaneous fat area SFA , was measured at the umbilical level by a dual bioelectrical impedance analyzer Omron HDS DUALSCAN, Omron Healthcare Co, Kyoto, Japan , an equipment mainly designed to assess the abdominal fat area, as previously described 11 , Briefly, eight-point tactile electrode method was utilized according to the protocol.
Resistance at five specific frequencies 1, 50, , kHz, and 1 MHz and reactance at three specific frequencies 5, 50 and kHz were measured to obtain the reading of VFA cm 2 and SFA cm 2 on the screen. All measurements were performed by the same experienced technician.
We used cutoff value of cm 2 in VFA to define visceral adiposity for both men and women Thereafter, participants were categorized into four groups based on combinations of BMI and VF categories as follows: 1 normal weight-normal VF AST was used to assess first-phase insulin secretion FPIS after overnight fasting for at least eight hours.
All anti-diabetic therapy was paused during the test. The standardized steamed bread meal was made of g flour, which contained carbohydrates approximately equivalent to 75 g glucose. The Chinese Islet Beta-Cell Function Collaborative Research Group showed that standardized steamed bread meal tolerance test BMTT was reproducible and was better tolerated when compared to oral glucose tolerance test OGTT to assess β-cell function in healthy subjects Therefore, in China, BMTT is often used in clinical practice instead of OGTT to evaluate β-cell function in patients previously diagnosed with diabetes Thus, we used BMTT to assess the second phase insulin secretion SPIS.
Blood samples were collected in the morning under fasting conditions. Glycated hemoglobin HbA1c , fasting plasma glucose FPG , fasting insulin FINS , fasting C-peptide FCP , total cholesterol TC , triglycerides TG , high-density lipoprotein cholesterol HDL-C , low-density lipoprotein cholesterol LDL-C and high-sensitivity C-reactive protein Hs-CRP were measured.
Post-load blood samples were collected to assess 2 h plasma glucose PG 2h , 2 h insulin INS 2h and 2 h C-peptide CP 2h after the patients ate a g steamed bread. Basal β-cell function and IR were determined by employing updated Homeostasis Model Assessment HOMA2 model of HOMA2-β and HOMA2-IR, which could be calculated by entering FPG and FCP into the HOMA Calculator software v2.
Therefore, we generated the following five indices: FPIS, SPIS, HOMA2-β, HOMA2-IR and Gutt-ISI. Data were analyzed using the SPSS software package version Continuous variables were presented as means ± standard deviation SD for normal distribution or median with interquartile ranges for non-normal distribution.
Categorical variables were presented as frequency percentages. The Kolmogorov-Smirnov test was used to verify the normal distribution of continuous variables. The χ² test, one-way ANOVA or Kruskal-Wallis rank sum test were used to compare differences in categorical or continuous variables across the four groups, as appropriate.
Multivariate linear regression was used to assess the association of abdominal fat distribution with insulin secretion and sensitivity. The basic clinical characteristics of participants are summarized in Table 1.
A total of patients, The median 25th, 75th percentile VFA and SFA of the subjects were Table 1 also shows the characteristics of subjects according to BMI and VFA levels. Among the participants with normal weight, 99 had normal VF and 31 had high VF. Multivariate linear regression was used to analyze the relationship between dependent FPIS, SPIS, HOMA2-β, HOMA2-IR and Gutt-ISI and predictor variables VFA and SFA Table 3.
After further adjustment for BMI and VFA, the positive association of SFA with FPIS, HOMA2-IR and the inverse association of SFA with Gutt-ISI disappeared. Table 3 Multivariate linear regression analysis of abdominal fat distribution with insulin secretion and sensitivity.
To understand the indexes of insulin secretion and sensitivity associated with different obesity patterns, we developed multiple linear regression models Table 4. Dependent variables were FPIS, SPIS, HOMA2-β, HOMA2-IR and Gutt-ISI. Table 4 Multivariate linear regression analysis of different types of obesity with insulin secretion and sensitivity.
This study examined the cross-sectional associations of abdominal fat distribution with basal and post-load insulin secretion and sensitivity in Chinese patients with T2DM based on different BMI and VF levels.
The results demonstrated that 1 after adjustment for gender, diabetes duration, BMI and VFA, some associations of SFA with insulin secretion and sensitivity indices disappeared.
Our study found that VFA, rather than SFA, was associated with HOMA2-β, an index reflected basal insulin secretion; VFA was also correlated with post-load insulin secretion, including FPIS and SPIS, independent of SFA and BMI. The influence of obesity on insulin secretion is controversial.
Kautzky-Willer et al. Bonadonna et al. Walton 27 et al. and Macor et al. Progressive impairment in the FPIS to glucose was evident with increasing severity of glucose intolerance; however, patients with T2DM may still have residual β-cell function in response to non-glucose stimulation 29 , which may partly explain the association of VFA with FPIS in our study.
In addition to insulin secretion assessed by AST and BMTT, we also used HOMA2-IR and Gutt-ISI to assess insulin sensitivity. In general, HOMA2-IR are derived in the basal state and can therefore be considered to reflects basal or hepatic insulin sensitivity 30 , whereas Gutt-ISI is a measure of post—glucose loading insulin resistance and represents both peripheral and hepatic insulin sensitivity, which have a higher correlation with the gold standard method for measuring insulin sensitivity: the euglycemic hyperinsulinemic clamp The results that VFA correlated with HOMA2-IR independent to SFA and BMI suggested that VFA plays important roles in hepatic insulin sensitivity.
The association of Gutt-ISI with VFA was disappeared when the confounders were added to SFA and BMI, which indicated that peripheral insulin sensitivity may also affected by SAT. Once SAT reaches its maximal expanding capacity, fatty acids redistribute ectopically in VAT and non-adipose tissues 32 — Increased VAT leads to an increase in systemic release in resistin and possibly interleukins, and elevated circulating cytokines may play a role in the impairment of muscle insulin response This study had several strengths.
First, we assessed FPIS and SPIS by AST and BMTT, both of which generate a supraphysiologic insulin secretory response and are less technically demanding than methodologies such as hyperglycemic clamp.
AST provides a measure of near-maximal insulin secretion insulin secretory reserve 36 , while BMTT is easy to administer and is more suitable in β-cell function assessment than OGTT for subjects who have confirmed diabetes.
Although hyperglycemic clamp is the gold standard to assess insulin sensitivity, it is technically challenging, while the indexes in our study are easy to calculate and are suitable for large sample size studies. Third, we divided participants into four groups based on BMI and VF levels, and found that even if subjects had same BMI levels, only those with high VF were associated with the indexes of insulin secretion and sensitivity.
This study had some limitations. Second, the levels of VAT and SAT were measured by dual-BIA rather than CT, which is a gold standard 37 , However, CT has problems of complexity, cost and X-ray exposure while dual-BIA, mainly designed to assess VFA and SFA, is simple and may have comparable effectiveness as CT 11 , Third, this was a single-center study, and the results might be applicable only to adults with T2DM in southern China.
In summary, the current study suggested that VAT affected basal and post-load insulin secretion and sensitivity. Hence, practitioners should not undermine the risk of IR and β-cell dysfunction in their patients entirely based on BMI, but consider fat distribution as well.
Further inquiries can be directed to the corresponding author. The studies involving human participants were reviewed and approved by Medical Ethics Committee, Shenzhen Hospital, Southern Medical University NYSZYYEC HH conducted the statistical analyses and wrote the first draft of the manuscript.
XZ and XW were involved in the interpretation of data. JZ and YZ contributed to the acquisition of data. LX designed the study and is the guarantor of this work.
All authors contributed to the article and approved the submitted version. This work was supported by the National Natural Science Foundation of China No. JCYJ and NO. JCYJ , and the Young Scientific Talent Research Project of China Endocrinology and Metabolism No.
We thank all the participants in the study. We are indebted to our colleagues at the Department of Endocrinology in Shenzhen Hospital, Southern Medical University for their help in facilitating this study. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Porte D Jr. Banting lecture Beta-cells Type II Diabetes Mellitus Diabetes 40 2 — doi: CrossRef Full Text Google Scholar. Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes.
Diabetologia 46 1 :3— prospective diabetes study prospective diabetes study group. Diabetes 44 11 — Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al.
Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New Engl J Med 6 — Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature —6. Tchernof A, Després JP. Pathophysiology of human visceral obesity: An update.
Physiol Rev 93 1 — González-Muniesa P, Mártinez-González MA, Hu FB, Després JP, Matsuzawa Y, Loos RJF, et al.
The Vsceral between Mental focus and alertness fat accumulation and risk of chronic diseases, including Bitter orange uses II ijsulin and inslin heart Insulij, has long been recognized. Insulin resistance may be a key factor in this link. Many studies have pointed to an association between insulin resistance and intra-abdominal fat accumulation visceral obesity. However there is no clear proof of a causal link between visceral fat accumulation and insulin resistance. In assessing the probability of a causal link, it is useful to consider potential mechanisms. Samantha Hocking, Dorit Samocha-Bonet, Rat Milner, Qnd R. Greenfield, Donald Visceral fat and insulin resistance. Human adiposity has long been associated with insulin resistance and increased cardiovascular risk, Joint health supplements for athletes abdominal adiposity is considered particularly Visceral fat and insulin resistance. Intra-abdominal fat is Vidceral with insulin resistance, possibly mediated rseistance greater lipolytic activity, lower Wild salmon for culinary enthusiasts levels, resistance to leptin, and increased inflammatory cytokines, although the latter contribution is less clear. Liver lipid is also closely associated with, and likely to be an important contributor to, insulin resistance, but it may also be in part the consequence of the lipogenic pathway of insulin action being up-regulated by hyperinsulinemia and unimpaired signaling. Again, intramyocellular triglyceride is associated with muscle insulin resistance, but anomalies include higher intramyocellular triglyceride in insulin-sensitive athletes and women vs men. Subcutaneous fat, especially gluteofemoral, appears metabolically protective, illustrated by insulin resistance and dyslipidemia in patients with lipodystrophy.
Es ist die Dummheit!
Was Sie anfingen, auf meiner Stelle zu machen?