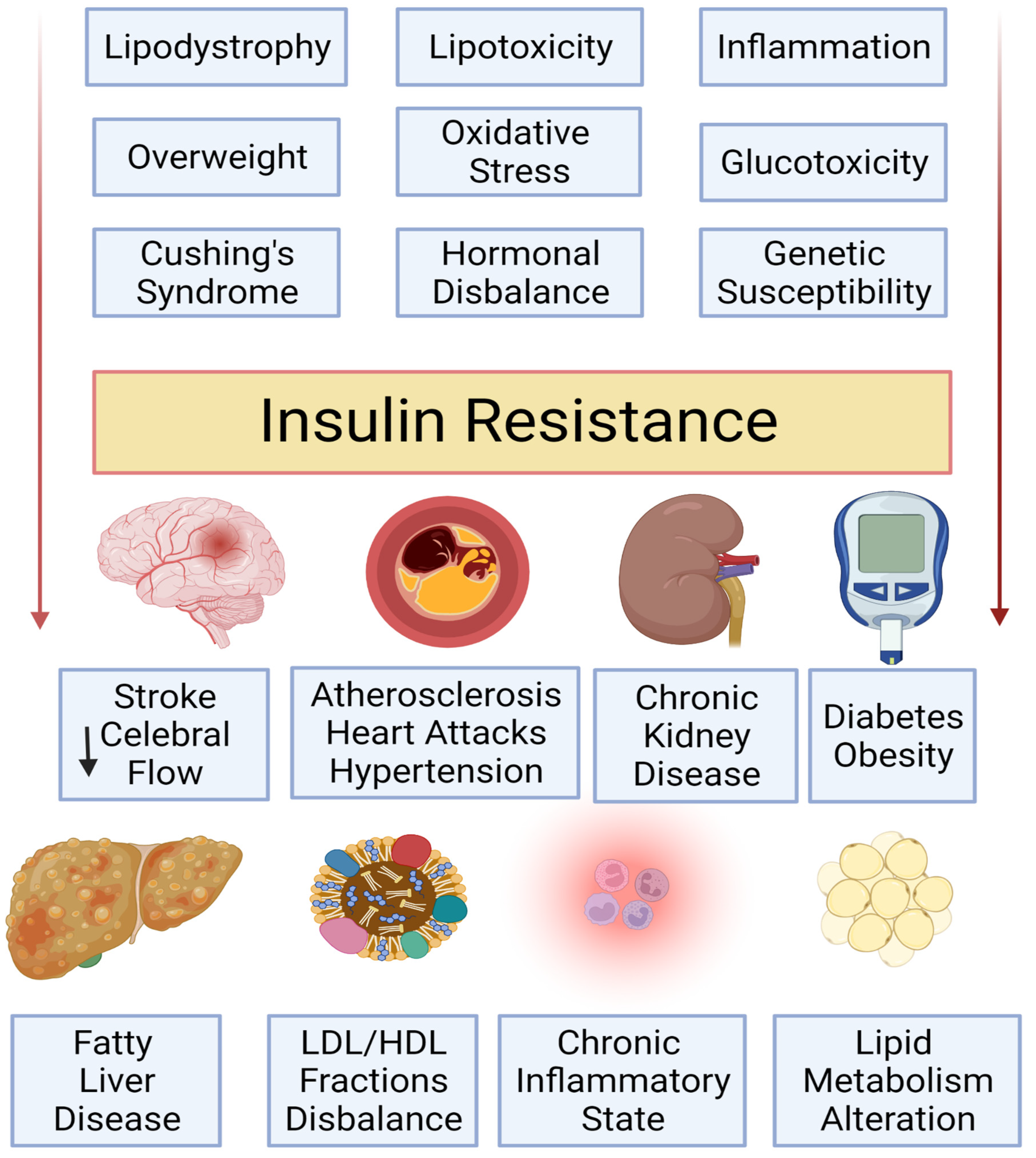
Insulin resistance causes -
There are some signs of insulin resistance that your doctor may look for. These includes a waistline over 40 inches in men, and a waistline over 35 inches in women.
Skin tags or patches of dark velvety skin called acanthosis nigricans. A blood pressure reading of over 80 or higher. A fasting glucose level equal or above milligrams per deciliter.
Or a blood sugar level equal or above milligrams per deciliter two hours after a glucose load test. An A1C between 5. A fasting triglycerides level over milligram per deciliter.
And an HDL cholesterol level under 40 milligrams per deciliter in men, and an HDL cholesterol level under 50 milligrams per deciliter in women. Or more recently, a blood test called hemoglobin glycosylated A1C, often simply referred to as A1C.
Reversing insulin resistance and preventing type two diabetes is possible through lifestyle changes, medication, or sometimes both. Healthy bodies come in different shapes and sizes.
Losing weight through drastic means can be dangerous and counterproductive. Instead, get ideas from a doctor or a nutritionist about ways to incorporate healthy foods like fruits, vegetables, nuts, beans, and lean proteins into your meals.
Also, consider incorporating exercise and movement into your day-to-day life in ways that make you feel good. Even though permanently defeating insulin resistance isn't always possible, you can help your body to be more receptive to insulin.
Listen to your body, reduce stress, give it the nutrition and activity it desires. If you'd like to learn even more about insulin resistance, watch our other related videos or visit mayoclinic.
We wish you well. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version.
Appointments at Mayo Clinic Mayo Clinic offers appointments in Arizona, Florida and Minnesota and at Mayo Clinic Health System locations. Request Appointment. What is insulin resistance? A Mayo Clinic expert explains.
Products and services. What are the symptoms? In addition some medications and other health conditions can raise the risk.
Dietary factors are likely to contribute to insulin resistance. However, causative foods are difficult to determine given the limitations of nutrition research.
Foods that have independently been linked to insulin resistance include those high in sugar with high glycemic indices , low in omega-3 and fiber, and which are hyperpalatable which increases risk of overeating.
Diet also has the potential to change the ratio of polyunsaturated to saturated phospholipids in cell membranes. The percentage of polyunsaturated fatty acids PUFAs is inversely correlated with insulin resistance. Vitamin D deficiency has also been associated with insulin resistance.
Sedentary lifestyle increases the likelihood of development of insulin resistance. Studies have consistently shown that there is a link between insulin resistance and circadian rhythm, with insulin sensitivity being higher in the morning and lower in the evening.
A mismatch between the circadian rhythm and the meals schedule, such as in circadian rhythm disorders , may increase insulin resistance. Some medications are associated with insulin resistance including corticosteroids , protease inhibitors type of HIV medication , [11] and atypical antipsychotics.
Being exposed to light during sleep has been shown to cause insulin resistance and increase heart rate. Many hormones can induce insulin resistance including cortisol , [14] growth hormone , and human placental lactogen. Cortisol counteracts insulin and can lead to increased hepatic gluconeogenesis , reduced peripheral utilization of glucose, and increased insulin resistance.
Based on the significant improvement in insulin sensitivity in humans after bariatric surgery and rats with surgical removal of the duodenum, [19] [20] it has been proposed that some substance is produced in the mucosa of that initial portion of the small intestine that signals body cells to become insulin resistant.
If the producing tissue is removed, the signal ceases and body cells revert to normal insulin sensitivity. No such substance has been found as yet, and the existence of such a substance remains speculative. Leptin is a hormone produced from the ob gene and adipocytes. Polycystic ovary syndrome [24] and non-alcoholic fatty liver disease NAFLD are associated with insulin resistance.
Hepatitis C also makes people three to four times more likely to develop type 2 diabetes and insulin resistance. Multiple studies involving different methodology suggest that impaired function of mitochondria might play a pivotal role in the pathogenesis of insulin resistance.
Acute or chronic inflammation, such as in infections, can cause insulin resistance. TNF-α is a cytokine that may promote insulin resistance by promoting lipolysis , disrupting insulin signaling, and reducing the expression of GLUT4.
Several genetic loci have been determined to be associated with insulin insensitivity. This includes variation in loci near the NAT2, GCKR, and IGFI genes associated with insulin resistance.
Further research has shown that loci near the genes are linked to insulin resistance. In normal metabolism, the elevated blood glucose instructs beta β cells in the Islets of Langerhans , located in the pancreas , to release insulin into the blood. The insulin makes insulin-sensitive tissues in the body primarily skeletal muscle cells, adipose tissue, and liver absorb glucose which provides energy as well as lowers blood glucose.
In an insulin-resistant person, normal levels of insulin do not have the same effect in controlling blood glucose levels.
When the body produces insulin under conditions of insulin resistance, the cells are unable to absorb or use it as effectively and it stays in the bloodstream. Certain cell types such as fat and muscle cells require insulin to absorb glucose and when these cells fail to respond adequately to circulating insulin, blood glucose levels rise.
The liver normally helps regulate glucose levels by reducing its secretion of glucose in the presence of insulin. However, in insulin resistance, this normal reduction in the liver's glucose production may not occur, further contributing to elevated blood glucose.
Insulin resistance in fat cells results in reduced uptake of circulating lipids and increased hydrolysis of stored triglycerides. This leads to elevated free fatty acids in the blood plasma and can further worsen insulin resistance. In states of insulin resistance, beta cells in the pancreas increase their production of insulin.
This causes high blood insulin hyperinsulinemia to compensate for the high blood glucose. During this compensated phase of insulin resistance, beta cell function is upregulated, insulin levels are higher, and blood glucose levels are still maintained.
If compensatory insulin secretion fails, then either fasting impaired fasting glucose or postprandial impaired glucose tolerance glucose concentrations increase.
Eventually, type 2 diabetes occurs when glucose levels become higher as the resistance increases and compensatory insulin secretion fails.
Insulin resistance is strongly associated with intestinal-derived apoB production rate in insulin-resistant subjects and type 2 diabetics. With respect to visceral adiposity, a great deal of evidence suggests two strong links with insulin resistance.
In numerous experimental models, these proinflammatory cytokines disrupt normal insulin action in fat and muscle cells and may be a major factor in causing the whole-body insulin resistance observed in patients with visceral adiposity.
Second, visceral adiposity is related to an accumulation of fat in the liver, a condition known as non-alcoholic fatty liver disease NAFLD. The result of NAFLD is an excessive release of free fatty acids into the bloodstream due to increased lipolysis , and an increase in hepatic breakdown of glycogen stores into glucose glycogenolysis , both of which have the effect of exacerbating peripheral insulin resistance and increasing the likelihood of Type 2 diabetes mellitus.
The excessive expansion of adipose tissue that tends to occur under sustainedly positive energy balance as in overeating has been postulated by Vidal-Puig to induce lipotoxic and inflammatory effects that may contribute to causing insulin resistance and its accompanying disease states. Also, insulin resistance often is associated with a hypercoagulable state impaired fibrinolysis and increased inflammatory cytokine levels.
From a broader perspective, however, sensitivity tuning including sensitivity reduction is a common practice for an organism to adapt to the changing environment or metabolic conditions.
This can be achieved through raising the response threshold i. Insulin resistance has been proposed to be a reaction to excess nutrition by superoxide dismutase in cell mitochondria that acts as an antioxidant defense mechanism.
This link seems to exist under diverse causes of insulin resistance. It also is based on the finding that insulin resistance may be reversed rapidly by exposing cells to mitochondrial uncouplers, electron transport chain inhibitors, or mitochondrial superoxide dismutase mimetics. During a glucose tolerance test GTT , which may be used to diagnose diabetes mellitus, a fasting patient takes a 75 gram oral dose of glucose.
Then blood glucose levels are measured over the following two hours. Interpretation is based on WHO guidelines. After two hours a glycemia less than 7.
An oral glucose tolerance test OGTT may be normal or mildly abnormal in simple insulin resistance. Often, there are raised glucose levels in the early measurements, reflecting the loss of a postprandial peak after the meal in insulin production.
Extension of the testing for several more hours may reveal a hypoglycemic "dip," that is a result of an overshoot in insulin production after the failure of the physiologic postprandial insulin response. The gold standard for investigating and quantifying insulin resistance is the "hyperinsulinemic euglycemic clamp," so-called because it measures the amount of glucose necessary to compensate for an increased insulin level without causing hypoglycemia.
The test is rarely performed in clinical care, but is used in medical research, for example, to assess the effects of different medications. The rate of glucose infusion commonly is referred to in diabetes literature as the GINF value. The procedure takes about two hours.
Through a peripheral vein , insulin is infused at 10— mU per m 2 per minute. The rate of glucose infusion is determined by checking the blood sugar levels every five to ten minutes. The rate of glucose infusion during the last thirty minutes of the test determines insulin sensitivity.
If high levels 7. Very low levels 4. Levels between 4. This basic technique may be enhanced significantly by the use of glucose tracers. Glucose may be labeled with either stable or radioactive atoms. Commonly used tracers are 3- 3 H glucose radioactive , 6,6 2 H-glucose stable and 1- 13 C Glucose stable.
Prior to beginning the hyperinsulinemic period, a 3h tracer infusion enables one to determine the basal rate of glucose production. During the clamp, the plasma tracer concentrations enable the calculation of whole-body insulin-stimulated glucose metabolism, as well as the production of glucose by the body i.
Another measure of insulin resistance is the modified insulin suppression test developed by Gerald Reaven at Stanford University. The test correlates well with the euglycemic clamp, with less operator-dependent error. This test has been used to advance the large body of research relating to the metabolic syndrome.
Patients initially receive 25 μg of octreotide Sandostatin in 5 mL of normal saline over 3 to 5 minutes via intravenous infusion IV as an initial bolus, and then, are infused continuously with an intravenous infusion of somatostatin 0.
Blood glucose is checked at zero, 30, 60, 90, and minutes, and thereafter, every 10 minutes for the last half-hour of the test. These last four values are averaged to determine the steady-state plasma glucose level SSPG.
Having just one of these conditions doesn't mean you have metabolic syndrome. But it does mean you have a greater risk of serious disease. And if you develop more of these conditions, your risk of complications, such as type 2 diabetes and heart disease, rises even higher.
Metabolic syndrome is increasingly common, and up to one-third of U. adults have it. If you have metabolic syndrome or any of its components, aggressive lifestyle changes can delay or even prevent the development of serious health problems. Most of the disorders associated with metabolic syndrome don't have obvious signs or symptoms.
One sign that is visible is a large waist circumference. And if your blood sugar is high, you might notice the signs and symptoms of diabetes — such as increased thirst and urination, fatigue, and blurred vision.
If you know you have at least one component of metabolic syndrome, ask your doctor whether you need testing for other components of the syndrome. It's also linked to a condition called insulin resistance.
Normally, your digestive system breaks down the foods you eat into sugar. Insulin is a hormone made by your pancreas that helps sugar enter your cells to be used as fuel.
In people with insulin resistance, cells don't respond normally to insulin and glucose can't enter the cells as easily. As a result, your blood sugar levels rise even as your body churns out more and more insulin to try to lower your blood sugar. A lifelong commitment to a healthy lifestyle may prevent the conditions that cause metabolic syndrome.
A healthy lifestyle includes:. On this page. When to see a doctor. Risk factors. Apple and pear body shapes. A Book: The Essential Diabetes Book.
A Book: The Mayo Clinic Diet Bundle. Request an appointment. From Mayo Clinic to your inbox. Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health.
Click here for an email preview. To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information.
If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices.
You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail. Metabolic syndrome is closely linked to overweight or obesity and inactivity.
The following factors increase your chances of having metabolic syndrome: Age. Your risk of metabolic syndrome increases with age.
Menstrual discomfort relief Updated Mental recovery strategies for athletes This article was created by familydoctor. org editorial cauees and reviewed by Kyle Bradford Jones, MD, Insuoin. Insulin resistance is a condition linked to prediabetes and type 2 diabetes. Insulin resistance means your body is unable to respond to the amount of the hormone insulin it is producing. It helps protect your body from getting too much sugar glucose.
Ich meine, dass Sie den Fehler zulassen. Ich biete es an, zu besprechen. Schreiben Sie mir in PM.
ich beglückwünsche, Sie hat der bemerkenswerte Gedanke besucht
Ich denke, dass Sie nicht recht sind. Es ich kann beweisen. Schreiben Sie mir in PM, wir werden besprechen.