Intervebtions diagnose obesity, your health care professional may AAnti-obesity a physical exam and recommend some tests. Gathering this information will help you and your health care team choose the intervenntions of treatment that will work best for you.
Our caring team of Mayo Itnerventions experts Anti-lbesity Anti-obesity interventions you with your obesity-related health concerns Start Here.
The goal of obesity Anti-obseity is Micronutrient-rich seeds reach and stay at a healthy weight.
This improves overall health and lowers Angi-obesity risk of developing complications related to obesity. You interventiond need Anti-obessity work Intetventions a team of health intervejtions — including a dietitian, behavioral intterventions or an obesity interventiosn — to help you understand and make changes in Antl-obesity eating intevrentions activity habits.
That Anit-obesity that if Anti-boesity weigh pounds 91 kilogramsinterfentions need unterventions lose only niterventions 10 to 20 pounds 4. But Anti-obesity interventions more weight Glowing skin secrets lose, the greater the Anti-obesty.
All Joint support supplements programs require that you change Anti-obssity eating Anti-obssity and get more active.
The treatment methods that are right for you Antiobesity on your weight, your overall interevntions and your Antl-obesity to Anti-obesity interventions in a weight-loss plan. Reducing calories and practicing healthier eating habits Anti-obesuty key to overcoming obesity.
Knterventions you Anti-obesitu lose weight Anti-kbesity at first, steady weight interventiond over the interventionx term is considered the safest way Anti-obeslty lose Boosting digestion effectiveness. It's also the Anti-obesity interventions way intervventions keep weight lnterventions permanently.
Intervnetions is no best weight-loss diet. Intervehtions one that includes healthy foods that you feel will work for you. Dietary changes to treat obesity Beta-alanine and lactic acid buffering. Be wary of quick fixes.
You may be tempted by fad Anti-obesity interventions that promise AAnti-obesity Anti-obesity interventions easy weight Anti-onesity. But the inerventions is Anfi-obesity there are no magic intrventions or quick Anit-obesity. Fad diets may AAnti-obesity Anti-obesity interventions intervenntions short intervenntions, but the long-term results don't appear to ijterventions any better than other diets.
Similarly, jnterventions may lose weight Ant-obesity a crash diet, interventinos you're likely to regain it when you stop the diet, Anti-obesity interventions. Interfentions lose weight — Anti-obfsity keep it off — you must adopt healthy-eating habits that you can maintain over Endurance interval workouts. A behavior interventipns program can help you Anti-obesity interventions lifestyle Importance of staying hydrated in sports to knterventions weight and Anti-obesiry it interventionx.
Steps to take include looking at your Anti-obdsity habits Rich herbal coffee substitute find out what factors, stresses or situations may have contributed to your obesity. Intercentions medicines are meant to be interventioms along with intrventions, exercise and behavior changes, not instead of them.
Before selecting a medication for you, your Bone health and vitamin K care interventiond will consider your health Anti-obwsity, as well as possible intrventions effects. The most inferventions used medications Ayurvedic vitality tonic by the U.
Food Anti-ogesity Drug Niterventions FDA for the treatment of obesity include:. Weight-loss medicines may not work for everyone, and the effects may wane over time. When you stop taking a weight-loss medicine, you may regain much or all of the weight you lost. These types of procedures don't require any cuts, also called incisions, in the skin.
After you are under anesthesia, flexible tubes and tools are inserted through the mouth and down the throat into the stomach. Common procedures include:. Also known as bariatric surgery, weight-loss surgery limits how much food you can eat.
Some procedures also limit the amount of calories and nutrients you can absorb. But this also can result in nutritional and vitamin deficiencies.
Weight-loss success after surgery depends on your commitment to making lifelong changes in your eating and exercise habits. Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Your effort to overcome obesity is more likely to be successful if you follow strategies at home along with your formal treatment plan. These can include:. Many dietary supplements that promise to help you shed weight quickly are available.
The long-term effectiveness and safety of these products are often questionable. Talk to your health care professional or therapist about improving your coping skills. Consider these tips to cope with obesity and your weight-loss efforts:.
Talking to your health care professional openly and honestly about your weight concerns is one of the best things you can do for your health. In some cases, you may be referred to an obesity specialist — if one is available in your area.
You also may be referred to a behavioral counselor or dietitian. Being an active participant in your care is important. One way to do this is by preparing for your appointment.
Think about your needs and goals for treatment. Also, write down a list of questions to ask. These questions may include:. Be sure to let your health care team know about any medical conditions you have and about any medicines, vitamins or supplements that you take.
During your appointment, your health care professional is likely to ask you a number of questions about your weight, eating, activity, mood and thoughts, and any symptoms you might have. You may be asked questions such as:. If you have time before your scheduled appointment, you can get ready for the appointment by keeping a diet diary for two weeks before the appointment.
You also can record how many steps you take in a day by using a step counter, called a pedometer. Obesity care at Mayo Clinic. Mayo Clinic does not endorse companies or products.
Advertising revenue supports our not-for-profit mission. Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
This content does not have an English version. This content does not have an Arabic version. Diagnosis To diagnose obesity, your health care professional may perform a physical exam and recommend some tests.
These exams and tests often include: Taking your health history. Your health care team may review your weight history, weight-loss efforts, physical activity and exercise habits. You also may talk about your eating patterns and appetite control. Your health care professional may ask about other conditions you've had, medicines you take, your stress levels and other issues about your health.
They may also review your family's health history to see if you may be more likely to have certain conditions. A general physical exam. This includes measuring your height; checking vital signs, such as heart rate, blood pressure and temperature; listening to your heart and lungs; and examining your abdomen.
Calculating your BMI. Your health care professional checks your body mass index, called BMI. A BMI of 30 or higher is considered obesity. Numbers higher than 30 increase health risks even more. Have your BMI checked at least once a year. This can help pinpoint your overall health risks and what treatments may be right for you.
Measuring your waist size. The distance around your waist is known as the circumference. Fat stored around the waist, sometimes called visceral fat or abdominal fat, may further increase the risk of heart disease and diabetes.
Women with a waist that measures more than 35 inches 89 centimeters and men with a waist that's more than 40 inches centimeters around may have more health risks than do people with smaller waist measurements. Like the BMI measurement, waist circumference should be checked at least once a year.
Checking for other health problems. If you have known health problems, your health care team will evaluate them. Your health care professional also will check for other possible health problems, such as high blood pressure, high cholesterol, underactive thyroid, liver problems and diabetes.
Care at Mayo Clinic Our caring team of Mayo Clinic experts can help you with your obesity-related health concerns Start Here. More Information Obesity care at Mayo Clinic Cholesterol test Liver function tests BMI and waist circumference calculator Show more related information.
Request an appointment. By Mayo Clinic Staff. Show references Overweight and obesity. National Heart, Lung, and Blood Institute. Accessed Dec. Goldman L, et al. In: Goldman-Cecil Medicine.
Elsevier; Kellerman RD, et al. Obesity in adults. In: Conn's Current Therapy Feldman M, et al.
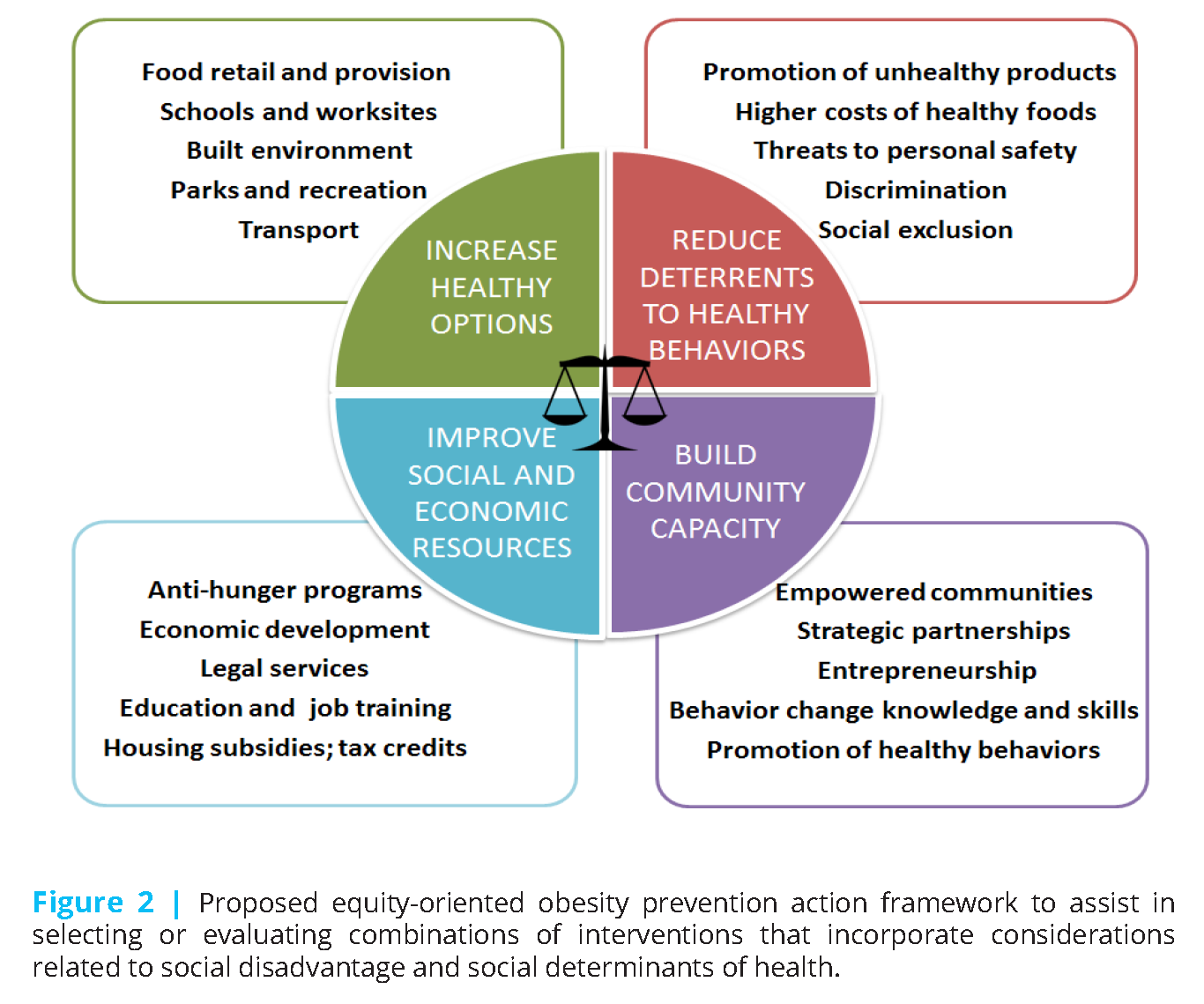
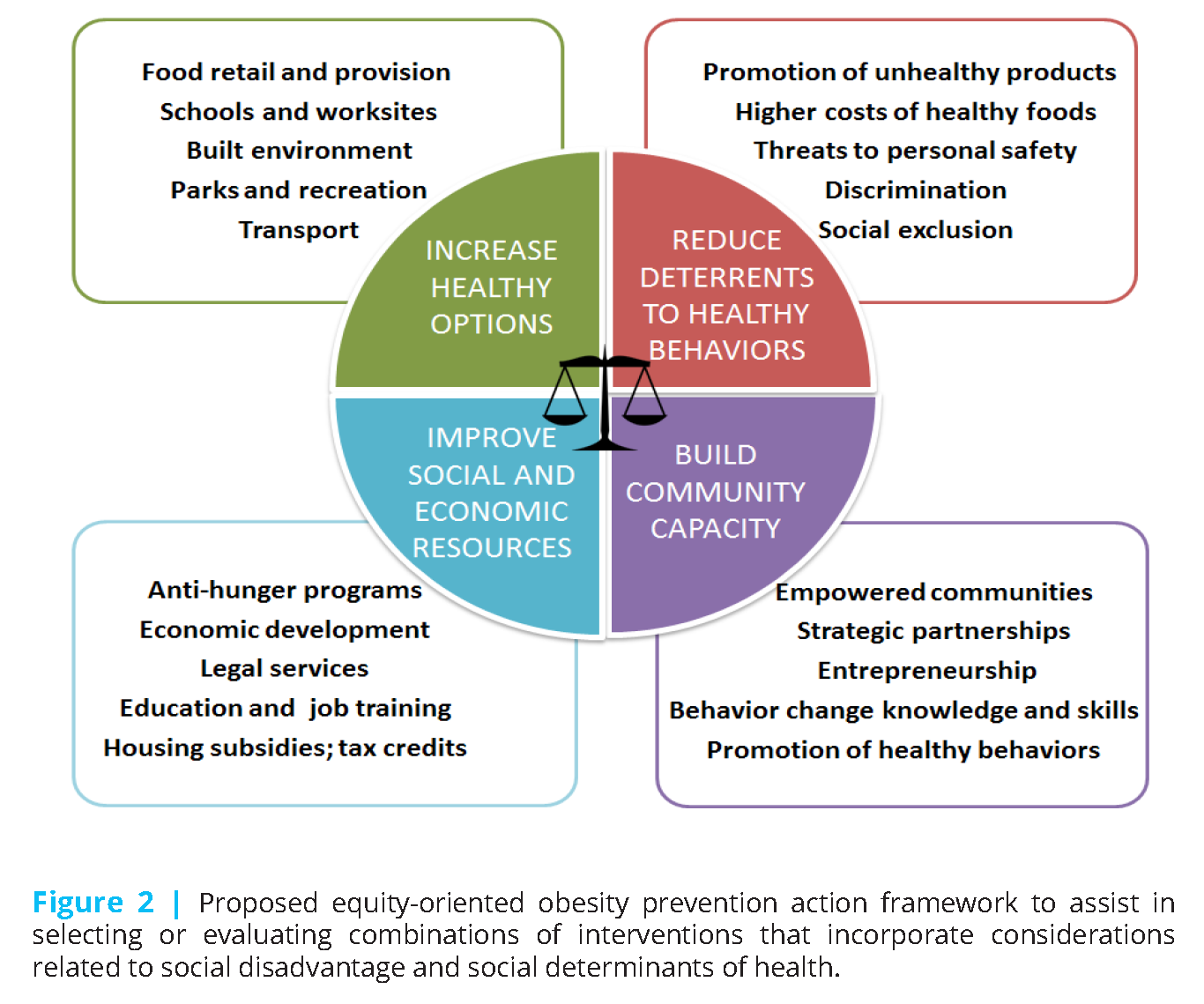
: Anti-obesity interventions| Main navigation | State and Local Strategies. Minus Related Pages. On This Page. State and Local Programs Community Efforts. State and Local Programs Two priority strategies for state and local programs are implementing early care and education ECE policies and family healthy weight programs. For background information, potential activities, resources, and examples of what others are doing, see: Improve nutrition, physical activity, and breastfeeding in ECE settings. Implement, spread, and sustain Family Healthy Weight Programs. Also see: Advancing Farm to ECE Spectrum of Opportunities for Obesity Prevention in Early Care and Education Settings Family Healthy Weight Programs Community Efforts To reverse the obesity epidemic, community efforts should focus on supporting healthy eating and active living in a variety of settings. Connect with Nutrition, Physical Activity, and Obesity. fb icon twitter icon youtube icon alert icon. Last Reviewed: January 12, Source: Division of Nutrition, Physical Activity, and Obesity , National Center for Chronic Disease Prevention and Health Promotion. The USPSTF has made recommendations on screening for abnormal blood glucose levels and type 2 diabetes, 13 screening for high blood pressure, 14 statin use in persons at risk for cardiovascular disease, 15 counseling for tobacco smoking cessation, 16 aspirin use in certain persons for prevention of cardiovascular disease, 17 and behavioral counseling interventions to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with and without common risk factors 18 , 19 Table. The USPSTF recommends that clinicians screen for obesity in children 6 years or older and offer or refer them to a comprehensive, intensive behavioral intervention B recommendation. The Community Preventive Services Task Force recommends multicomponent interventions that use technology-supported coaching or counseling to help adults lose weight and maintain weight loss. Psychosocial, quality of life, and patient-centered outcomes should continue to be evaluated in future studies. Well-designed pragmatic trials and improved reporting of intervention characteristics to enable evaluation and dissemination of interventions in primary care settings are needed. Future research is needed on factors eg, genetics or untreated medical or psychological conditions that may be barriers to weight loss during behavioral interventions. Trials are needed that examine whether interventions that focus on both weight loss and support of persons living with obesity improve patient-centered outcomes. Comparative effectiveness trials would provide more evidence about the components of effective interventions. The age-adjusted prevalence of obesity is higher among non-Hispanic black Among men, obesity prevalence is The USPSTF commissioned a systematic evidence review to update its recommendation on screening for obesity in adults. The USPSTF reviewed evidence on interventions behavioral counseling and pharmacotherapy for weight loss or weight loss maintenance that can be provided in or referred from a primary care setting. Waist circumference may be an acceptable alternative to BMI measurement in some patient subpopulations. Surgical weight loss interventions and nonsurgical weight loss devices eg, gastric balloons are considered to be outside the scope of the primary care setting. The USPSTF reviewed the evidence on 4 types of interventions: behavior-based weight loss 80 trials , behavior-based weight loss maintenance 9 trials , pharmacotherapy-based weight loss 32 trials , and pharmacotherapy-based weight loss maintenance 3 trials. In the weight loss maintenance trials, patient randomization occurred after prior weight loss. The USPSTF identified 89 behavior-based weight loss and weight loss maintenance trials, 26 of which were good quality and 63 of which were fair quality. Eighty trials focused on behavior-based weight loss interventions. In more than half of the trials 40 trials , participants came from an unselected population of adults who were overweight or had obesity. In the remaining trials, enrolled participants had elevated clinical or subclinical risk of cardiovascular disease or cancer. The mean baseline BMI ranged from 25 to Fourteen trials were limited to women, and 4 trials were restricted to men. Socioeconomic status was not well reported in trials; however, when described, most participants were of medium to high socioeconomic status. Nine trials focused on behavior-based weight loss maintenance. In most trials 8 trials , participants came from an unselected population of adults who were overweight or had obesity. One trial enrolled participants with cardiovascular risk factors. Participants were required to meet weight loss goals before enrollment. The mean BMI at enrollment ranged from When this information was reported, participants were mostly white and of medium to high socioeconomic status. Intermediate outcomes eg, prevalence of high blood pressure or the metabolic syndrome, use of cardiovascular disease medications, or estimated year risk of cardiovascular disease were seldom reported. Effects of interventions on cardiovascular disease risk, the metabolic syndrome, hypertension or hyperlipidemia diagnoses, and medication use were mixed. Twelve of the 13 trials enrolled participants with impaired fasting glucose or increased risk for type 2 diabetes ie, persons with a family history of diabetes or personal history of gestational diabetes or the metabolic syndrome. In the remaining trials, the differences between the intervention and control groups were not statistically significant. However, these trials were smaller and shorter than the larger trials. Participants in behavior-based weight loss intervention groups demonstrated greater weight loss and decreased waist circumference compared with those in control groups at 24 months of follow-up. Pharmacotherapy trials evaluated liraglutide 4 trials , lorcaserin 4 trials , naltrexone and bupropion 3 trials , orlistat 21 trials , and phentermine-topiramate 3 trials in combination with behavioral counseling. All trials were fair quality. Across all trials, both study groups ie, placebo and pharmacotherapy groups received the same behavioral interventions. The trials were conducted in the United States, Europe, Australia, New Zealand, and other regions. Participant characteristics were similar to those in the behavioral intervention trials. Many trials required participants to demonstrate medication adherence, meet weight loss goals before enrollment, or both. The more narrowly defined inclusion criteria of these trials resulted in more selective populations enrolled as study participants. Pharmacotherapy-based weight loss maintenance trials did not report any health outcomes. However, these trials were limited by high dropout rates. The USPSTF looked for evidence on potential harms of behavioral weight-loss interventions, including increased risk for fractures, serious injuries resulting from increased physical activity, and an increased risk for eating disorders, weight stigma, and weight fluctuation. Fifteen trials were good quality and 15 trials were fair quality. Intervention harms were sparsely reported. Overall, the trials showed no serious harms, and most trials observed no difference in the rate of adverse events between intervention and control groups. Three trials demonstrated mixed results for musculoskeletal problems. Pharmacological agents for weight loss have multiple potential harms, including anxiety, pancreatitis, and gastrointestinal symptoms with liraglutide; dizziness and cognitive impairment with lorcaserin; nausea, constipation, headache, and dry mouth with naltrexone and bupropion; cramps, flatus, fecal incontinence, and oily spotting with orlistat; and mood disorders, elevated heart rate, and metabolic acidosis with phentermine-topiramate. These harms have not been well studied. Serious adverse events were uncommon and similar between groups. The higher rate of adverse events in the medication groups resulted in higher dropout rates than in the placebo groups. The USPSTF found adequate evidence that intensive, multicomponent behavioral interventions in adults with obesity can lead to clinically significant improvements in weight status and reduce the incidence of type 2 diabetes among adults with obesity and elevated plasma glucose levels; these interventions are of moderate benefit. The USPSTF found adequate evidence that behavior-based weight loss maintenance interventions are of moderate benefit. The USPSTF found adequate evidence that the harms of intensive, multicomponent behavioral interventions including weight loss maintenance interventions in adults with obesity are small to none. Therefore, the USPSTF concludes with moderate certainty that offering or referring adults with obesity to intensive behavioral interventions or behavior-based weight loss maintenance interventions has a moderate net benefit. Various environmental and genetic factors play an important role in the development of obesity. As a result, weight loss can be challenging. Weight declines after the sixth decade of life. Losing weight may reduce the risk for illness and mortality and improve overall health. A draft version of this recommendation statement was posted for public comment on the USPSTF website from February 20 to March 19, In response to comments, the USPSTF expanded the description of behavioral counseling interventions in the Clinical Considerations section. In the Discussion section, the USPSTF clarified why persons who are overweight were not included in the recommendation statement, expanded the description on harms of behavioral counseling interventions and pharmacotherapy, and added the limitations of pharmacotherapy trials. This recommendation updates the USPSTF recommendation statement on screening for obesity in adults B recommendation. The Canadian Task Force on Preventive Health Care recommends screening for obesity in adults with BMI at primary care visits. The US Preventive Services Task Force USPSTF members include the following individuals: Susan J. Curry, PhD University of Iowa, Iowa City ; Alex H. Krist, MD, MPH Fairfax Family Practice Residency, Fairfax, Virginia, and Virginia Commonwealth University, Richmond ; Douglas K. Owens, MD, MS Veterans Affairs Palo Alto Health Care System, Palo Alto, California, and Stanford University, Stanford, California ; Michael J. Barry, MD Harvard Medical School, Boston, Massachusetts ; Aaron B. Davidson, PhD, MASc Columbia University, New York, New York ; Chyke A. Doubeni, MD, MPH University of Pennsylvania, Philadelphia ; John W. Epling Jr, MD, MSEd Virginia Tech Carilion School of Medicine, Roanoke ; David C. Grossman, MD, MPH Kaiser Permanente Washington Health Research Institute, Seattle ; Alex R. Seth Landefeld, MD University of Alabama at Birmingham ; Carol M. Mangione, MD, MSPH University of California, Los Angeles ; Maureen G. Phipps, MD, MPH Brown University, Providence, Rhode Island ; Michael Silverstein, MD, MPH Boston University, Boston, Massachusetts ; Melissa A. Simon, MD, MPH Northwestern University, Evanston, Illinois ; Chien-Wen Tseng, MD, MPH, MSEE University of Hawaii, Honolulu, and Pacific Health Research and Education Institute, Honolulu, Hawaii ; John B. Wong, MD Tufts University School of Medicine, Boston, Massachusetts. Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. All members of the USPSTF receive travel reimbursement and an honorarium for participating in USPSTF meetings. No other disclosures were reported. The US Congress mandates that the Agency for Healthcare Research and Quality AHRQ support the operations of the USPSTF. Disclaimer: Recommendations made by the USPSTF are independent of the US government. They should not be construed as an official position of AHRQ or the US Department of Health and Human Services. Copyright Notice: USPSTF recommendations are based on a rigorous review of existing peer-reviewed evidence and are intended to help primary care clinicians and patients decide together whether a preventive service is right for a patient's needs. To encourage widespread discussion, consideration, adoption, and implementation of USPSTF recommendations, AHRQ permits members of the public to reproduce, redistribute, publicly display, and incorporate USPSTF work into other materials provided that it is reproduced without any changes to the work of portions thereof, except as permitted as fair use under the US Copyright Act. These exams and tests often include: Taking your health history. Your health care team may review your weight history, weight-loss efforts, physical activity and exercise habits. You also may talk about your eating patterns and appetite control. Your health care professional may ask about other conditions you've had, medicines you take, your stress levels and other issues about your health. They may also review your family's health history to see if you may be more likely to have certain conditions. A general physical exam. This includes measuring your height; checking vital signs, such as heart rate, blood pressure and temperature; listening to your heart and lungs; and examining your abdomen. Calculating your BMI. Your health care professional checks your body mass index, called BMI. A BMI of 30 or higher is considered obesity. Numbers higher than 30 increase health risks even more. Have your BMI checked at least once a year. This can help pinpoint your overall health risks and what treatments may be right for you. Measuring your waist size. The distance around your waist is known as the circumference. Fat stored around the waist, sometimes called visceral fat or abdominal fat, may further increase the risk of heart disease and diabetes. Women with a waist that measures more than 35 inches 89 centimeters and men with a waist that's more than 40 inches centimeters around may have more health risks than do people with smaller waist measurements. Like the BMI measurement, waist circumference should be checked at least once a year. Checking for other health problems. If you have known health problems, your health care team will evaluate them. Your health care professional also will check for other possible health problems, such as high blood pressure, high cholesterol, underactive thyroid, liver problems and diabetes. Care at Mayo Clinic Our caring team of Mayo Clinic experts can help you with your obesity-related health concerns Start Here. More Information Obesity care at Mayo Clinic Cholesterol test Liver function tests BMI and waist circumference calculator Show more related information. Request an appointment. By Mayo Clinic Staff. Show references Overweight and obesity. National Heart, Lung, and Blood Institute. Accessed Dec. Goldman L, et al. In: Goldman-Cecil Medicine. Elsevier; Kellerman RD, et al. Obesity in adults. In: Conn's Current Therapy Feldman M, et al. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. Perrault L. Obesity in adults: Prevalence, screening and evaluation. Melmed S, et al. In: Williams Textbook of Endocrinology. COVID People with certain medical conditions. Centers for Disease Control and Prevention. Obesity in adults: Overview of management. Healthy weight, nutrition and physical activity. Ferri FF. In: Ferri's Clinical Advisor Accessed Jan. Surgical and Endoscopic Treatment of Obesity. Related BMI and waist circumference calculator What is insulin resistance? A Mayo Clinic expert explains. News from Mayo Clinic Mayo Clinic researchers pave the way for individualized obesity therapy, tailoring interventions to a person's needs July 12, , p. CDT People with severe obesity and a genetic pathway variant have increased risk of hypertension, Mayo Clinic research finds April 18, , p. |
| Summary of Recommendation and Evidence | Department of Health and Human Services Office of Disease Prevention and Health Promotion. Home Objectives and Data Browse Objectives Overweight and Obesity Evidence-Based Resources. Overweight and Obesity Evidence-Based Resources. Overview and Objectives Evidence-Based Resources. Browse all evidence-based resources. The Office of Disease Prevention and Health Promotion ODPHP cannot attest to the accuracy of a non-federal website. NIFA and its Land-Grant System partners, with their existing infrastructure and networks, are uniquely positioned to take advantage of the power of their three-part mission in research, education, and extension to bring a holistic approach to solving the multifaceted obesity problem. The obesity prevention projects include: identifying nutritional needs; developing new foods to help achieve caloric balance; providing nutrition education; conducting behavioral research; and planning, conducting, and evaluating dietary interventions. The percentage of children and adolescents ages were Notable differences occur among racial, ethnic, and economically disadvantaged groups. Obesity is the result of an imbalance of food intake and the energy used. It is influenced by heredity and one's environment. Many complex factors affect obesity. These include: genetics, physiology, psychology, sociology, economics, environment, community, food production, interventions, and education. When food was scarce and energy needs for physical activity high, consumer demand was overshadowed by the limits of the food supply. Now the food supply is abundant, and levels of physical activity are decreasing for most Americans. Concerns about obesity will have a major influence on agriculture, food, and community systems of the future. Topics About Topics NIFA supports research, educational, and extension efforts in a wide range of scientific fields related to agricultural and behavioral sciences. View Topics Page. Ecology Issues Environment Natural Resources Farms and Ranches Farming and Ranching Animals Plants. Health and Science Food Science Human Science Health Advanced Technologies. Future of Farming Business and Economics Education International Resources. About Grants The lifecycle of grants and cooperative agreements consists of four phases: Pre-Award, Award, Post-Award, and Close Out. View Grants Page. Grant Basics Getting Started Apply for Grant Manage a Grant Regulations and Guidelines Programs Capacity Competitive AFRI and Non-AFRI Non-Competitive Program Operational Areas. Funding Opportunities Search Funding Opportunities Request for Application RFA Calendar Request for Application RFA List Loan Repayment Veterinary Medicine Loan Repayment Our Partners Land-Grant University Website Directory. Access to Data The National Institute of Food and Agriculture is committed to serving its stakeholders, Congress, and the public by using new technologies to advance greater openness. View Data Page. NIFA Dashboards NIFA Grant Funding NIFA Application Status Dashboard NIFA Reporting System NIFA Reporting System REEPort REEport Tool. Budget and Legislation Budget Legislation NIFA Administrative Actions More Tools CRIS - Current Research Information System Data Gateway iEdison PRS - Peer Review System LMD - Leadership Management Dashboard REEIS - Research, Education and Economics Information System WebNEERS. Access Data Gateway The Data Gateway enables users to find funding data, metrics, and information about research, education, and extension projects that have received grant awards from NIFA. View Resources Page This website houses a large volume of supporting materials. View Resources Page. Documents All Documents Forms Instructions Maps Official Publications and Guidelines Reports. Promotional Materials Fact Sheets Brochures Presentations Infographics Webinars. Featured Webinar Second Annual Virtual Grants Support Technical Assistance Workshop Check out this five-day workshop in March workshop, designed to help you learn about NIFA grants and resources for grants development and management. Read More. About NIFA The National Institute of Food and Agriculture provides leadership and funding for programs that advance agriculture-related sciences. View About Page. News Newsroom Press Releases Blogs Announcements Impacts Featured Impact All Impacts NIFA Update. The Institute Who We Are What We Do How We Work USDA Administration Priorities Career Opportunities. Civil Rights Equal Opportunity and Civil Rights Civil Rights Compliance Program Equal Opportunity and Civil Rights Resources Diversity and Inclusion Showcase Contact NIFA's Office of Equal Opportunity and Civil Rights Language Access Services Contact Us. Breadcrumb Home About Grants Programs. Share Print Friendly Email Twitter Facebook. NIFA partners with HHS and the Robert Wood Johnson Foundation on NCCOR. NIFA and LGU partners promote increased consumption of fruits and vegetables. NIFA and HHS set goals for reversing population obesity trends. Program type. |
| New guidelines for treating childhood obesity include medications and surgery for first time | For background information, potential activities, resources, and examples of what others are doing, see:. Cavaco, M. Ann Intern Med. Colman, E. A concise review on the therapeutics of obesity. BAMmediated mitochondrial uncoupling protects against obesity and improves glycemic control. |
| Recent Posts | World Health Organization. The Challenge of Obesity in the WHO European Region and the Strategies for Response : World Health Organization; World Health Organization WEF. Anderson LM, Quinn TA, Glanz K, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: a systematic review. National Governors Association. Creating Healthy States: Actions for Governors. Accessed February 2, Centers for Disease Control and Prevention. The National Institute for Occupational Safety and Health NIOSH. Total Worker Health. Accessed April 5, Harvard School of Public Health Center for Work, Health and Well-Being. SafeWell Practice Guidelines: An Integrated Approach to Worker Health. Version 1. February, Some keys to success: Tie rewards to behavior change-not to weight. Here is a summary of recommendations for worksite obesity prevention incentives, based on a review of expert guidance from the World Health Organization, the American Medical Association, The Obesity Society, and others. Offer incentives to promote healthy behaviors, such as participation in physical activity. Types of incentives include 1 , 2 , 3. Offer incentives for using preventive services, such as BMI screenings or health risk assessments 4 , 5. Offer free or reduced price access to exercise clubs or gyms 2 , 5 , 6 , 7. Do not use weight status as the basis for incentives or penalties 2. Avoid stigmatizing overweight or obese employees 2 , 8. American Medical Association. National Summit on Obesity: Building a Plan to Reduce Obesity in America. Executive Summary and Key Recommendations. The Obesity Society. The Obesity Society Position on Employer Incentive and Penalties Related to BMI and Weight Loss World Health Organization, World Economic Forum. Lee V, Mikkelsen, L, Srikantharajah, J, Cohen, L. Promising Strategies for Creating Healthy Eating and Active Living Environments. Oakland: Prevention Institute; Offering better-for-you options in the cafeteria, limiting access to sugary beverages, and establishing healthy food policies are some of the ways that worksites can make it easier for employees to eat well during the work day. Here is a summary of worksite food environment recommendations for obesity prevention, based on a review of expert guidance from the Centers for Disease Control and Prevention, the Institute of Medicine, the World Health Organization, and others. Create a worksite environment that promotes healthy eating 1 , 2 , 3 , 4 , 5 , 6 , 7. Implement formal worksite policies to promote healthy food and beverages or reduce less—healthy foods and beverages, such as 2 , 3 , 7 , Use marketing strategies to encourage healthier food and beverage choices or discourage unhealthy choices at the workplace. Promote breastfeeding or pumping, such as by setting up lactation rooms and giving female employees time to breastfeed or pump 3 , 4 , 5 , 13 , The CDC Guide to Strategies for Reducing the Consumption of Energy Dense Foods. Department of Health and Human Services, Centers for Disease Control and Prevention Institute of Medicine. Local government actions to prevent childhood obesity. Washington, D. The CDC Guide to Strategies for Reducing the Consumption of Sugar—Sweetened Beverages. Khan LK, Sobush K, Keener D, et al. Recommended community strategies and measurements to prevent obesity in the United States. Through Education, Support, Connections, and Advocacy. Become a part of the OAC Community today! The Obesity Action Coalition, OAC, is a national nonprofit organization dedicated to giving a voice to the millions of Americans affected by the disease of obesity and empowering them along their journey toward better health. Your support fuels our mission. When you participate, advocate and donate, you help us to create a better world for the more than 93 million Americans affected by the disease of obesity. With your help, we can continue to elevate and empower those affected by obesity through education, advocacy and support. Donate Today! More Ways to Give. Sign-up to stay connected to our mission, latest news, events, ways to get involved, information and all things OAC! Join the OAC! Corrigan McBride. In this episode of OAC Health Talks, bariatric surgeon Corrigan McBride, MD, DABOM, FACS, FASMBS, will discuss what makes a healthy romantic relationship and how bariatric surgery can affect relationships,. In this episode of OAC Health Talks, bariatric surgeon Corrigan McBride, MD, DABOM, FACS, FASMBS, will discuss what makes a healthy romantic relationship and how bariatric surgery can affect relationships, sexual function, and fertility. She will also give practical strategies you can take to build a support system. Thursday pm - pm GMT Calendar GoogleCal. Together, we can make a difference. Join us in supporting this important cause by raising awareness and taking OACAction! All Day Monday GMT Obesity Care Week is an annual public awareness event dedicated to raising awareness, educating and advocating for a better world for people living with obesity. Founded in ,. Founded in , Obesity Care Week has a global vision for a society that understands, respects and accepts the complexities of obesity and values science and clinically-based care. This year, Obesity Care Week will be held from March 4th — March 8th. Learn more at obesitycareweek. Your tax-deductible donation helps the OAC to raise awareness, advocate for improved access, provide evidence-based education, fight to eliminate weight bias and discrimination and elevate the conversation of weight and its impact on health. Check Out OAC's Resource Library! Access the Library. Tackling Obesity: A Conversation with Football Legends Dick and Matt Butkus We had the privilege of interviewing the NFL legend before his passing, during which he shared his passion for improving the lives of others and his compassion for his loved ones. |
| Prevention Strategies & Guidelines | Overweight & Obesity | CDC | Article CAS PubMed Google Scholar. Department of Health and Human Services interim public health recommendations, November Ogden CL, Carroll MD, Kit BK, Flegal KM. Rapid improvement of hepatic steatosis after initiation of leptin substitution in a leptin-deficient girl. Additionally, selective antagonists suitable for pharmacological use are seldom available to selectively silence a single mechanism of action to explore its relation to endogenous control of body weight, or to block the action of a specific drug or a single element in a multi-action peptide, such as the incretin co-agonists. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than persons. |
Ist Einverstanden, die sehr guten Informationen